A 59 year-old woman with a history of successfully treated Hepatitis-C, Systemic Lupus Erythematosus, and a remote history of melanoma of the scalp presented to our center for evaluation of abdominal pain, nausea, vomiting, and malaise. An outpatient CT scan revealed numerous cystic liver lesions. A liver ultrasound from one year prior to admission showed a mildly heterogeneous and echogenic liver texture with no observed masses or dilated ducts. Her genotype 1b Hepatitis-C virus had been successfully treated with Pegylated interferon, Ribavirin, and Telaprevir 9 months prior to presentation. A liver biopsy revealed stage I fibrosis 6 months prior to presentation.
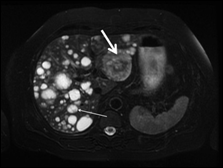
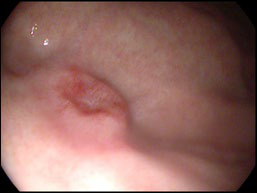
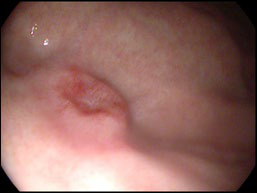
At our center, an abdominal MRI revealed greater than 50 hepatic cysts and cystic masses. A dominant 6 cm cystic mass in segment 2 was notable for peripheral enhancement and evidence of intralesional hemorrhage. A 2 cm complex appearing cystic mass was also noted at the junction of segments 6 and 7. No as cites or splenomegaly was observed (Figure 1). Further work-up with an EGD and liver FNA were performed. The EGD revealed an 8 mm ulcer in the gastric fundus (Figure 2) as well as multiple small nodules in the gastric body. Biopsies of the gastric ulcer and nodules were consistent with malignant melanoma.
Figure 1: Abdominal MRI showing numerous hepatic cysts and cystic masses. A 6 cm mass in segment 2 (thick white arrow) is remarkable for mild peripheral enhancement and intralesional hemorrhage. A 2 cm complex appearing cystic mass is noted at the junction of segments 6 and 7 (thin white arrow).
Figure 2: Endoscopic image of ulcer in the gastric fundus.
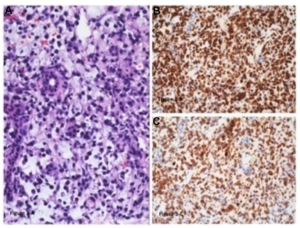
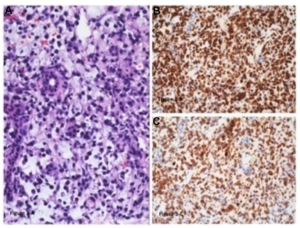
FNA of the 6 cm cystic hepatic mass showed small to intermediate sized epitheliod cells infiltrating and replacing the hepatic parenchyma on H&E stain (Figure 3A). HMB-45 (Figure3B) and Melan A (Figure 3C) immunohistochemical staining highlight melanocyte differentiation. Staining for S-100 was also positive. Analysis for BRAF mutation was negative.
Figure 3: Liver with metastatic melanoma. (A) Hepatic parenchyma replaced by melanoma – small, non pigmented, epithelioid cells with scant cytoplasm and hyperchromatic nuclei. (Hematoxylin-eosin, original magnification x200) (B) HMB45 immunohistochemical stain shows diffuse cytoplasmic staining in the tumor cells. (Original magnification x200) (C) Melan A/MART-1 immunohistochemical stain shows diffuse cytoplasmic staining in the tumor cells. (Original magnification x200).
Cystic hepatic metastases commonly occur due to necrosis and cystic degeneration of rapidly growing hypervascular tumors such as melanoma, sarcoma, carcinoid, neuroendocrine tumors, as well as some lung and breast tumors.1 Alternatively, some cystic metastases occur due to the cystic nature of the primary tumor (pancreatic or ovarian cystadenocarcinomas).2 Melanoma accounts for nearly 5% of new cancer diagnoses yearly; 4% of which are metastatic at the time of diagnosis.3 Liver involvement is seen in as many as 50% of metastatic cases. The 10-year survival rate for patients with metastatic melanoma is less than 10%.4
Radiologic characterization of liver metastases is often performed with magnetic resonance imaging. Non-contrast imaging typically reveal lesions with a cystic appearance due to liquefactive necrosis. Hyper-intense appearance on T1 images is often noted due to paramagnetic substances such as melanin and extracellular haemoglobin. Contrast enhanced imaging is notable for the presence of hyper-vascular lesions.5 Diagnosis of liver metastases is made by pathology on liver biopsy. Positive IHC staining for Melan A, HMB-45 and S-100 constitute the classic immuno-profile for melanoma.
Some patients with limited disease burden may be candidates for surgical metastasectomy. Medical therapy in advanced melanoma is focused on the use of immunotherapy such as interleukin-2 or the anti-CTL antigen-4 monoclonal antibody, Ipilimumab. Patients with BRAF mutations may be candidates for additional targeted therapies such as BRAF inhibitors (eg, Vemurafenib or Dabrafenib) and/or MEK inhibitors (eg, Trametinib).6
Our patient was started on Ipilimumab as palliative therapy. This case highlights a difficult diagnosis in the setting of complex liver cystic masses – an assessment of previous history and repeated biopsies are often needed to clinch the diagnosis.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest to report with respect to the content of this article.
ACKNOWLEDGEMENTS
Speaker’s Bureau/Advisor/Consultant: Gilead Sciences, BMS, Janssen, Abbvie, Salix, Onyx, Genentech.
Research Grants: Gilead, BMS, Abbvie, Salix, Vertex, Santaris, Bioalliance, Vital Therapies, ISIS, Merc.