INTRODUCTION
Variceal bleeding is the final outcome of many events that start with increase of portal blood pressure, development of varices and their progressive dilatation up to their rupture and bleeding.
Variceal bleeding mostly occurs as a result of portal hypertension within liver cirrhosis, and it can occur from oesophageal varices, gastric varices or ectopic varices along digestive tract.
Left-sided portal hypertension (LSPH) is a rare form of portal hypertension that usually occurs as a result of isolated obstruction and thrombosis of the splenic vein, and it can cause bleeding from isolated gastric varices.
LSPH should be considered in all cases of gastrointestinal bleeding accompanied by normal liver function, splenomegaly and passable portal vein.
In this paper we present a case of a male patient with history of chronic pancreatitis that was presented by abundant bleeding from upper gastrointestinal tract caused by LSPH due to splenic vein thrombosis.
CASE REPORT
In October 2007, a 45-years-old male patient was admitted to gastrointestinal department because of the bleeding from upper GI tract which presented with abundant hematemesis and clinical signs of hemorrhagic shock.
In patient’s history it is important to highlight alcohol consumption for many years. First time he was hospitalized in 1993 because of acute pancreatitis caused by alcohol, and several next year’s he was hospitalized because of repetitive chronic pancreatitis exacerbations.
Six years after the first hospitalization complete diagnostic work up was done and abdominal ultrasound showed enlarged spleen with many perisplenic collaterals and suspicion on splenic vein thrombosis was set. During the same hospitalization patient develops clinical signs of acute abdomen and small intestinal obstruction and was transferred to surgical department.
Explorative laparotomy revealed numerous, tight small bowel adhesions so adhesiolysis was performed. During repeated hospitalization in March 2003 upper endoscopy showed emphasised and voluminous folds of gastric large curve that were suspected to be isolated varices.
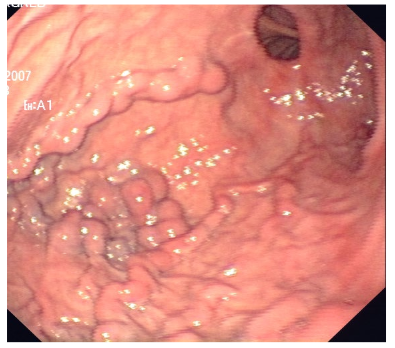
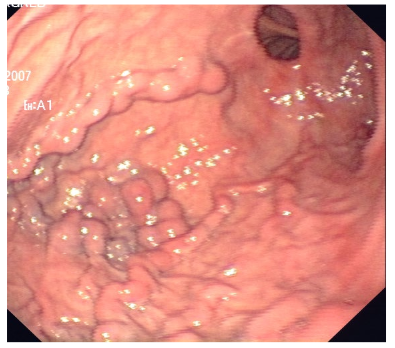
Transabdominal ultrasound with Doppler could not show vascular structures due to meteorism. Endoscopic ultrasound with Doppler of gastric fundus confirmed existence of isolated gastric varices. Multi Slice Computer Tomography (MSCT) with contrast visualized extremly enlarged spleen (8 cm x 15 cm x 19 cm) and numerous convolution of wide veins with diameter up to 2 cm which led from spleen to stomach, up to oesophagus and peripancreatically. Splenic vein did not fill in with contrast so it was concluded that splenic vein thrombosis occurred. Patient missed his control follow up for few years, and then in April 2007 he was again admitted in emergency room because of obstructive symptoms- recurrent vomiting and inability to eat. Endoscopically and radiologically fixed bulbostenosis was confirmed, next to early known gastric varices. Emergency surgical treatment was indicated so antecolic gastroenetroanastomosis with entero-enteroanastomosis section Braun was done. Surgical procedure was complicated due to numerous fibrous adhesions and that is the reason why splenectomy did not take place. (Figure 1)
Figure 1: Upper gastrointestinal endoscopy. Isolated varices on the greater curvature of the stomach.
At admission in October 2007 the patient was extremly pallor, with cold periphery, tachycardia and very low blood pressure. Laboratory findings showed significant posthemorrhagic anaemia: erythrocytes 2.19×10¹²/L (4,34-5,72×10¹²/L), haemoglobin 55 g/L (138-175 g/L), haematocrit 0.173 L/L (0,415-0.530 L/L), MCV 89.2 fL (83.0-97.2 fL), Prothrombic time (PV) 0.15 (0.70-1.30), thrombocytes 205×109/L (158-424×109/L). After patient was stabilized receiving crystalloid fluids, transfusion of concentrated erythrocytes and fresh frozed plasma emergency oesophagogastroduodenoscopy was performed. In oesophagus and stomach there was fresh blood and in stomach big coagulum that was not able to be removed completely but huge gastric varices were seen beneath. Due to significant varices and acute bleeding endoscopic haemostasis could not be performed. Control gastroscopy after emptying blood from stomach showed enlarged varices on major gastric curve.
As endoscopic haemostasis was not able and risk of repetitive bleeding very high, consultation between gastroenterologist, surgeon, and intervent radiologist concluded that therapeutic method of choice was transcatheter embolization of splenic artery due to high risk of operation.
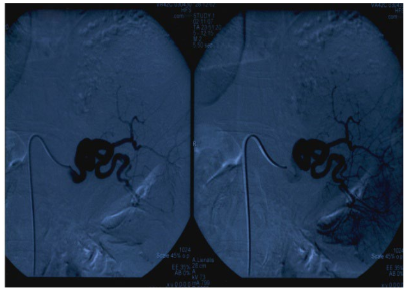
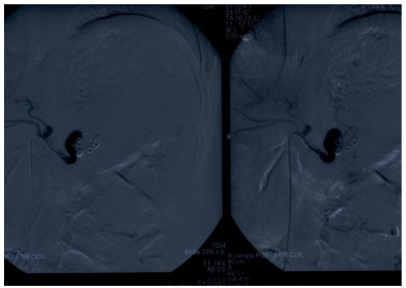
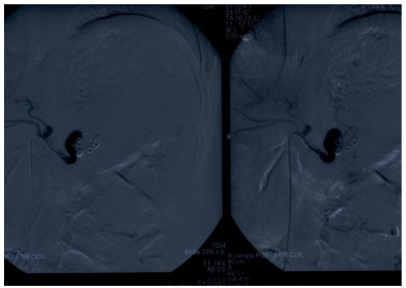
Three days after admission to hospital digital subtraction angiography of abdominal aorta was performed to demonstrate beginning of coeliac truncus and splenic artery. During procedure coeliac truncus was selectively catheterized and catheter was placed in main tree of splenic artery all the way to its distal segment. Within splenic hilus significant curve of splenic artery was visualized. (Figure 2). The main tree of splenic artery was embolized by serial of spirals whose diameter was from 5 to 8 mm, and the goal was devascularization and development of collateral blood path to stop necrosis upgrowth. Control angiography did not show flow within main tree of splenic artery, so the goal of intervention was achieved. (Figure 3)
Figure 2: DSA of abdominal aorta. Tortuotic lienal artery filled with contrast before embolization procedure.
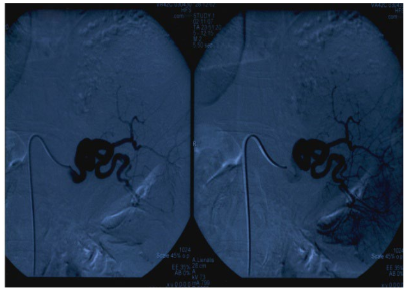
Figure 3: DSA of abdominal aorta. Lienal artery after DSA embolization with a series of coils 5-8 mm. There is no sign of flow inside lienal artery.
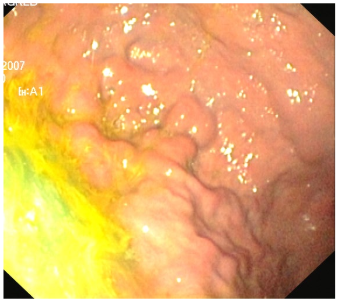
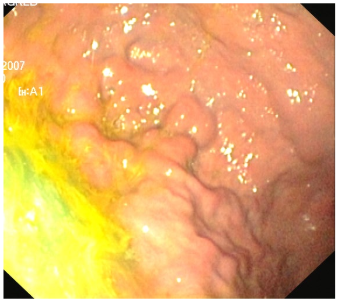
Procedure finished without complications, and during follow up there were no signs of sepsis or splenic abscess. Few days after procedure patient’s condition improved. Fifteen days after transcatheter embolization control oesophagogastroduodenoscopy showed significant reduction of varices on major gastric curve (Figure 4). Control MSCT showed ischaemic splenic upper half and reduced gastric varices. During 3 years of follow up there was not recurrent bleeding from gastric varices.
Figure 4: Upper gastrointestinal endoscopy. Significantly reduced gastric varices after embolization of the lienal artery.
DISCUSSION
We presented a case of a 45-years-old male patient with recurrent bleeding from gastric varices caused by a rare form of portal hypertension.
Left-sided portal hypertension (LSPH) represents localized form of portal hypertension which originates as a result of isolated splenic vein obstruction, mostly connected with thrombosis (Splenic Vein Thrombosis-SVT).1 Because of their anatomical relation every pancreatic condition can effect splenic vein.2,3 Acute and chronic pancreatitis and pancreatic tumors are main causes of SVT.2,4 Exact mechanism of thrombosis development is obviously multifactorial and includes intrinsic injury of endotel with inflammatory and neoplastic process and extrinsic damage connected with venous compression from outside due to fibrosis, pseudocyst that lies next to vein or adjacent oedema.
LSPH is a rare cause of upper GI tract bleeding. Obstruction of splenic vein results with vein hypertension in collateral flows of vv.gastricas breves, vv.coronariae ventriculi, vv.gastroepiploice and veins of upper part of stomach. Usually after obstruction splenic blood goes through vv.gastricae breves to gastric vein plexus. As pressure and flow in those structures grow, dilatation of submucous veins occurs and gastric varices develop. As most of the patients have no symptoms it is very hard to predict accurate incidence of this disorder. But percentage of LSPH in all patients with portal hypertension is less than 5.3 First clinical manifestation of splenic vein thrombosis and left-sided portal hypertension is mostly acute or chronic bleeding from oesophageal or gastric varices.5 Splenomegaly is one of the major characteristics of long lasting portal hypertension, and in LSPH splenomegaly is more expressed than in liver cirrhosis.6
In our paper we presented a case of a male patient with history of repetitive chronic pancreatitis exacerbations due to aethylic etiology. With continuous, long lasting alcohol consumption he developed chronic pancreatitis and consequently by repetitive exacerbations he developed fixed bulbostenosis and gastric varices due to splenic vein thrombosis. The diagnosis of gastric varices was established endoscopically four years after first, clinically proven bleeding. At that time he presented with abundant bleeding from big, isolated gastric varices and clinical signs of hemorrhagic shock.
The diagnosis of gastric varices is made from clinical status, endocopically and radiologically. Upper endoscopy is a procedure of choice for visualization of gastric varices, especially when performed by experienced doctor. New studies that compare splenoportography and endoscopy reveal that even 90% of gastric varices are able to be diagnosed endoscopically.7
Finding of isolated gastric varices during upper endoscopy always require work-up to find if possibly splenic vein thrombosis exists. Generally ultrasound with Doppler is the first method to be done in patients with portal hypertension.8 According to limitations of this method (interpretation due to operator, bad acustic window), when SVT is suspected it is often necessary to do an extra view angiographically. As splenoportography and digital subtractial angiography are invasive methods, to show porto-lienal vascular system today we use non invasive methods as MSCT and MR angiography. Between MSCT and MR angiography, the last one is more reliable for visualization of porto-lienal vascular system in relation to Doppler ultrasound and MSCT.9 Endoscopic ultrasound is sensitive method to show small pancreatic lesions, chronic pancreatitis, changes in vascular structure and oesophagus and gastric varices.10
LSPH is one of the therapy accessible disorders caused by portal hypertension.11 As it is localised form of portal hypertension, therapy needs to be directed to splenic side of portal circulation as hypertension is expressed in that pool. The method of choice in treating patients with LSPH and bleeding is splenectomy due to high mortality and risk of re-bleeding.12 Removal of spleen decreases vein flow through collateral circulation, shrinks varices and prevents re-bleeding. In patients who did not manifest with bleeding, routine splenectomy is not method of choice because of low risk of bleeding. In patients who are not candidates for surgery, transcatheter embolization of splenic vein can be performed.13
During this procedure spirals or other agents (antilogous thromb or gelatinous mass) are transcatheterically put into splenic artery which will lead to artery embolization. In 25% of patients who underwent embolization of splenic artery development of septic complications around spleen is possible, especially development of splenic abscess. In those cases splenectomy needs to be performed.14 Recurrent bleeding after transarterial catheterization is not common, and prognosis of patients mostly depends on aethyiology of disorder.
Embolization of the splenic artery has been shown as an alternative method which has the same effects as a splenectomy, moreover, it can avoid some severe complications such as post-splenectomy sepsis, or uncontrolled increase of platelet count because of the residual noninfarcted spleen. Koconis, et al.15 reported that partial splenic embolization made efficacious improvements on the bleeding and hematologic parameters for partial hypertension patients, and the associated morbidity and mortality were acceptable.16
Because of extensive fibrous adhesions in abdomen, especially around spleen and pancreas, gastroenterologist, surgeon and radiologist concluded that in case of our patient there is significant risk of surgical procedure. So transcatheter embolization of the splenic artery was undertaken as the method of “non-surgical splenectomy”. The procedure underwent without complications, and during follow up there was no recurrent bleeding from gastric varices.
The case we presented indicates a rare cause of segmental portal hypertension. Splenic vein thrombosis, which is usually connected with pancreatic disorders (tumor, inflammation) is cause of Left-sided portal hypertension (LSPH). It should always be considered in patients with normal liver function and obscure splenomegaly, and in patients with isolated gastric varices.17 Therapy of choice in patients with bleeding is splenectomy, and in patients with high surgical risk transcatheter embolization of the splenic vein. In asymptomatic patients there is no consensus about therapeutic approach.
DISCLOSURES
All authors listed have contributed sufficiently to the project to be included as authors, and all those who are qualified to be authors are listed in the author byline. To the best of our knowledge, no conflict of interest, financial or other, exists.