Incidental durotomy (ID) is a term used to describe unintentional opening of the dura mater during spinal surgery. Although, commonly referred to as dural tear; most recent scholars are circumventing the use of the latter term, as it could imply an element of carelessness when none were necessarily present. Therefore, ID, unintended durotomy, unintentional durotomy or simply just dural opening, have been recommended to replace the term dural tear.1,2
The reported incidence of ID of spinal surgeries ranges from 0.1-13.7%. Despite being one of the most common complications of spinal surgery, it remains often underreported because of the lack of morbidity in the most of cases.3 ID is often associated with cerebrospinal fluid (CSF) leakage from the subarachnoid space through the dural defect.1
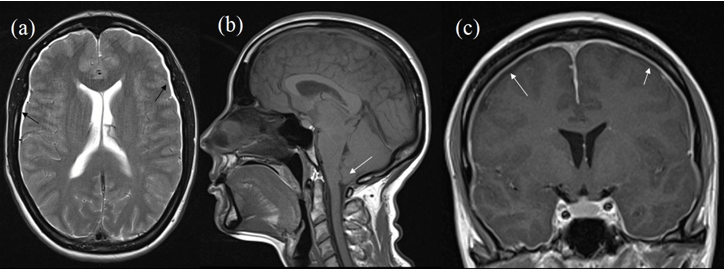
CSF leakage can lead to several complications resulting from loss of CSF volume (decreasing the brain’s supportive cushion), which can lead to symptoms of intracranial hypotension (presenting with nausea, vomiting, postural headache, tinnitus, vertigo, etc) (Figure 1). It can also lead to more serious yet less common complications such as CSF fistula formations, and meningitis.4 Since some of the aforementioned symptoms are improved in the recumbent position, patients are often advised to remain flat in bed for a period of time (ranging from 1-10 days) after the spine surgery.4 Previous studies showed that bed rest without intervention is ineffective in treating an accidental durotomy.5 However, following dural repair the need for flat bed rest is still an area of ongoing debate.6
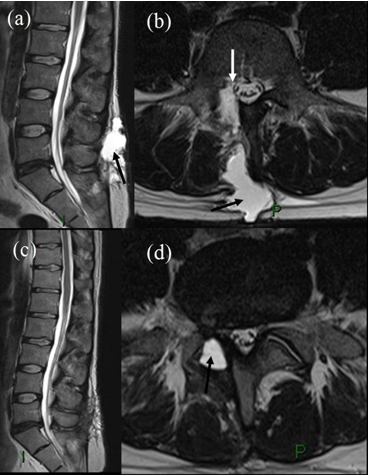
Figure 1: Low Intracranial Pressure Following CSF Leak
T2 Axial (a) Shows Thin Subdural Fluid Collection (Black Arrows). (b) T1 Sagittal Shows Sagging of Brainstem and Cerebellar tonsillar Descent (White Arrow). (c) T1 Coronal Post-Contrast Shows Diffuse Pachymeningeal Enhancement (White Arrows).
Currently, there is no concrete evidence to support the beneficial effects of flat bed rest following ID nor there a consensus about the period of this bed rest. Therefore, post-operative instructions for patients with ID remain controversial and rely heavily on the previous experience/preference of the treating surgeon(s).5
This debatable topic was first addressed by Hodges et al6 who conducted a retrospective review of 20 patients with ID and resultant CSF leakage treated without mandatory bed rest following the dural repair. In 19 cases the CSF leakage was detected and repaired (with non-absorbable stiches and fibrin glue) during the initial procedure, and in 1 patient the defect was repaired 2 weeks after the surgery. All 20 patients had their symptoms monitored for 1 week, and delayed follow-up at a minimum of 10 months took place. During a week from surgery only 2 patients (10%) reported headache, 2 patients (10%) reported nausea, and 1 patient (5%) reported tinnitus.6 Worth mentioning; similar symptoms were reported in patients treated with bed rest following ID and CSF leak.1 The study concluded that 75% of the patients had no symptoms related to the ID despite being mobilised immediately post-operative.6
In 2013 Low et al7 addressed the same topic, through a retrospective study. They looked at a year data of a single centre for all patients who incurred an accidental durotomy and were repaired intraoperatively.7 Their notes were reviewed for evidence of complications for a minimum of 12 months after surgery. Out of 889 patients who had lumbar surgery 61 patients (6.8%) had ID and CSF leak. Twenty six patients were mobilised immediately following surgery, 9 patients were mobilised after 48 hours and 26 patients were prescribed flat bed rest for 72 hours or more. The review concluded that there was no statistical significance between the day of mobilisation and the rate of complication. Similar results were reproduced by other study promoting early mobilisation.8
Bonanos et al9 prospectively audited flat bed rest for managing ID in lumbar spine surgery over a period of 6 months. The study showed that flat bed rest was used in 20 patients with ID for an average of 4 days ranged from 1-10 days. They concluded that flat bed rest does not reduce morbidity following ID, and in fact was deemed unnecessary.9
A German national survey looking at the intra- and post-operative management of accidental durotomy in lumbar spine surgery, showed no consensus concerning the management. The survey however, concluded that despite not being proved to reduce the rate of cerebrospinal fluid fistulas, bed rest is still frequently used. While period of flat bed rest prolongs the hospital stay with additional costs and potentially higher rate of medical complications, the survey warranted a multicentre trial to address the topic.10 Another survey looking at 3 nations (German, Swiss, and Austrian) practice regarding the management of ID, revealed once more the substantial heterogeneity in the management. Nonetheless; there is a trend towards early mobilisation if the ID has been closed sufficiently with no participant favouring bed rest for more than 72 hours.11
One study compared rates of complications between patients who undergo flat bed rest (for over 24 hours) following ID to those allowed to mobilize early (within the first 24 hours post-operative ).12 The study concluded that there was no statistically significant difference between both groups in regards to post-durotomy related neurological complications, wound complications and need for revision surgery. However, there was a statistically significant decrease in the incidence of total medical complications in the early mobilized group (0% vs. 50%, p=0.0003).12
In our own practice, we have not done a full fledged study on the management of CSF leak following ID. However, Intra-operatively and more often on imaging, it is possible to clearly localise the site of intradural communication. We have practised open repair, lumbar drain insertion and lately injection of dural sealing agents with very good results. Prescription of flat bed rest remains controversial in our local practice. Nonetheless the senior author encourages early mobilisation for all his patients following satisfactory repair of the durotomy; with increasingly encouraging results for early mobilisation, other consultants in the department have started adopting early mobilisation approach for their patients.
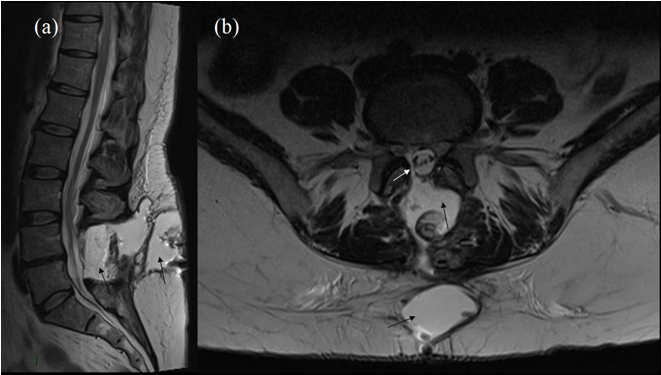
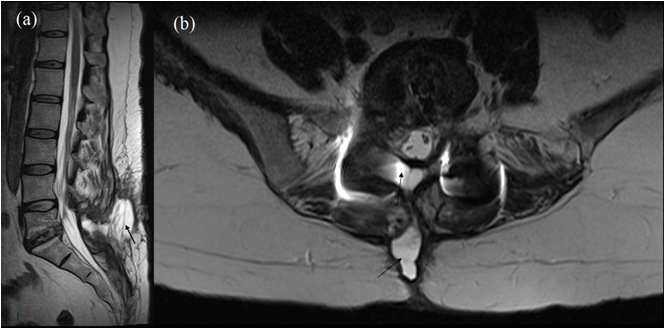
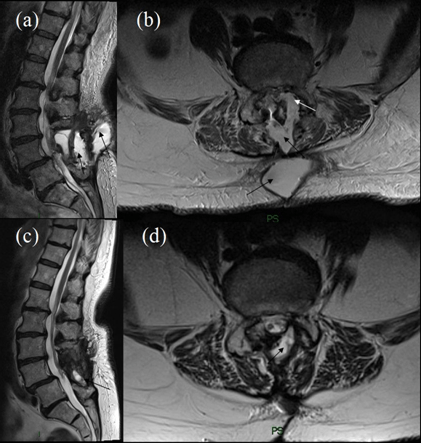
Some examples from our own practice are included here. Figure 2 shows a patient who was treated with lumbar drain and flat bed rest, following which the patient improved and returned to normal. Figure 3 shows a patient with ID, treated with open repair and flat bed rest, with good outcome. Even prominent collections managed with dural sealing agent; have been successfully treated without flat bed rest (Figure 4). However, we do come across occasional patients who have had unfavourable outcome with persistent symptoms despite open repair and bed rest, we have successfully treated such patients with glue injection, it is often important to localise the site of communication in such patients (Figure 5).
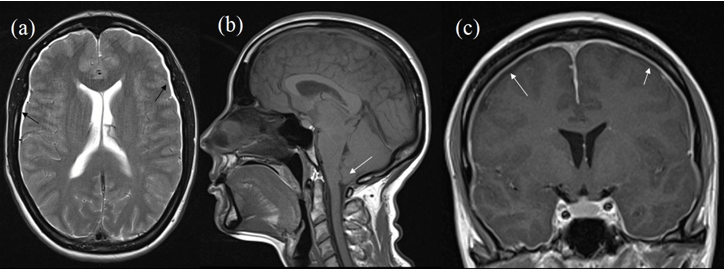
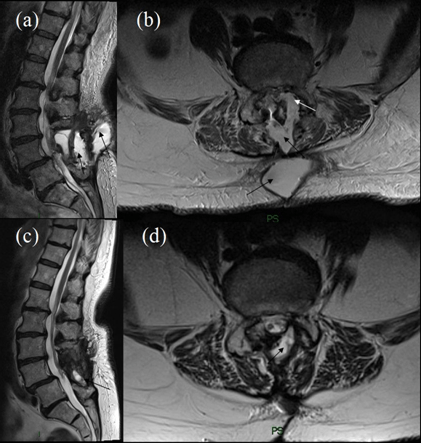
Figure 2: CSF Leak Following ID.
T2 Sagittal (a) and Axial (b) Images Showing a Prominent CSF/Fluid Collection (Black Arrows) Following ID. White Arrow in (b) Shows the Site of Dural Communication, Leading to the Fluid Collection. Patient has been Treated with Lumbar Drain and Flat Bed Rest with Good Outcome.
Figure 3: CSF Leak Following ID.
T2 Sagittal (a) and Axial (b) Images Showing a Prominent CSF/Fluid Collection (Black Arrows) Following ID. The Site of Communication Not Clearly Identified. Patient was Treated with Open Repair and Flat Bed Rest with Good Outcome.
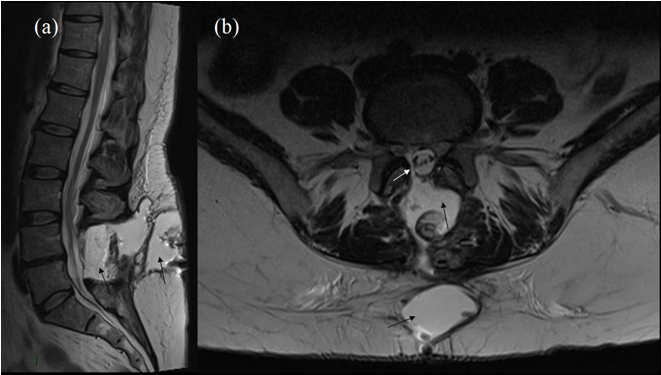
Figure 4: CSF Leak Following ID
T2 Sagittal (a) and Axial (b) Images (Above) Showing a Prominent CSF/Fluid Collection (Black Arrows) Following ID. The Site of Intradural Communication is Marked by White Arrow. Patient was Treated with Dural Sealant but Without Flat Bed Rest with Good Outcome. Follow-up T2 Sagittal (c) and Axial (d) Images (below) Showing Significantly Reduced CSF Collection (Black Arrows in c and d).
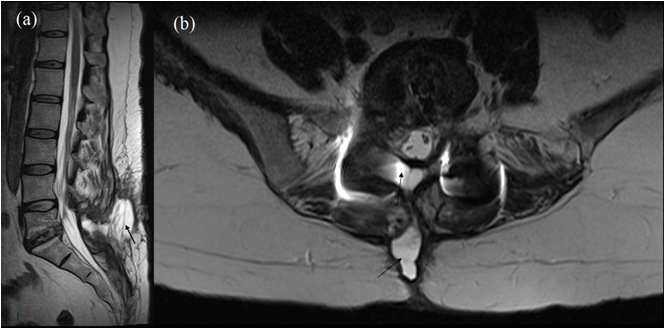
Figure 5: CSF Leak Following ID.
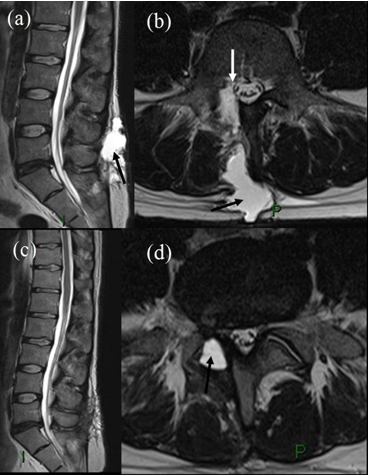
T2 Sagittal (a) Axial (b) Images (Above) Showing a Large CSF Collection (Black arrows). Site of Communication Shown by White Arrow in (b). Initially Patient had an Unsatisfactory Outcome Following Conservative Treatment. Subsequently Treated with Glue Injection. T2 Sagittal (c) and Axial (d) Images (Below) Showing Significantly Reduced Collection (Black Arrow in d) Following Glue Injection.
CONCLUSION
Despite the fact that a period of flat bed rest following ID and CSF leak is commonly advised, it is by no means accepted as a standard practice. Although, there is a clear need for first class evidence to address the topic; yet, the current available evidence supports early mobilisation following sufficient dural repair. We understand the difficulties in running such trial as standardizing the size and site of the durotomy, the underlying spinal pathology, patients’ comorbidities/healing potentials, and closure techniques might be challenging to say the least.
Different methods for achieving satisfactory dural closure exist, with promising results of the advancing technology for dural sealing agents especially for durotomies where primary suturing is not thought to be feasible or technically possible without significant collateral damage.
Long periods of flat bed rest does not decrease the rate of complications, in fact early patients mobilisation potentially reduces the length of hospital stay, medical complications and the overall cost on the health system.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.