INTRODUCTION
Double J (DJ) stenting is a routine procedure in urological practice. Possible complications of DJ stents include encrustation, fragmentation, migration, malposition, stenturia, stent fracture, forgotten stent, urinary tract infection (UTI) and severe lower urinary tract symptoms (LUTS).1 We report a rare case where the proximal coil of a DJ stent was malpositioned in the second part of the duodenum, diagnosed on imaging and confirmed by upper GI endoscopy, in a patient with chronic right flank pain who underwent emergency right DJ stenting elsewhere and who visited us 3-months later for further management.
CASE REPORT
We present a case of 59-year-old man known to be diabetic and hypertensive who presented with dull, intermittent right flank pain for the past 3-months. This was associated with mild dysuria, no hematuria and occasional low grade fever.
On enquiring further history we found that 3-months ago, he underwent right DJ stenting as an emergency procedure elsewhere. Upon checking his medical records, a complicated obstructive uropathy on the right side was suggested by a computerized tomography (CT) scan which reported a small hydronephrotic right kidney. There was a retroperitoneal (RP) mass at the L1 level just inferior to the head of the pancreas behind the D3-D4 segment of the duodenum. The right upper and mid ureter were involved by the RP mass. A CT guided fine needle aspiration of the retroperitoneal mass was performed which revealed acute suppurative inflammation. Blood tests showed a serum creatinine of 1.4 mg/dL (123.79 umol/L) and slight elevation of WBC counts to 16,000 cells/mm3. In view of the above mentioned parameters he underwent emergency right DJ stenting but without intra- and post-operative imaging at the host institution. Following this there was normalization of blood test parameters and the serum creatinine settled to 1mg/dl (88.42 umol/L). Long-term antibiotics were prescribed because of suspected super infection and the cytology report showing acute suppurative inflammation.
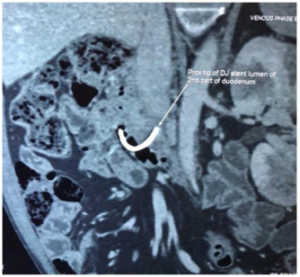
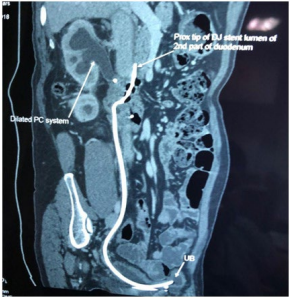
He then presented to our outpatient clinic with chronic dull right flank pain for evaluation and for right DJ stent removal. Blood test analysis showed that the serum creatinine was 1.4 mg/ dL (123.79 umol/L) with normal WBC count. An abdominal CT was performed which revealed a malpositioned right DJ stent with the tip of the proximal coil in the second part of duodenum (Figure 1), and the distal tip in urinary bladder. The right kidney showed evidence of hydronephrosis (Figure 2). There was no evidence of the previously seen RP mass (suggesting that it had resolved on previous long-term antibiotics). The excretory phase showed a shrunken, poorly functioning right kidney (Figure 3).
Figure 1. Proximal Tip of DJ Stent Seen in the Lumen of the Second Part of Duodenum
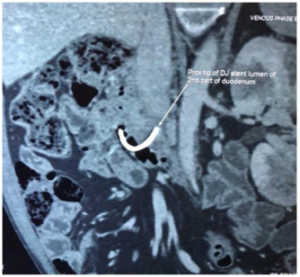
Figure 2. 320 Slice CECT Abdomen Showing a Right Small Hydronephrotic Kidney, the Upper Part of the DJ Stent Uncoiled and Malpositioned into Duodenum while the Rest of the Stent was Properly Positioned
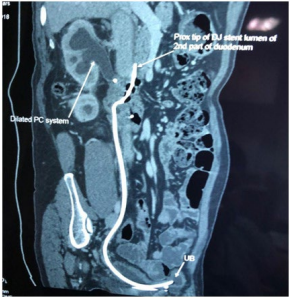
Figure 3. Contracted Right Poorly Functioning Kidney with Uncoiled Proximal DJ Stent Coil

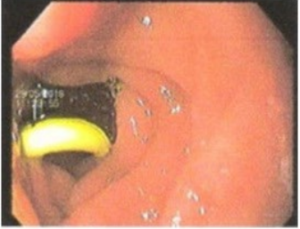
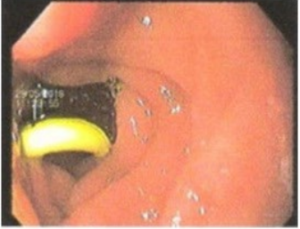
We consulted with the Gastroenterology Department and upper GI endoscopy showed the upper coil of the DJ stent in the second part of duodenum (Figure 4), confirming the CT findings. A renogram was performed which revealed 8% right split renal function. With these findings a laparoscopic right nephrectomy with right DJ stent removal was planned.
Figure 4. Upper GI Endoscopy Confirming DJ Stent Tip in Second Part of the Duodenum
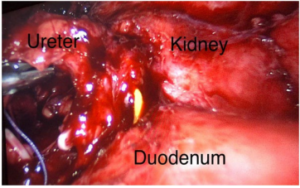
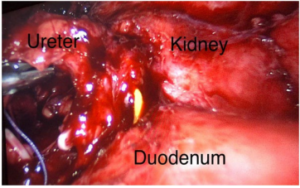
Under general anaesthesia, in the left lateral decubitus position, peumoperitoneum was created using a Veress needle and standard laparoscopic ports placement done. The right colon was mobilised and dropped down, with great difficulty the right ureter was identified amidst dense adhesions (presumably due to the previous retroperitoneal inflammatory mass). The duodenum was found stuck to the right renal pelvis and the upper ureter and was mobilized by further gentle dissection. During these maneuvers, the DJ stent entering into duodenum suddenly appeared through a very tiny orifice (Figure 5). The upper coil was extracted from the duodenum and the entire stent was removed from the ureter and retrieved through one of the ports. The duodenum was then inspected, revealing a very small opening without leakage of intestinal material. The defect was closed with two interrupted 2-0 vicryl sutures and reinforced with an omental patch. Subsequently, right nephrectomy was performed, and the specimen retrieved though extension of one of the port site in right iliac fossa. A drain was placed and the abdominal opening and port sites were closed.
Figure 5. Intra OP Picture Showing Proximal Part of DJ Stent Entering into the Duodenum from the Upper Ureter, Observed while Mobilising the Duodenum from the Renal Pelvis and Upper Ureter
The peri-operative period was uneventful. After a nil by mouth regime with continuous Ryles tube drainage for 3-days the patient was started on oral liquids. The drain was removed on the 5th post-operative day and the patient was discharged on a soft diet. Blood test showed that the serum creatinine had reduced to to 1.1 mg/dL (97.26 umol/L) from 1.4 mg/dL (123.79 umol/L). The histopathology report was suggestive of chronic pyelonephritis. He visited the out-patient clinic where he was noted to be asymptomatic and further followed-up at 3, 6, 12, 24-months with no complications to date.
DISCUSSION
Malposition of a stent is defined as an incorrect position relative to the initial or planned placement.2 Sometimes guidewires and stents made of stiffer materials may penetrate the ureter, collecting system, and kidney parenchyma during placement, resulting in urinomas or hematoma formation. In our case, the presence of an ongoing inflammatory process in the retroperitoneum close to the upper end of the ureter and around the duodenum, the guidewire might have perforated the upper ureter and entered into the duodenum. Railroading a DJ stent over such a guidewire would then lead to malposition of the upper coil of the DJ stent into the duodenum. In these cases while inserting the guidewire there might be little or no resistance felt but there is still a chance of ureteric wall perforation. Intra-operative imaging helps to prevent this complication.
Laparoscopy is of great help particularly in this type of case with dense adhesions as gentle dissection can be performed under direct vision enabling stent removal and complete nephrectomy. Management of such cases depends on the renal function. With normal renal function, cystoscopic DJ stent removal or correct repositioning can be performed with close observation and monitoring for bile in the urine. After DJ stent removal if a uroenteric fistula is evident this may need uretero-ureterostomy or pyelo-ureterostomy, excision of fistulous tract and reconstructive repair of the duodenum as appropriate. If ipsilateral renal function is poor, nephrectomy will be required as in this case.3
CONCLUSION
Insertion of a DJ stent though a common urologic procedure should be performed carefully to avoid complications. The surgeon should be aware of all possible complications beforehand and have a high-level of suspicion if there are any intra- or post-operative problems. If such complication arise they need to be dealt with early.
Malposition of a DJ stent may happen in situations where there is inflammation of the renal pelvis which may allow the guidewire to perforate these structures during insertion creating a false passage leading to faulty placement of DJ stent.
Blind DJ stent insertion should be avoided especially in acute or inflammatory conditions. This complication can be avoided by stenting under guidance with an image intensifier preferably with a retrograde pyelogram (RGP) and by deploying a guidewire under vision using a ureteroscope. Salazar pointed out that an X-ray done post insertion of a stent is important to confirm correct placement of the stent4 if this has not already been done intra-operatively. Early detection and replacement of a misplaced stent under fluoroscopic guidance is an important step in the management.5
FUNDING
None.
CONSENT
Informed consent has been taken from the patient for this study.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.