Clinicians are always in search of a less invasive method of diagnosing and assessing a patient. Patients with liver cirrhosis are no exception. Liver cirrhosis is the end stage of many liver pathologies and knowledge of the onset and stage of liver cirrhosis is important to the clinician as it dictates the treatments on offer. This has become increasingly important in viral hepatitis, as it determines level and timing of anti-viral therapy. Furthermore, onset of cirrhosis would alert the physician to screen for varices and hepatocellular carcinoma. To date the gold standard for diagnosing and staging liver cirrhosis is percutaneous liver biopsy. This is expensive and carries a significant complication rate and a small mortality rate. There could also be sampling error and it only shows if the area targeted has the cirrhotic changes, and does not give the picture of the entire liver. There have been attempts at non-invasive tests like the Fibrotest and ultrasound based elastography. There are at least two methods of ultrasound based elastography. Deformation elastography depends on the constant pressure/stress applied to the organ and shear wave elastography in which a shear wave is applied and propagation measured. These measures are at best qualitative and has a disadvantage of being operator dependent and subjects who have small livers or prominent fat cover may be difficult to assess.1
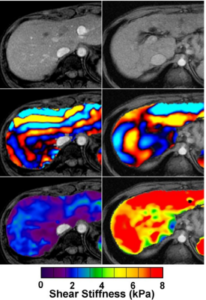
Magnetic Resonance Elastography (MRE) was first described in 1995. Since then the technique has been refined and applied to the liver. The technique uses propagating mechanical shear waves. The waves propagate more quickly in stiffer tissue. Wave propagation depends on wavelength, so the stiffer the tissue, the lower frequency (longer wavelength) is required to propagate the wave a given distance. A wave generator is applied to the liver at a frequency range of between 20-200 Hz. Imaging is done in one or more breathe holds and wave images taken. Special software generates elastograms that quantitatively display the tissue stiffness which can be displayed numerically or as colour-coded overlay on the Magnetic Resonance Imaging (MRI) images. (Figure 1)
Figure1: Normal liver is pictured on the left and the cirrhotic liver on the right. The top image is the MRI scan, the second row show the shear wave signal and the third, the integrated shear stiffness in kPa, colour coded as shown.
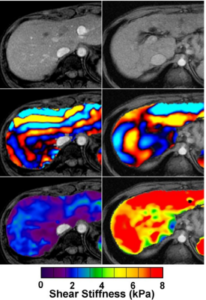
These images have proved valuable to the clinician. They tell the clinician of the stiffness and by implication degree of cirrhosis but more than that they show whereabouts the stiffness is. Biopsy samples only capture the histology of the targeted area and are open to sampling variability. MRI elastography gives the whole picture of what the liver is like.
Two recent papers have demonstrated the superiority of MRI elastography over fibrotest and ultrasound based elastography for non-alcoholic fatty liver disease and for all liver diseases including viral hepatitis.2,3 To date, staging of liver fribrosis/cirrhosis is based on histology. The reproducibility of MRI elastography may sway clinicians to use this in the future as a measure of liver stiffness rather than the more invasive and hazardous method of tissue sampling.
In the first paper, Singh, et al. performed a meta-analysis of data from 12 retrospective studies, comprising 697 patients who had both MRE and liver biopsies performed. 47.1% were with hepatitis C. Overall, 19.5%, 19.4%, 15.5%, 15.9%, and 29.7% patients had stage 0, 1, 2, 3, and 4 fibrosis, respectively. The overall rate of failure of MRE was 4.3%. Based on a pooled analysis of data from individual participants, MRE was shown to have a high accuracy for the diagnosis of significant or advanced fibrosis and cirrhosis, independent of Body Mass Index (BMI) and etiology of Chronic Liver Disease (CLD).2
In the second study, Cui, et al. compared the diagnostic utility of 2D-MRE against that of eight Clinical Prediction Rules (CPRs) (AST:ALT ratio, APRI, BARD, FIB-4, NAFLD Fibrosis Score, Bonacini Cirrhosis Discriminant Score, Lok Index and NASH CRN model) for predicting advanced fibrosis in a prospective cohort with paired liver biopsy as the gold standard. A prospective study of 102 patients (58.8% women) with biopsy-proven NAFLD, 2D-MRE and clinical research assessment within 90 days of biopsy. Receiver operating characteristic (ROC) analysis was performed to assess the performance of 2D-MRE and CPRs for predicting advanced fibrosis. In head-to-head comparisons using the DeLong test, 2D-MRE had significantly better AUROC (P<0.05) than each CPR for predicting advanced fibrosis. They concluded that compared to clinical prediction rules, 2D-MRE provides significantly higher accuracy for the diagnosis of advanced fibrosis in NAFLD.3
Are there drawbacks? It may be perceived as expensive but it is likely to be cheaper than histology. The additional equipment of the wave generator is perhaps the only other outlay if the MRI is already available in the institution. This new modality and how best to use it is still being explored and as it becomes increasingly used by mainstream hepatologists it is likely to be an important tool to the clinician.