INTRODUCTION
Paraganglioma (PG) is a type of neuroendocrine tumor that originates from chromaffin cells of the autonomic nervous system. These tumors can occur at various sites along the sympathetic and parasympathetic chains. While paragangliomas are related to pheochromocytomas (PCC), which are specifically adrenal gland tumors, they are not the same. Pheochromocytomas are a subset of paragangliomas that occur within the adrenal gland; hence, they are sometimes referred to as intra-adrenal paragangliomas. In contrast, paragangliomas occurring outside the adrenal gland are often referred to as extra-adrenal pheochromocytomas, though this term can be misleading. The incidence of paragangliomas in the general population is rare, ranging from 0.005-0.1%.1 Contrary to the original statement, the majority of paragangliomas (approximately 80-85%) are non-functional and do not produce excess catecholamines. When they do secrete these hormones, symptoms can be similar to those of pheochromocytomas, including hypertension, headaches, and palpitations.2,3
The superiority of laparoscopic surgery for PCC compared with open surgery has been demonstrated, such as less post-operative pain, rapid convalescence, a short hospital stay, and improved cosmetic results.4,5,6,7,8 Open surgery is the usual method for removing PGs, but performing laparoscopic surgery on these tumors is difficult due to their irregular location, the thick adhesions surrounding them, their rich blood supply, and their closeness to major blood vessels. Due to the rarity of the entity, only a few studies of laparoscopic surgery for PG have been reported, most of which were single-case reports or limited case series.3,9,10,11,12,13,14,15 To the best of our knowledge, most of these studies reported successful removal of PGs but simultaneously found longer operative time and a higher incidence of complications compared with PCC.13,14,15
In our retrospective study, we share our experiences with laparoscopic treatment of extra-adrenal pheochromocytomas. We compare the blood pressure and heart rate changes during these surgeries to those in laparoscopic removal of adrenal pheochromocytomas and assess the method’s practicality, safety, and surgical results.
PATIENTS AND METHODS
We retrospectively searched our database of medical records from June 2005 to June 2023 and retrieved the patients at Civil Hospital, Ahmedabad, Gujarat, India.
Patients satisfying the following criteria were included:
1. Primary single paraganglioma established by post-operative pathology, irrespective of size, and
2. Laparoscopic surgeries performed via transperitoneal approach by the same surgical team.
Patients with the following criteria were excluded:
1. Confirmed pre-operative metastasis, invasion of the surrounding structure.
2. Insufficient peri-operative data.
3. Recurrent PGs.
Pre-operatively, all the subjects to undergo laparoscopic surgery gave consent to open surgery as an alternative when necessary. Over an eighteen-year study period, 27 qualified patients with PG were enrolled in the study. All patients’ metanephrine and cortisol levels in serum samples were measured pre-operatively. All the retroperitoneal masses were pre-operatively assessed by computed tomography (CT) for surgical planning.
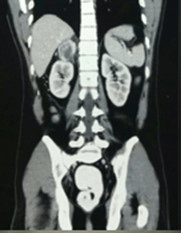
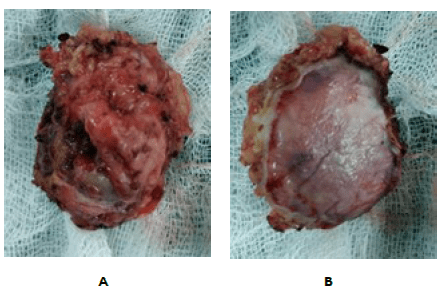
The pre-operative diagnosis of PGs was made by monitoring serum catecholamine levels and serum metanephrine levels. Of all the 27 cases, 17 had functional tumors. The other 10 cases have non-functional tumors diagnosed as suspected PGs pre-operatively according to clinical symptoms (hypertension, sweating, or palpitations) and tumor characteristics in the CT scan (location and obvious enhancement). The mean size of the pheochromocytoma is 3.7±1.2 cm (mean±SD). The diagnosis of PGs was confirmed for all 27 cases by post-operative pathology (pheochromocytoma) (Figures 1 and 2) (Tables 1 and 2).
Figure 1. CECT A+P S/O Right Adrenal Mass
Figure 2. Specimen (A and B)
| Table 1. Baseline Characteristics of Enrolled Subjects |
| A. According to Sex |
| Sex |
Number |
| Male |
19 |
| Female |
8 |
| Total |
27 |
| B. According to Location |
|
Left |
Right |
Total |
| Number |
11 |
16 |
27 |
| Table 2. Locations of the PGs |
| Location |
Number |
Percentage |
| Adrenal |
24 |
88.8 |
| Extra adrenal |
3 |
11.1 |
Pre-Operative Preparation of the Patients
All the enrolled subjects received α-adrenergic blockade (phenoxybenzamine) at least two weeks before surgery, starting with a dose of 10 mg per day and gradually increasing to 30-90 mg per day. The surgical prerequisites included stable blood pressure (below 140/90 mm Hg) and a heart rate (<90 beats per minute) for at least one week. β-adrenergic blockade was instituted if tachycardia occurred following α-adrenergic blockade. The last phenoxybenzamine was administered on the morning of the operation day.
Surgical Equipment
Commonly, we choose a 30° scope rather than a 0° scope because the former has a wider observation range. Ultrasound is the most commonly used energy platform during surgery. Hem-o-lock clips could be used to clamp large vessels, while hook electrics could help with fine dissection. Moreover, a titanium clip and laparoscopic needle holder should be prepared as a backup.
Peri-Operative and Follow-Up Data Collection
The hospital charts and operative notes of enrolled subjects were reviewed retrospectively, along with the baseline characteristics and the surgical outcomes. A “hypertensive episode” was defined as an increased systolic blood pressure (SBP) by 30% above the baseline level or an SBP of 200 mm Hg or higher. A ‘‘hypotensive episode” was defined as SBP that decreased below 80 mm Hg.14 Post-operative surgical complications within 1-month were recorded and evaluated according to Clavien-Dindo’s classification.16
After surgery, all patients underwent a one-month follow-up, followed by regular monitoring through computed tomography scans and blood tests for serum cortisol and metanephrine every 3 to 6 months. During this follow-up period, any instances of local recurrence or distant metastasis were documented.
RESULTS
Among the pre-operative symptoms of paragangliomas (PGs), hypertension was the most frequent, affecting 81.4% of patients, followed by sweating in 77% and palpitations in 44%, among other symptoms (Table 3).
| Table 3. The Symptoms of the PGs |
| Symptoms |
Number of Patient having Symptoms |
Percentage(%) |
| Hypertension |
22 |
81.4 |
| Persistent hypertension |
19 |
70.3 |
| Paroxysmal hypertension |
3 |
11.1 |
| Sweating |
21 |
77.7 |
| Palpitation |
12 |
44.4 |
| Headache |
14 |
51.8 |
| Anxiety |
5 |
18.5 |
The peri-operative data were summarized in the following Table (Table 4).
| Table 4. Perioperative Data |
| Open conversion (cases) |
1 |
| Mean size |
3.7±1.2 cm |
| Operative time (min) |
8 |
| (mean±SD) |
195.59±29.12 |
| Estimated blood loss (ml) |
2 |
| (mean±SD) |
360.78±184.70 |
| Blood transfusion (cases) |
5 |
| Intraoperative hemodynamic changes |
| 1. Incidence of hypertensive episode |
14/27 |
| 2. Incidence of hypotensive episode |
12/27 |
| Post-operative hospital stay (days) |
5.81±0.77 |
| Post-operative complications (cases) |
2 |
In this study, one open conversion occurred because of dense adhesion between the tumors and inferior vena cava (IVC), and it was subsequently performed successfully without intraoperative blood transfusions or other complications. All the PGs were resected with negative tumor margins, confirmed by post-operative histopathology (pheochromocytoma).
The operative time and estimated blood loss were analyzed in the 27 cases who underwent successful surgery, which were 195.59±29.12 minutes and 360.78±184.70 mL, respectively. Intraoperative blood transfusion occurred in 5 patients because of relatively large blood loss (600-1100 mL), and these 5 PGs were all resected successfully via transperitoneal approach without conversions to open operations. The maximum diameters of the 5 PGs were 4.7 cm, 4.8 cm, 5.0 cm, 5.8 cm and 6.5 cm, which all showed dense adhesion to surrounding tissues or great vessels. The post-operative hospital stay was 5.81±0.77 days.
Two post-operative complications were observed in this study, including Clavien Grade I (2 wound infections). All complications that occurred after surgery were managed conservatively without any further deterioration.
The follow-up interval ranged from 6 to 55 months (median 31 months), during which no local recurrence or distant metastasis occurred.
DISCUSSION
In this study, only one conversion to open surgery occurred due to the dense adhesions to the IVC other than surgical technical issues. The evaluation was done carefully with CT findings, meta-iodobenzylguanidine ( MIBG), clinical signs and symptoms, and a 24-hour urinary catecholamine, which suggests a unanimous conclusion about the nature of tumor characteristics.17
Functional paragangliomas, which make up 25% to 60% of all cases, produce too much catecholamine. This overproduction causes symptoms related to high catecholamine levels. Consequently, managing intraoperative hemodynamic changes becomes a crucial factor in ensuring the safety of paraganglioma resection.2,3
In this study, unmanageable hypertensive or hypotensive crises did not occur. In our experience, careful pre-operative pharmacological preparation was important for success, and a strategy similar to PCC was also appropriate for PG.
In our follow-up, there was no recurrence or metastasis after 6 months of operation, which shows that surgery was possible and possibly acceptable with a good prognosis.
In our opinion, the key to a successful laparoscopic surgery lies primarily with the surgical team. Due to variations in the lesion sites and the complicated relationship with great vessels.
Laparoscopic procedures were done via the transperitoneal approach because of the broad working space and maximal tumor exposure.
Two important indicators to assess the efficacy of a procedure are operational time and estimated blood loss. In several studies, that enrolled 5-9 PGs with smaller sizes (3.3-4.8 cm),3,13,14 the operative time of transperitoneal laparoscopic resection ranged from 189.8 to 290.4 min, and the estimated blood loss was 108-1036.3 mL. similar to our study demonstrated similar operative time (195.59±29.12 min) and estimated blood loss (360.78±184.70 mL).
Additionally, in our study, intraoperative blood transfusion was required in 5 cases due to a large amount of blood loss (600-1100 mL). These tumors were not only relatively large (4.7 cm, 4.8 cm, 5 cm, 5.8 cm and 6.5 cm), but also densely adhered to surrounding tissue and great vessels, which raised the complexity of tumor dissection.
LIMITATIONS
The limitations of this study were related to its retrospective nature, which will introduce uncontrolled recall bias and confounders, inevitably affecting the results. Second, there are only 3 cases of extra-adrenal, compared to 24 cases of adrenal. So, it will impact the accuracy of the study through sampling bias. Another limitation is that the follow-up interval was relatively short; thus, further investigation is warranted to track the surgical results in the long run.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.