INTRODUCTION
Since renal calculi was successfully removed by percutaneous nephrolithotomy (PCNL) reported in 1976, it became the standard treatment for large (>2 cm) renal stones.1 On the other hand, the complications and morbidity associated with the PCNL remains matter of concern.2,3 During puncture and dilatation of nephrostomy tract, the injury to renal parenchyma could be a major limiting factor of PCNL. It has been overcome by miniaturization of the renal access tract and nephroscope. The miniaturized (mini)-PCNL technique was initially developed for children, subsequently used in adults with a specially designed mini-nephroscope. Comparable success rate has been reported with mini-PCNL with standard prone lithotomy position in adults.4 However, increased morbidity has been reported, mainly due to cardiac and respiratory hindrance.5 Valdivia et al6 introduced the supine position and subsequently many variations in the patient positions with advantages and disadvantages. Supine PCNL was reported to be promising initially in terms of complication rate; however, recent meta-analysis does not support these finding.7,8,9,10 Intra-operative and post-operative outcomes, such as length of stay, duration of the operation and blood transfusion could be important to differentiate supine and prone positioning. A meta-analysis by Kumar et al11 reported lower blood transfusions and less operative time in supine position. However, recently reported meta-analyses did not report difference between the operation time between supine and prone positions.7,8,9 The advantages of supine are comfortable patient positioning, lesser radiation exposure of the surgeon, easy access to airways, possibility of simultaneous retrograde access, and low pressure in the renal pelvis.12 In prone position, the hindrance to access the respiratory system by anesthesiologist could be a limiting factor.
Many studies have been published in the literature comparing efficacy and safety of prone and supine positions in the patients undergoing PCNL. But the comparison of supine and prone positioning in patients undergoing mini-PCNL is scanty. A study by Tokatl et al13 compared the mini-PCNL performed in these two positions. No significant difference has been reported between these two approaches in terms of stone-free rates, complication rates and hospital stay. However, longer operative time has been reported in prone position.
The present study aimed to compare the success and complication rate of supine and prone mini-PCNL in patients with renal calculi 1-3 cm in size.
MATERIAL AND METHODS
This was a prospective observational study conducted at the Department of Urology, Apollo Main Hospitals, Chennai, India, from September 2017 to February 2019. The study protocol was approved by the Institutional Ethics Committee and study procedure was in accordance with the principles of the Declaration of Helsinki. All patients provided written informed consent.
Inclusion Criteria
All in-patients, more than 18-years of age with renal calculi of 1-3 cm in size, who underwent mini-PCNL during the study period were included in this study.
Exclusion Criteria
Patients with following conditions were excluded;
1. Complete staghorn calculus.
2. Altered anatomy limiting access to the kidney in the supine position (such as horseshoe kidney, pelvic kidney, retro renal colon, transplant kidney, etc.)
3. Medical comorbidities including coagulation abnormalities, cardiovascular and respiratory conditions which render patients unfit to withstand anesthesia.
4. Active urinary tract infection.
5. Pediatric patients.
After pre-operative assessment for surgical and anesthetic safety, patient underwent one of the two procedures, either supine or prone mini-PCNL as per the surgeon’s and patient’s preference. Bulls eye technique was used for all prone cases and free hand technique for supine cases. Sheath size used was between 14 Fr, 15.5 Fr, 16 Fr based on stone burden. The criteria for not putting double-J (DJ) stents/nephrostomy is mostly due to low intra-operative bleeding, no procedural complications which was purely surgeon’s choice based on the above factors. Operating time was considered from the time of induction of patient till removal of Amplatzs heath after confirmation of stone clearance. Supine mini-PCNL was done by one individual surgeon and prone mini-PCNL was done by another individual surgeon. No multiple surgeons for individual approach.
Demographic details such as age, sex, body mass index (BMI), co-morbidities, date of submission, surgery, and discharge, stone characteristics (size, location and number) were recorded. Pre-operative investigations included evaluation of complete blood count, serum levels of creatinine, blood urea, and coagulation profile. The stone size of the patients was determined by computed tomography (CT) scan and kidney, ureter, and bladder (KUB) X-ray of the intravenous urography series. Intra-operative assessments including stone clearance, operation time, puncture techniques under fluoroscopic guidance, lithotripter and puncture site, complications, usage of nephrostomy, placement of DJ stent and post-operative evaluations including hospitalization time, complications, drop in hemoglobin, secondary procedures for residual fragments were performed in all the patients. Post-operative complications were assessed during the period of 60 days. In post-operative follow-up, patients were assessed for stone clearance by KUB X-ray and stents were removed if deployed.
Statistical Analysis
The sample size was calculated using the software G*Power 3.1.9.2 based on the parameters of Giusti G et al14 The required sample size calculated was 35 patients in each group. All statistical analyses were performed using statistical package for the social sciences (SPSS) version 16.0. All the numerical variables were presented as mean (standard deviation (SD)) or median (interquartile range). All categorical variables were expressed as number (percentage). Categorical variables were compared with Chi-square (χ) test or Fischer’s exact test. Continuous variables were compared with independent sample t-test (for normally distributed data) or Mann–Whitney U test (for skewed data). Statistical significance was defined as p<0.05.
RESULTS
A total of 116 patients were enrolled in this study. Out of these, 52 patients underwent supine mini-PCNL and 64 patients underwent prone mini-PCNL. The mean age of the patients in supine and prone mini-PCNL groups was 47.40 and 47.95-years, respectively (p=0.79). The male to female ratio in supine and prone mini-PCNL groups was 3.9:1 and 2.7:1, respectively. No significant difference was observed in mean BMI between supine (26.71 kg/m2) and prone mini-PCNL groups (25.40 kg/m2) (p=0.16). In supine and prone min-PCNL groups, respective mean hemoglobin was 13 gm% and 13.42 gm%, respectively. The mean blood urea levels in prone mini-PCNL group was slightly higher (26.19 mg/dL) compared to the supine mini-PCNL group (23.21 mg/dL). The mean serum levels of creatinine in prone mini-PCNL group was marginally higher (1.33 mg/dL) compared to the supine mini-PCNL group (1.02 mg/dL). In both the groups, no significant difference was observed in the biochemical parameters (hemoglobin, blood urea and serum creatinine). The mean stone size was comparable between supine and prone mini-PCNL groups (15.53 mm and 16.33 mm, respectively) (p=0.43). The respective mean number of stones in supine and prone mini-PCNL group was 1.43 and 1.32. The respective number of patients with left sided procedure in supine and prone mini-PCNL groups were 56% and 44%, while number of patients with right-sided procedure were 44% and 56% (Table 1).
| Table 1. Demographic and Biochemical Parameters |
| Parameters |
Supine mini-PCNL (n=52) |
Prone mini-PCNL (n=64) |
p value |
| Age (years) |
47.40 (10.28) |
47.95 (12.03) |
0.79 |
| Sex, n (%) |
| Male |
38 (73) |
51 (81) |
0.16 |
| Female |
14 (27) |
13 (19) |
0.3 |
| BMI (kg/m2) |
26.71 (5.19) |
25.40 (4.57) |
0.16 |
| Hemoglobin (gm%) |
13.00 (2.01) |
13.42 (1.93) |
0.27 |
| Blood urea (mg/dL) |
23.21 (7.37) |
26.19 (9.88) |
0.08 |
| Serum creatinine (mg/dL) |
1.02 (0.57) |
1.33 (2.49) |
0.39 |
| Stone size (mm) |
15.53 (5.67) |
16.33 (6.00) |
0.43 |
| Number of stones |
1.43 (0.73) |
1.32 (0.62) |
0.39 |
| Laterality of Procedure, n (%) |
| Right |
23 (44) |
36 (56) |
0.2 |
| Left |
29 (56) |
28 (44) |
0.2 |
Data shown as mean (SD), unless otherwise specified.
BMI, body mass index; mini-PCNL, miniaturized percutaneous nephrolithotomy. |
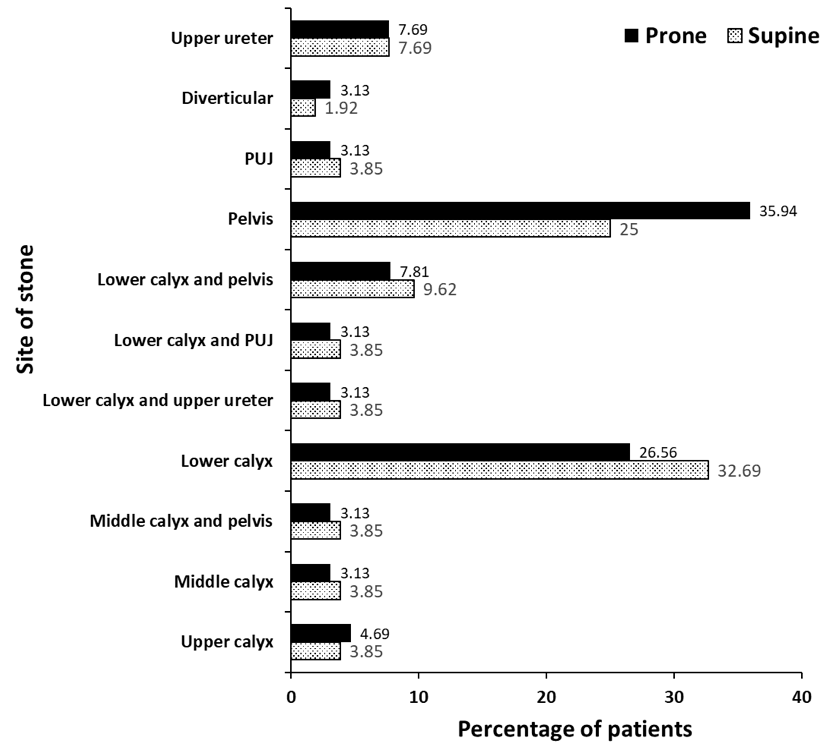
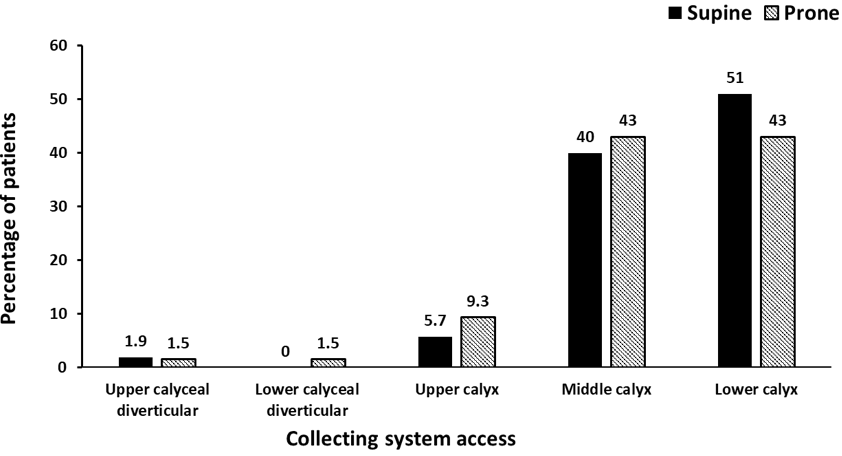
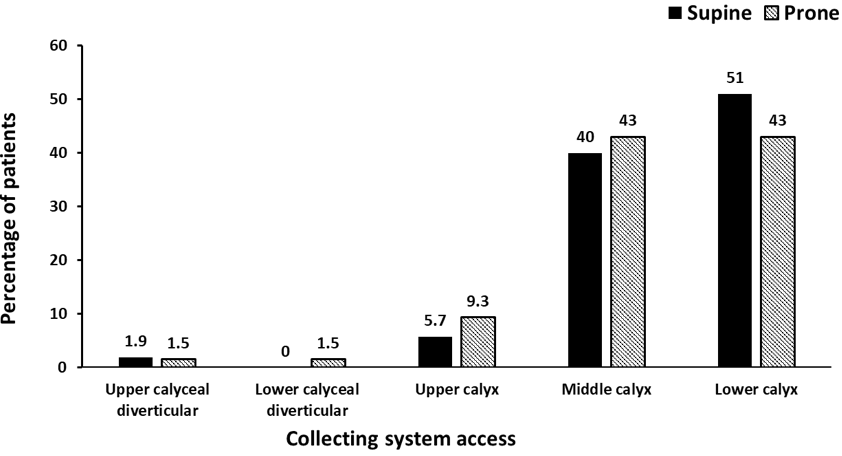
In supine mini-PCNL group the most common site of stone was at lower calyx (32%), followed by renal pelvis (25%), however, in prone mini-PCNL group the most common site of stone was renal pelvis (35%), followed by lower calyx (26%). Diverticular stones were presentin one patient (1.92%) of supine mini-PCNL group, and two patients (3.13%) of prone mini-PCNL group (Figure 1). The most commonly used site of access to reach the stone in supine and prone mini-PCNL groups was lower calyx (51% and 43%, respectively), and middle calyx (40% and 43%, respectively) (Figure 2).
Figure 1. Site of Stone
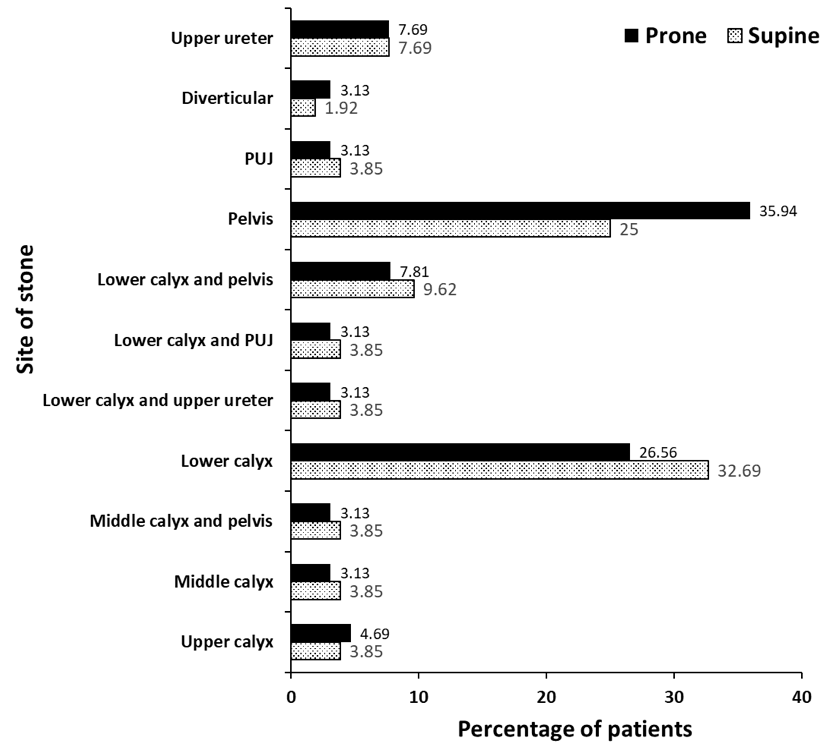
Figure 2. Collecting System Access
The mean operative time and mean hospital stay was significantly lower in supine mini-PCNL compared to the prone mini-PCNL group (44.89 vs. 53.94 min, p=0.007 and 2.06 vs. 2.51 days, p=0.01, respectively). All patients in supine mini PCNL group had 100% stone clearance, however, one patient in prone mini-PCNL group had residual fragments. The number of patients having nephrostomy was significantly lower in supine mini-PCNL group (9%) as compared to prone mini-PCNL group (74%) (p<0.0001). The number of patients with DJ stent placement was significantly lower in supine mini-PCNL group (29%) as compared to prone mini-PCNL group (85%) (p<0.0001). The number of tubeless (no nephrostomy) and totally tubeless (no nephrostomy plus no DJ stent) procedures were significantly higher in supine mini-PCNL group (90% and 61%, respectively) as compared to prone mini-PCNL group (23% and 4%, respectively) (p<0.0001). The mean drop in haemoglobin was significantly lower in supine mini-PCNL group (1.30 gm/dL) compared to prone mini-PCNL group (1.62 gm/dL) (p=0.009). In both the groups, none of the patients reported collecting system injuries or visceral injuries. One patient in supine mini-PCNL had right lower lobe basal atelectasis and underwent 3 units packed red cell blood transfusion for haemoglobin drop from 9.3 gm/dL to 7 gm/dL in post-operative period.
In prone mini-PCNL group, one patient required blood transfusion for significant drop in haemoglobin from 12.3 gm/dL to 7.8 gm/dL. This patient had right renal subcapsular hematoma with multiple pseudoaneurysms as diagnosed by CT Renal angiography in post-operative period. The right renal artery super selective angioembolization was performed to control the post mini-PCNL bleeding. Another patient from prone mini-PCNL group reported residual fragments for which extracorporeal shock wave lithotripsy (ESWL) was performed post-operatively for complete stone clearance (Table 2). Right lower lobe basal atelectasis reported in two patients, one patient each in both the prone and supine mini-PCNL groups.
| Table 2. Post-Operative Parameters |
| Parameters |
Supine mini-PCNL (n=52) |
Prone mini-PCNL (n=64) |
p value |
| Operative time (min), mean (SD) |
44.89 (10.48) |
53.94 (22.21) |
0.007 |
| Hospital stay in days, mean (SD) |
2.06 (0.42) |
2.51 (1.23) |
0.01 |
| Stone clearance |
52 (100) |
63 (98) |
0.3 |
| Nephrostomy |
5 (9) |
49 (74) |
<0.0001 |
| DJ stenting |
15 (29) |
55 (85) |
<0.0001 |
| Tubeless (no nephrostomy) |
47 (90) |
15 (23) |
<0.0001 |
Totally tubeless
(no nephrostomy+no stent) |
32 (61) |
3 (4) |
<0.0001 |
| Drop in hemoglobin (gm/dL), mean (SD) |
1.30 (0.7) |
1.62 (0.6) |
0.009 |
| Complication |
| Bleeding mandating transfusion |
1 (1.92) |
1 (1.56) |
– |
| Residual fragments |
0 |
1 (1.56) |
– |
Data shown as n (%), unless otherwise specified.
double J (DJ ); miniaturized percutaneous nephrolithotomy (mini-PCNL). |
DISCUSSION
Urolithiasis especially renal calculi are major risk factor associated with increased prevalence worldwide. Mainly, surgical procedure with high stone free rate, minimal risk of hemorrhage and decrease operative time should be considered as a standard treatment for renal calculi. PCNL has an excellent stone clearance rate which is an advantage over the previous minimal invasive procedure. Recently, to decrease renal parenchymal trauma conventional PCNL is shifted to a mini-PCNL with smaller tract size (11-20 Fr). An important topic to address is whether miniaturization affects the outcomes of the procedure comparing between prone and supine positions. The data in the literature concerning this subject are very limited. There are only two studies reporting the comparison between supine and prone mini-PCNL.13,15
The present prospective study comparatively assessed the outcome of supine and prone mini-PCNL. In this study the mini-PCNL was preferred over retrograde intrarenal stone surgery (RIRS) to achieve complete stone clearance, as at the present study site several RIRS are preformed, sometimes unavailability of flexible ureteroscopy for kidney stones (URS) due to repairs. Hence, in the present study only mini-PCNL in both positions were evaluated. Both the procedures were comparable in terms of complications. However, operation time and hospital stay in the supine mini-PCNL were significantly shorter compared to prone mini-PCNL. Though, the reason for shorter hospital stay is not very clear most of the supine cases have no nephrostomy, so that could be one of the possible reasons for being pain free early recovery. The mean age and gender wise distribution of patients in both the groups was comparable and majority of patients were men. This is in accordance with the previous studies which also showed men prevalence in these patients.13,16
In the present study, the mean operative time in the supine mini-PCNL group was significantly shorter compared to prone mini-PCNL group. The reduced operation time in the supine mini-PCNL was due to lack of repositioning of supine lithotomy position to prone one which saves the time with less complexity and minimal operation theatre personnel. Even though the mean operation time was significantly shorter in the supine PCNL group than prone PCNL group in the previous studies, the hospital stay did not differ between these two groups.7,8,9,13,15,16 In contrast, the present study reported significantly shorter hospital stay in the supine mini-PCNL group. However, a meta-analysis including 20 studies reported similar operation time and hospital stay between both the groups.10
In this study, prone and supine mini-PCNL have similar stone clearance rate which is consistent with previous studies.9,13,17 In contrast, a meta-analysis based on 9 studies involving 4956 patients with prone PCNL and 1457 patients with supine PCNL, showed significantly higher stone free rate in the prone position than supine position.8 Higher stone free rate in prone position maybe due to the effects of gravity on the irrigating fluid, and an unrestricted range of movement for the nephroscope, the prone position are easier access to the renal upper pole calices, a more distended collecting system for better vision, therefore, better clearance of stones.18,19
A retrospective study of 180 patients treated with mini-PCNL either in supine or prone position using nephrostomy tube reported similar success rate with shorter operative time and is only benefit of supine position over prone position. Similar results were obtained in a randomized study of patients with upper urinary tract calculi using prone and supine minimally invasive PCNL. A nephrostomy tube was placed in all the patients with post-operative internal stent.13 Nephrostomy tube placement and DJ stent placement after mini-PCNL depends upon many factors like intra-operative bleeding, size of the stones and more of surgeons’ preference. A study done by Gupta et al. reported ultra-mini PCNL in supine position with a complete tubeless approach for renal stone disease is a safe method for treating low-volume disease.20 The smaller access tract helps to make mini-PCNL tubeless or totally tubeless. In the present study, 47 and 15 procedures were tubeless and 32 and 3 procedures were totally tubeless in the supine mini-PCNL and prone mini-PCNL group, respectively. In both supine and prone mini-PCNL groups most of the patients who does not have nephrostomy or DJ stent, were retained with retrograde catheter (5 Fr open ended ureteric catheter) which was drained into Foleys catheter during their post-operative period.
Regarding the complications, only one patient from each group had required blood transfusion and one patient in the prone mini-PCNL group reported residual fragments. Meta-analysis of nine studies demonstrated lower blood transfusions in the supine position than in the prone position.7 Whereas, randomized study of 109 patients with upper urinary calculi reported no requirement of transfusion in either groups. A meta-analysis was done to assess the best position for the management of kidney stones; reported patients in the supine PCNL group received less transfusion and had less fever rates.10 Another recent meta-analysis of 15 randomized controlled trials involving 1474 patients revealed comparable results in overall complications rate and blood transfusion between supine PCNL group and prone PCNL group.9 A case series of 14 patients who underwent ultra-mini PCNL in the supine position demonstrated only one patient had residual fragments and needed subsequent extracorporeal shock wave lithotripsy.20
The present study has few limitations. It is a non-randomized observational study with relatively small sample size. The supine mini-PCNL has been performed by a single surgeon. However, prone mini-PCNL has been performed by different surgeons. This might have attributed to the variation observed in operation time for each patient. This study did not report the need of analgesic requirement and morbidity associated with DJ stent placement.
CONCLUSION
In the treatment of renal calculi of 1-3 cm in size, supine mini-PCNL can be an alternative option for prone mini-PCNL as stone clearance rate and complications were similar in both the groups. However, significantly shorter operative time and hospital stay were benefits of the supine mini-PCNL technique.
FUNDING
None.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.