BACKGROUND
As patient’s awareness and technical expertise increase, the rates of breast reconstruction after mastectomy continue to rise,1 but enormous differences can be observed: a median overall reconstruction rate of 24% has been reported, ranging from 5-81%.2 Implants seem to be the most frequent type of reconstruction, whereas the use of autologous techniques is decreasing.1,3
Several Breast Implant crises were generated in the 90’s4 and more recently the Poly Implant Prosthesis (PIP) Breast Implants in 2010.5,6 The U.S had not been involved in the PIP crisis,7 but the European countries and Australia have reacted in different ways to this issue7,8,9,10 which clinical implications have been reviewed recently.11 In March 2010, the French national regulation agency (AFFSAPS) requested that doctors’ call back all women who had undergone breast reconstruction/augmentation based on PIP implants. The PIP recall was because the implants were produced with a non-homologated silicone gel. Considerable media attention was attracted by the PIP scandal in France. The characteristics of this scandal have been described in depth by Greco.12 The publicity it generated seemed likely to have affected women with breast cancer psychologically in terms of their satisfaction and regret with breast reconstruction and their trust in health care professionals. These effects were expected to have occurred not only in women with breast cancer who had been given PIP breast implants, but also in those who had undergone other types of breast reconstruction.
The aims of this study were: first to describe the perceived impact of the PIP recall in a prospective cohort of breast cancer women, depending on the type of breast reconstruction undergone, and secondly, to analyze the individual determinants of patient’s satisfaction and regrets about breast reconstruction, taking the patients’ experience of the initial decision-making process into account.
METHODS
Participants
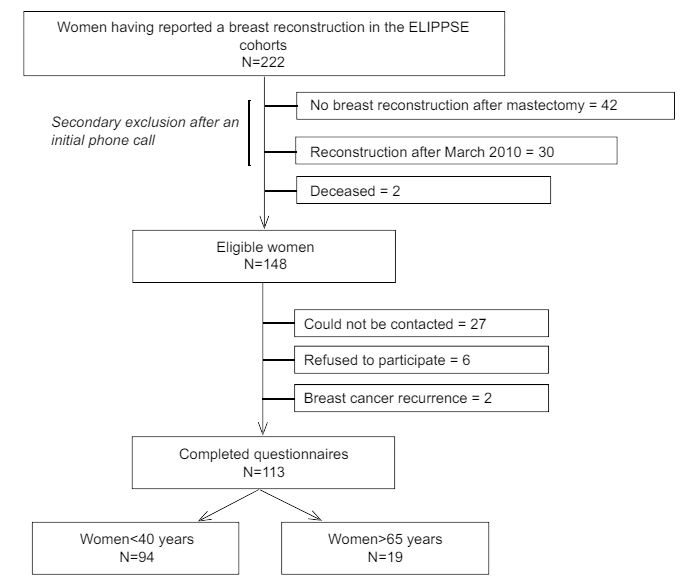
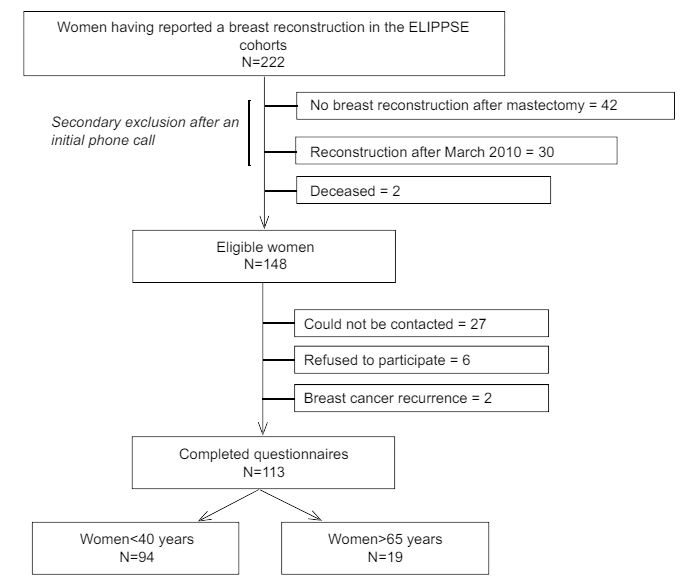
Participants were selected from two geographically designed cohorts of breast cancer women, the ELIPPSE (Etudes Longitudinales sur l’Impact Psycho-social des Pathologies du Sein ie. Longitudinal Studies on Psycho-social Impact of Breast Diseases) cohorts (N=1357). These cohorts which included women with/without mastectomy were set up to document the effects of breast cancer and its treatment on women’s everyday lives.13,14,15,16 Eligible patients for these cohorts were all women with incident primary breast cancer (time period of diagnosis: 2004-2008) aged 18-40 (ELIPPSE 40) or >65 (ELIPPSE 65) living in South-eastern France at the time of their cancer diagnosis. These women have been followed during 5 years after the initial diagnosis with closed questionnaires administered by telephone. Women with distal metastases at diagnosis, serious cognitive deficits, and those unable to answer questionnaires were excluded. Only the women who had a previous mastectomy and who declared a breast reconstruction before March 2010, the time of the PIP recall by the national regulatory agency in France were eligible to participate in this study.12 This represents a small subset of the overall ELIPPSE cohorts since a minority of the women had a mastectomy and in this group not so many women had a breast reconstruction completed before March 2010. A specific cross-sectional telephone survey was performed on these women after an initial phone call to check the validity of women’s declarations (Figure 1).
Figure 1: Sample selection pathway
Data Collection
Enrolment in the ELIPPSE cohorts resulted in regular scheduled telephone interviews with the women and medical questionnaires sent to the physicians in charge of breast cancer. Details about these cohorts have been published elsewhere.13,14,15,17 For this study, it was designed specifically for the women who had a breast reconstruction before the PIP recall a cross-sectional telephone survey based on a closed questionnaire which content is presented below was conducted between June and September 2013 in order to collect details about the type of breast reconstruction, the number of surgeries and the procedure involved.
Sociodemographic (age, educational level, and marital life) and medical data (clinical stage, treatment) were obtained from the ELIPPSE cohorts questionnaires, whereas the variables relating to breast reconstruction and psychosocial characteristics detailed below were collected in the cross-sectional questionnaire. When a French version of a scale had not been validated previously, it was translated following the procedures recommended.18
Impact of the PIP Recall
Impact of event scale: The distress generated by the PIP problems was measured using the 15-item Impact of Event Scale (IES).19 A French translation of this scale had been carried out and validated in previous studies.17 The women were asked to answer to the questions of their feelings corresponding to the months after they were informed about the PIP problems, i.e. the event was ‘the information time about the PIP problems’.
The IES includes two subscales measuring intrusive and avoidance ideation. In this study, both the Global IES score (Cronbach’s α=0.91) and the two subscales (intrusive ideation: Cronbach’s α=0.88 and avoidance ideation: Cronbach’s α=0.82) were measured.
Attendance at a medical centre: Women were asked what they knew about the PIP recall and whether they had been in contact with a medical Centre after hearing about this issue.
Trust in the medical team: Participants were asked whether the PIP recall had affected their trust in the medical team: increased trust/no change/decreased trust.
Women’s Decision-Making Characteristics
Type of decision-making: A French version of the Control Preference Scale was used to elicit Breast Cancer patient’s preferences about treatment decisions and to determine their perceived involvement in the decision-making about breast reconstruction.20 This 5-item scale, which has been widely used in studies on cancer patients,21 includes statements ranging from fully active/passive involvement to fairly active/passive involvement and shared decision-making. Preferred levels of involvement in decision-making were collected on the cohorts, while perceived involvement in breast reconstruction was collected in the cross-sectional survey.
Decisional conflict scale (short form): Patients’ decisional conflicts were tested using a 4-item scale, the SURE test.22 Decisional conflicts were taken to occur in women with a score below 4. Information seeking tendencies were measured using the Extent of Information Desire (EID) scale.23
Patient-Reported Outcomes about Breast Reconstruction
Satisfaction was assessed using a 10-point scale (“give a number between 0 and 10 to rate your satisfaction with Breast Reconstruction”).
Decisional Regret Scores about Breast Reconstruction were assessed using the Decision Regret Scale.24
Data Analysis
Chi2, Fisher’s exact tests and Student’s t-tests were used to make univariate comparisons. The links between Decisional regret about Breast Reconstruction and other variables were assessed by performing logistic regression. In our analysis Satisfaction with Breast Reconstruction was strongly associated with Breast Reconstruction Decisional regret. This variable was checked to be endogenous (because it may have depended on other predictive variables) by performing the augmented regression test presented by Davidson and McKinnon.25 As the results confirmed the presence of endogeneity, a simultaneous equations approach based on a two-stage regression procedure was used. In the first stage, instrumental variables were introduced into a linear model to predict Satisfaction about Breast Reconstruction. In the second stage, predicted Satisfaction scores about Breast Reconstruction were introduced into the model for Decisional regret about Breast Reconstruction rather than the actual Breast Reconstruction Satisfaction scores obtained.26 Adjustments were systematically made for age, level of education and type of Breast Reconstruction. Wald statistics and log-likelihood ratios were used to determine the significance of variables and model fit. Statistical analyses were performed using the STATA/SE 12.1 for Windows program.
Ethics Statement
The study was approved for ethics, consent and confidentiality of the data by the French National Committee on Informatics and Freedom (CNIL N°905296v1, 906277v2).
Results
Sample Characteristics
A total number of 222 women were initially identified for inclusion since they had declared a Breast Reconstruction at the time of their initial treatment. However, after the first telephone call, only 148 women were still eligible for our study (Figure 1). Among those not included, two had a recurrence of Breast Cancer, 6 refused to participate and 27 could not be contacted. A total number of 113 questionnaires were therefore available for analysis. No differences were observed between the socio-demographic or medical characteristics of respondents and non-respondents except for their educational level: the respondents included a higher proportion of women who had been educated beyond secondary school certificate level (66% versus 42%, p=0.01).
At the initial reconstruction, 90.3% (n=102) had a Breast Implant: 10.6% of them had a PIP Breast Implant (n=12), 79.6% had a Breast Implant other than PIP (n=90) and 9.7% (n=11) had undergone autologous reconstruction (Table 1). These three groups did not differ in terms of their socio-demographic or initial medical characteristics. The mean age was 49 at the time of the interview, and reconstruction had occurred 5.3 years on average before the survey. However, all the PIP implants had been removed by 2013. At least one implant had been removed since the initial treatment for Breast Cancer in 31.1% of the ‘other Breast Implants’ group.
| Table 1: Socio-demographic and medical characteristics, depending on the type of breast reconstruction – n=113. |
|
|
Type of reconstruction
|
|
|
Total
n=113
|
With PIP implant(s)
n=12 |
With implant(s) other than PIP
n=90 |
Autologous
reconstruction
n=11 |
p
|
|
N(%)
|
N(%) |
N(%) |
N(%)
|
|
| Socio-demographics at cancer diagnosis |
| Age, in years (mean(SD)) |
49(12)
|
46(10) |
49(12) |
48(14) |
0.687
|
Level of education >secondary school certificate
No
Yes
not specified |
62(55.9)
49(44.1)
2 |
4(33.3)
8(66.7)
– |
53(58.9)
37(41.1)
– |
5(55.6)
4(44.4)
2 |
0.246 |
Living with a partner
No
Yes |
95(84.1) 18(15.9)
|
11(91.7)
1(8.3) |
73(81.1)
17(18.9) |
11(100.0)
0(0.0) |
0.203
|
| Medical characteristics |
|
|
|
|
|
Year of diagnosis
2005
2006
2007
2008
2009 |
22(19.5)
25(22.1)
29(25.7)
22(19.5)
15(13.3)
|
2(16.7)
0(0.0)
4(33.3)
2(16.7)
4(33.3) |
19(21.1)
22(24.5)
20(22.2)
18(20.0)
11(12.2) |
1(9.1)
3(27.3)
5(45.4)
2(18.2)
0(0.0) |
0.180
|
Clinical stage at diagnosis
0/I
II/III
Not specified |
56(50.0)
56(50.0)
1
|
8(66.7)
4(33.3)
– |
43(48.3)
46(51.7)
1 |
5(45.4)
6(54.6)
– |
0.466
|
| Received chemotherapy
Yes
No
Missing |
67(61.5) 42(38.5)
4
|
6(50.0)6(50.0)
– |
53(61.6)33(38.4)
4 |
8(72.7)3(27.3)
– |
0.534
|
| Underwent radiotherapy
Yes
No
Not specified |
71(66.4) 36(33.6)
6
|
5(41.7)7(58.3)
– |
58(64.4)32(35.6)
6 |
8(72.7)3(27.3)
– |
0.239
|
| Immediate reconstruction
Yes
No |
43(38.1)
70(61.9)
|
6(50.0)6(50.0) |
35(38.9)
55(61.1) |
2(18.2)
9(81.8) |
0.273
|
| Implant removed after being placed
No
Yes
Not concerned |
62(60.8)
40(39.2)
11
|
–
12(100.0)
|
62(68.9)
28(31.1)
– |
–
–
11 |
<.001 |
|
Mean(SD)
|
Mean(SD) |
Mean(SD) |
Mean(SD)
|
|
| Time since breast reconstruction, in years |
5.3(1.4)
|
5.9(1.5) |
5.3(1.4) |
5.0(1.1) |
0.332
|
| Number of surgical interventions |
4(2)
|
5(3) |
4(2) |
4(2) |
0.072
|
Women’s Decision-Making Characteristics
The three groups differed in their preferred involvement in decision-making: the proportion of passive women were higher in the autologous implant group (81.8%), while the proportion of active women were higher in the PIP group. Actual involvement in reconstruction did not differ between the three groups, nor did the congruence between preferred and actual involvement in Breast Reconstruction. Decisional conflict was detected in 62.8% of women, but no significant differences were detected between groups.
The three groups’ information-seeking profiles differed slightly: women in the autologous group reported more frequently that they read all they could about their health (72.7%, versus 63.6% of the women in the PIP group and 41.4% of those in the other-BI group, p=0.07).
Declared Impact of the PIP Problem
The impact of the PIP problem, based on the overall IES score, and on the intrusion subscale was found to be significantly heavier in the PIP group than in the other groups (p<0.05). In the great majority (74.8%), the PIP problem had no consequences in terms of trust in the medical staff. However, 27% of the PIP group reported that their trust had decreased, when compared with 7.9% in the ‘other Breast Implant’ group (p=0.08). Details are given in Table 2.
| Table 2: Decision-making process about reconstruction and respondents’ psycho-social characteristics, depending on the type of breast reconstruction – n=113. |
|
|
Type of reconstruction
|
|
|
Total
n=113
|
With PIP implant(s)
n=12 |
With implant(s) other than PIP
n=90 |
Autologous reconstruction
n=11 |
p
|
|
N(%)
|
N(%) |
N(%) |
N(%)
|
|
Preferred involvement in decision-making
Fully/fairly passive
Shared decision-making
Fully/fairly active
Not specified |
55(50.0)
38(34.6)
17(15.4)
3
|
5(41.7)
3(25.0)
4(33.3)
– |
41(47.1)
35(40.2)
11(12.7)
3 |
9(81.8)
0(0.0)
2(18.2)
– |
0.034
|
Actual involvement in decision-making about breast reconstruction
Fully/fairly passive
Shared decision-making
Fully/fairly active
Not specified |
20(17..9)
60(53.6)
32(28.6)
1
|
3(27.3)
7(63.6)
1(9.1)
1 |
15(16.7)
46(51.1)
29(32.2)
– |
2(18.2)
7(63.6)
2(18.2)
– |
0.488
|
| Congruence between preferred and actual involvement
Less control than they wanted
As much control as they wanted
More control than they wanted
Not specified |
18(16.5)
40(36.7)
51(46.8)
4
|
3(27.3)
5(45.4)
3(27.3)
1 |
14(16.1)
32(36.8)
41(47.1)
3 |
1(9.1)
3(27.3)
7(63.6)
– |
0.524
|
| Decisional conflict scale
Decisional conflict
No decisional conflict |
71(62.8)
42(37.2)
|
9(75.0)
3(25.0) |
57(63.3)
33(36.7) |
5(45.5)
6(54.5) |
0.334
|
Breast Reconstruction Decisional Regret
No
Yes
Not specified |
48(42.9)
64(57.1)
1
|
2(18.2)
9(81.8)
1 |
41(45.6)
49(54.4)
– |
5(45.4)
6(54.6)
– |
0.220
|
Low health-related literacy. Needed help with reading instructions
No
Yes
Not specified |
95(85.6)
16(14.4)
2
|
11(100.0)
–
1 |
75(84.3)
14(15.7)
1 |
9(81.8)
2(18.2)
– |
0.349
|
| Effects of PIP scandal in terms of trust
Greater trust
No change in trust
Less trust
Not specified |
16(14.4)
83(74.8)
12(10.8)
2
|
1(9.1)
7(63.6)
3(27.3)
1 |
12(13.5)
70(78.6)
7(7.9)
1 |
3(27.3)
6(54.5)
2(18.2)
– |
0.164
|
I read all I can about my health problems
No
Yes
Not specified |
58(53.2)
51(46.8)
4
|
4(36.4)
7(63.6)
1 |
51(58.6)
36(41.4)
3 |
3(27.3)
8(72.7)
– |
0.072
|
|
Mean(SD)
|
Mean(SD) |
Mean(SD) |
Mean(SD) |
|
| Satisfaction with breast reconstruction score
Not specified |
7(2)
1
|
6(2)
– |
7(2)
1 |
8(1)
– |
0.006
|
| Impact of Event Scale (IES) about the PIP scandal
Not specified |
7(10)
7
|
15(13)
1 |
6(9)
5 |
7(13)
1 |
0.025
|
| Intrusion Subscale of IES about the PIP recall
Not specified |
4(5)
7
|
9(9)
1 |
3(4)
5 |
4(7)
1 |
0.001
|
| Denial Subscale of IES about the PIP recall
Not specified |
4(6)
7
|
6(7)
1 |
4(6)
5 |
4(6)
1 |
0.390
|
| Extent of information desired (EID) score
Not specified |
15(4)
5
|
15(5)1 |
15(3)4 |
13(3)- |
0.538
|
At the time of the survey, all the respondents knew about the PIP problems, 100 via the media, and 13 via a Surgeon/General Practitioner. After this disclosure, 50 declared that they had contacted their Surgeon/GP, 13 that the latter had contacted them, and 32 that they had checked the brand of their implant(s); 11 were not concerned as they had no implants, 7 did not contact their physicians as they were sure of being contacted if there was a problem, and the last woman did not contact her surgeon because she no longer trusted him.
Factors Associated with Satisfaction with Breast Reconstruction
The mean Breast Reconstruction satisfaction score differed significantly between the three groups (Table 2). It was lowest in the PIP group (6 versus 7 and 8 in the ‘other Breast Implant’ group and the autologous reconstruction group, respectively, p=0.006).
In the first stage, multivariate linear regression showed that neither educational level, age nor the number of surgical interventions was significantly associated with the respondents’ satisfaction (Table 3). Women who had undergone autologous reconstruction had significantly higher Breast Reconstruction satisfaction scores than those who were given implants. Satisfaction was found to be lower among the less health-literate women and among those with a high information-seeking profile; satisfaction was also lower among those whose trust in the medical profession decreased because of the PIP scandal.
| Table 3: Multivariate linear model for satisfaction about breast reconstruction (n=107). |
|
Multivariateanalysis
|
|
ẞ(sd)
|
p
|
| Effects of the PIP scandal in terms of trust |
|
|
| Greater trust / no change in trust |
Ref
|
|
| Less trust |
-2.02(0.67)
|
0.003
|
| Extentof information desired(EID) score |
-0.14(0.05)
|
0.014
|
| Type of breast reconstruction |
|
|
| With implant(s) other than PIP |
Ref
|
|
| With PIP implant(s) |
0.20(0.65)
|
0.755
|
| Autologous reconstruction |
1.57(0.66)
|
0.019
|
| Low health-related literacy. Needed help with reading instructions |
|
|
| No |
Ref
|
|
| Yes |
-1.23(0.60)
|
0.043
|
| Number of surgical interventions |
-0.17(0.09)
|
0.073
|
| Level of education |
|
|
| Secondary school certificate level or lower |
Ref.
|
|
| Above secondary school certificate level |
0.55(0.39)
|
0.161
|
| Age at diagnosis |
|
|
| <40 |
Ref.
|
|
| >65 |
0.46(0.53)
|
0.391
|
Factors associated with Breast Reconstruction Decisional Regrets
Regrets about their Breast Reconstruction decision were expressed by 57.1% of the respondents, and no significant differences were detected between the three groups. However, 81.8% of the PIP group expressed regrets about Breast Reconstruction, versus only 54.4% of the other women (p=0.07).
The results of the second stage in the analysis, which focused on the factors associated with Breast Reconstruction decisional regrets, are given in Table 4, taking the endogeneity induced by the ‘satisfaction with Breast Reconstruction’ variable into account. After adjusting for age and level of education, regrets about Breast Reconstruction were more frequently observed when the decision-making had not been sufficiently proactive. They also tended to be greater in the PIP group. In addition to these factors, regrets were associated with lower Breast Reconstruction satisfaction scores.
| Table 4: Factors associated with respondents’ decisional regret about breast reconstruction (n=107). |
|
Multivariate analysis
|
IV-logistic1 model
AOR CI(95%)
Ref=no regret |
p
|
| Satisfaction with breast reconstruction2 |
0.4(0.2-0.8)
|
0.005
|
| Congruence between preferred and actual involvement |
|
|
| More control than they wanted or as much control as they wanted |
1
|
|
| Less control than they wanted |
5.3(1.3-22.4)
|
0.023
|
| Type of breast reconstruction |
|
|
| With implant(s) other than PIP |
1
|
|
| With PIP implant(s) |
4.5(0.8-25.9)
|
0.091
|
| Autologous reconstruction |
3.6(0.6-20.2)
|
0.147
|
| Age at diagnosis |
|
|
| <40 |
1
|
|
| >65 |
1.8(0.5-7.0)
|
0.380
|
| Level of education |
|
|
| Secondary school certificate level or lower |
1
|
|
| Above secondary school certificate level |
0.7(0.4-2.1)
|
0.761
|
| 1Instrumental Variable logistic model, taking into account the endogeneity of the respondents’ satisfaction about breast reconstruction.
2as estimated by performing linear regression at the first stage in the analysis. |
DISCUSSION
This is a first study on the impact of the PIP recall on women who had undergone Breast Reconstruction in south-eastern France, where the PIP scandal was widely publicized. First, the psychological intrusive effects observed in the PIP group were not found to occur in the other groups of women. Secondly, the satisfaction with Breast Reconstruction declared by the participants five years after the initial cancer diagnosis was lower in those whose trust in their health professionals decreased, those who had a Breast Implant, those with the highest information-seeking profiles and those with lower levels of health-related literacy. Thirdly, some regrets about the Breast Reconstruction decision were expressed by a majority of the sample, especially when the decision-making had been less proactive than they would have liked and when they were less satisfied with Breast Reconstruction.
Few studies have been carried out on the psychological impact of the various Breast Implants crises which have occurred during the last thirty years on women undertaking reconstructive surgery. A specific study has been carried out on the PIP scandal in France, not specifically for reconstructive surgery, showing the interconnection of embodied experience and professional and public policy definitions of medical risk through the concepts of moral economy and biological citizenship.12 Anderson and Larson,27 who described patients’ reactions to the media coverage of the risks associated with silicone Breast Implants in the mid-90’s, observed that all the respondents coped with anxiety mainly by consulting their physicians. Among the 102 participants with Breast Implants in this study, 13 were contacted first by their healthcare providers (including all the women with a PIP Breast Implant), whereas 50 had contacted their healthcare providers themselves. It is worth noting that 32 of the women did not contact their physicians because they checked the brands of their implants, while 7 did not contact their physicians as they felt sure they would be contacted if there was a problem. The fact that the psychological effects of the PIP recall observed in the PIP group did not occur in the other groups reflects the existence of trust between these patients and their doctors.
Patients’ trust in their healthcare providers is a key to the women’s satisfaction with the Breast Reconstruction process. Satisfaction with the plastic surgeon has been previously reported to predict greater satisfaction with Breast Reconstruction.28 In previous studies on satisfaction with Breast Reconstruction, the role of various clinical variables was investigated, and women with autologous reconstruction were found to be more satisfied than those with implants,29 which was confirmed by the present results. Two other variables analyzed in our study were found to be independently related to satisfaction: higher information-seeking profiles and lower health-related literacy. Higher information-seeking profiles are often detected in people who have been described as “monitors”: those who need more information than other people.30 The association between satisfaction with the information provided and satisfaction with Breast Cancer treatment in general and preoperative information in particular has been documented.28,31,32 The results obtained here confirm that satisfaction with Breast Reconstruction does not depend directly on women’s age or educational level.29
Nearly half of young Breast Cancer survivors expressed some regret five years after their treatment;33 regret about Breast Reconstruction was also observed here in about half of the sample, in line with other studies.31,32 Post-decisional regrets were observed more frequently in our study when the decision-making was not felt to be sufficiently proactive and in those who were less satisfied with their Breast Reconstruction. The impact of shared decision-making is certainly worth investigating in this context34,35 with facilitating interventions.36,37
The main limitation of our study was that some of the sub-groups, such as the PIP Breast Implant and the autologous Breast reconstruction sub-groups, were very small, which reduced the statistical power of some of the analyses. With higher numbers a statistical significance of the PIP Breast Implant on the decisional regret may be found (Table 4). One of the strength of the study was its geographically based sampling with prospective follow-up of the women at the time of the PIP recall. However if one considers that one third of breast cancer women have a mastectomy and one fourth to half of them have breast reconstruction which is not immediate in most of the times,1 it was difficult to have a larger number of cases in a regional cohort.
The long-term effects of medical devices are often difficult to predict; however, the recent PIP saga was unique in that it was the only recall resulting from fraudulent procedures. This scandal, which confirmed the need for the regulation of medical devices Europe-wide, therefore had some needed reforms.9 Satisfaction and regrets are two a posteriori decisional indexes, which differ as was seen above. Regrets, which involve looking back at a decision when the outcome is not satisfactory, and participating actively in the initial decision-making are key issues which need to be attended to more closely. In the context of Breast Reconstruction, it is therefore essential to promote the involvement of women with Breast Cancer in the decision-making about mastectomy and to provide them with tailored information and specific interventions when feasible.36,37,38
CONCLUSION
The PIP recall did not appear to disturb women with non-PIP types of Breast Reconstruction in the context of this French regional cohort study. Involving women routinely in the initial decision-making process about Breast Reconstruction as much as they would like is likely to prevent the occurrence of subsequent regrets if it turns out that the final reconstruction does not meet their initial expectations. Promoting systematic large geographically-based data collections to obtain specific medical and psycho-social information may be an option to have up-to-date and representative data to measure the eventual psychological, social, and medical side-effects of new medical devices at a population level.
ACKNOWLEDGEMENTS
This study has been supported by a Canceropole PACA grant (emerging project 2013-2014).
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.