INTRODUCTION
According to the World Health Organization (WHO) and United Nations International Children’s Emergency Fund’s (UNICEF’s) World Report on Child Injury Prevention,1 while communicable diseases are still the primary killer of infants, injuries contribute significant proportions of deaths for children aged between 5 and 14 years (27%) and adolescents/young adults aged 15-29 years (40%). More specifically, drowning and road traffic injuries were reported to be the top ten causes of death amongst children between the ages of 1 to 14-years-old, and for those aged between 15 and 19 years old, road traffic injuries was the number one cause of death in the year 2004. Each year, injury and violence kills up to 950,000 children under 16 years of age and millions more suffer long-term consequences of non-fatal injuries.2 And about 60% of road traffic injury deaths occur in the South East Asian and Western Pacific Regions.3 Again, to further demonstrate the importance and significance of the burden of injuries to children, everyday over 2,000 children die as a result of an injury worldwide, and many more sustain severe injury outcomes.1
Based on the Child Maltreatment fact sheet by WHO, every year, there are an estimated 41,000 homicide deaths in children under 15 years of age.4 Reported levels of non-fatal abuse are much higher. It is important to take note that estimates are based on limited country-level data and reported cases only and may under-estimate the magnitude of the problem. It is suggested that many fatal cases due to maltreatment may go unreported especially in low and middle-income countries (LMIC) where injury reporting, databases, registries and surveillance systems are either non-existent or are limited in their ability to track those deaths.
Regardless of who the perpetrators are, child maltreatment is recognised globally as a serious public health, human rights, legal and social issue. In the majority of cases involving abuse/maltreatment, it is suggested that the physical injury itself may have less impact in terms of the damage to the child’s well-being compared with often devastating acute psychological and psychiatric consequences and long-term effects on the child’s cognitive, neurological and emotional development. Several studies indicated that exposure to abuse/maltreatment and other forms of violence during childhood is associated with a host of risk factors for other injurious events and risk-taking behaviours in life.5,6 Similarly, children who experience parental abuse or neglect are more likely to show negative outcomes that carry forward into adult life, such as ongoing problems with emotional regulation, self-concept, social skills, and academic motivation, as well as serious learning and adjustment problems, including academic failure, severe depression, aggressive behaviour, peer difficulties, substance abuse, and delinquency.7,8
In summary, the effect of child abuse/maltreatment on individuals can be devastating and life-long, with significant impact on many aspects of life, even during later stages of life. It also has an enormous impact on the economy, largely contributing towards the increasing burden on the healthcare system.
METHODS
The participants were recruited from three major public hospitals in the Klang Valley (Selayang Hospital, Serdang Hospital and Sg Buloh Hospital) and included emergency department (ED) specialists, paediatricians, medical officers, nurses and medical assistants using purposive sampling. The participants were invited to participate and recruited specifically if they worked directly with children presenting at the hospital (mainly at the Emergency Department and Paediatric Department).
A total of 30 participants were recruited and interviewed from all the three hospitals. Housemen were excluded from the study as they are considered to be trainees and would not have enough experience, knowledge and skills within the area of paediatric injuries (identification of accidental and non-accidental injuries); medical officers, nurses and medical assistants who have less than 2 years of experience working at the ED were also excluded.
Following interview protocols, each interview sessions lasted between 45 minutes to 1 hour and 30 minutes each depending on the knowledge and experience of each participant.
The number of healthcare professionals interviewed and years of service are shown in Table 1:
| Table 1. Frequencies and Percentages of Demographic Characteristics of Participants |
|
Variable
|
N=30 |
%
|
| Gender |
| Male |
12
|
40.00
|
| Female |
18
|
60.00
|
| Ethnicity |
| Malay |
25
|
83.30
|
| Chinese |
2
|
6.70
|
| Indian |
3
|
10.00
|
| Position |
| Specialist |
5
|
16.67
|
| Medical Officer |
11
|
36.67
|
| Nurse |
10
|
33.34
|
| Medical Assistant |
4
|
13.34
|
| Years in service |
| 0-5 years |
12
|
40.00
|
| 6-10 years |
12
|
40.00
|
| 11-15 years |
5
|
16.67
|
| 16-20 years |
1
|
3.34
|
A higher proportion of females (60%) compared with males (40%) were interviewed, and a range of experience levels were shown amongst the samples. In general, there was a high-level of experience with participants working around 8 years on average. Only two participants had worked for a minimum of two years and one for twenty years.
A questionnaire was developed to gather important information from the health professionals and was based on the Integrated Change (I-change) model used previously by Dutch researchers in 2009 amongst public and healthcare professionals.9 This model describes factors such as knowledge, attitude and skills that are involved in any behavioural (change) process.10
The model stems from the health promotion field and comprises concepts from the Theory of Planned Behaviour,11 Social Cognitive Theory,12 the Transtheoretical Model,13 the Health Belief Model,14 and Implementation and Goal Setting Theories.15 Although, several revisions have been made to the model, according to De Vries, it is still based on the fact that “covert and overt behaviors are determined by a person’s motivation or intention to carry out a particular type of behavior”.16
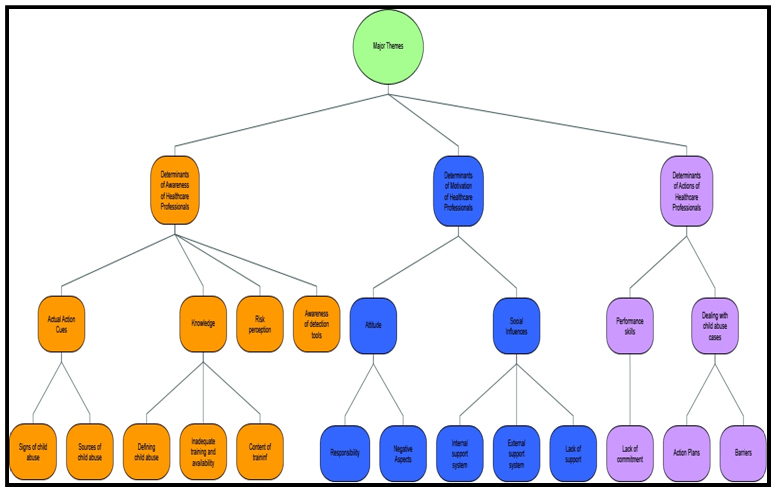
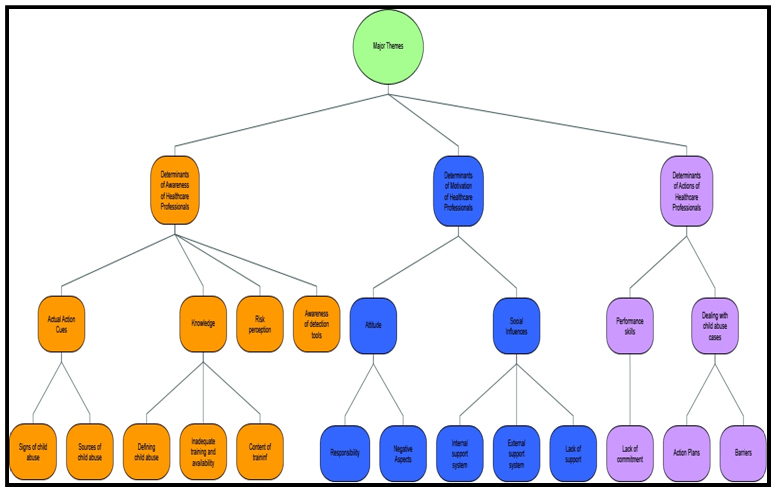
Upon completion of the interviews, audio recordings were transcribed initially into an electronic format (Microsoft Office word document). Once all interviews were transcribed and translated (if needed), they were transferred to NVivo qualitative analysis software. Keywords and phrases appeared as word clouds and text frequency which were analyzed and encoded with suitable category labels. Once these codes were categorized, they were compared to one another. Further refinement of these coding was done by identifying similar themes. Based on the I-change model of behaviour and suggested coding for NVivo analysis, several themes emerged. Under the first major theme on Determinants of Awareness of Healthcare Professionals, four key themes were identified.
RESULTS
First main key theme of “Actual action triggers”, several subthemes such as “Signs of child abuse” and “Sources of signs for abuse” emerged. The second key theme of “Knowledge”, several subthemes such as “Defining child abuse”, “Inadequate training and availability” and Content of training” emerged. Third key theme is “Risk Perception” and the last key theme is “Awareness of detection tools”.
The second major theme is on Determinants of Motivation of Healthcare Professionals, two key themes were identified. The first main key theme of “Attitude”, several subthemes such as “Responsibility” and “Negative aspects” emerged. The second key theme of “Social influences”, several subthemes such as “Internal support system”, “External support system” and “Lack of support” emerged.
The third and final major theme is on Determinants of Action of Healthcare Professionals, three key themes were identified. First main key theme of “Performance Skills” the subtheme of “Lack of commitment” emerged. The second main key theme of “Dealing with child abuse cases”, two subthemes emerged such as “Action plans” and “Barriers” emerged. Visual representation of the themes is shown in Figure 1.
Figure 1. Development of Coding Based on Major Themes, Key Themes and Subthemes Adapted from the I-change Model.
1. Major Theme 1: Determinants of Awareness of Healthcare Professional
Keytheme 1: Trigger for Actions
The participants were asked how they go about determining whether a child is suspected of being abused or not when the child presented himself/herself at the ED. Subthemes emerged from these questions are discussed in detail below.
Subtheme 1: Signs of abuse
The participants reported that they depend on the physical signs to detect abuse. There are neither detection nor screening tools that is currently being used in any of the hospitals to detect child abuse in the emergency settings. Most medical officers claimed that the most reliable signs of abuse that they looked for in a child who came with injuries are the inconsistency in the history and physical signs. One medical officer noted that changes in the history telling and delay in seeking medical treatment can be a red flag. This was supported by another staff nurse, who met a patient with a fracture that did not correlate to the history given by carer.
In addition, participants indicated that they looked at the presentation of the injuries itself, for example, an atypical fracture such as a spiral type of fracture, or an atypical place for abrasion such as at the posterior triangle of the neck or the inner thighs which usually happens when a child is being sodomized, or even specific pattern of injuries such as a buckle-mark, a cigarette mark, or a pinch mark were noted as ‘red flags’ for abuse. Signs that showed intracranial bleed were also considered a ‘red flag’ for abuse such as sudden seizures in a previously healthy child and an upper neurological sign such as hypertonia.
In terms of neglect, one nurse focused on the hygiene aspect of a child in order to detect neglect. It should be noted that severe presentation of unhygienic features and severe malnutrition is usually picked up as a sign of neglect. Another medical officer added that immunization record and the state of nutrition of the child can also be used to detect neglect.
In terms of psychological and emotional abuse, the refusal that one child showed to his or her perpetrator is considered as an important indicator of child abuse as noted by many of healthcare workers that were interviewed.
Only a few participants highlighted the fact that abuse can be psychological, neglect or emotional. In contrast, a high proportion of participants emphasised more on physical abuse.
Subtheme 2: Sources of signs of abuse
Although most of the healthcare workers did not mention the importance of sources of signs of abuse, most of them noted that the people; either teacher, parent, police officer who brought the child to the hospital due to their suspicion of an abused.
This role of teachers and authorities in recognizing child abuse in the community is vital as a nurse mentioned a case encountered where the teacher detected signs of neglect in a child, thus the police officer was contacted. One specialist stated that unless anyone close to the child such as their teachers, their neighbours, or their relatives played their part in reporting child abuse cases, these kinds of cases would continue to be underreported and undetected in the clinical setting.
A specialist mentioned that conflicts between parents tend to complicate cases. They tend to manipulate the system to accuse the other party as the perpetrator in order to take full custody of the child. And to complicate the case even more the parent request for clinical examination to be done by the medical officer so that based on the clinical report they can make a police report. Therefore, sources of sign abuse can still be assessed depending on case by case nature to determine the intent of the person bringing the child in for clinical examination.
Key theme 2: Knowledge
Participants were posed several questions regarding their understanding on what can be defined as child abuse in their own words as they did not need to provide a full textbook definition of child abuse. Regardless, most of them struggled to provide a full definition of child abuse and resorted to examples of child abuse instead as shown in subthemes discussion below. Understanding of child abuse affect their capability in identifying children who are potentially at risk of being abused which are discussed further in the subthemes below.
Subtheme 1: Defining child abuse
Most healthcare workers were well-informed about the definition of child abuse and some were aware on the different types of child abuse such as physical abuse (bruises, fractures, etc.) mental abuse (change in attitude, verbally abused, etc.), and neglect (malnourished, unhygienic, etc.). One doctor mentioned that any harm that came to a child with intention is a form of child abuse. But most participants defined child abuse frequently as physical as opposed to other types of abuse. Some of the participants found it hard to separate the physical abuse and neglect completely.
One medical officer mentioned that true abuse and true neglect falls on a very thin line as a mother may take her eyes off a child momentarily and if the child would have fallen, the question on whether that is considered a form of neglect as well.
A high proportion of participants claimed to know types of abuses other than the physical ones but feels that more training is needed in order to identify these abuses as there are concerns on misdiagnosing. However, the difficult decision to diagnose neglect has been an issue even for those who have been dealing with abuse cases for such a long time. It is not surprising that many new junior medical officers are often not able to make the call, hence, would refer to their supervisors for guidance. Child abuse cases were not commonly found in the hospitals where this research was conducted. Some said that in a month maybe around 5% of children came with injuries consistent with abuse. Therefore, even though these healthcare workers knew the text-book signs of child abuse, many did not have enough experience when it comes to recognizing the signs, especially the non-physical signs.
Some of the participants noted that emotional and psychological abuses were often subtle and easily missed. Thus, there are demands on awareness to be created so that the probability of missed cases could be lowered. As mentioned by a medical doctor that feels that clinicians are failing children for not being able to detect the subtle signs and symptoms of neglects or emotional abuses unless they have the awareness. Many healthcare workers also based on their own intuition and their own experience in dealing with child abuse cases and making reports instead of consistent training.
This could be problematic especially for the junior participants and junior nurses who were not experienced enough in recognizing signs of neglect or abuse. This is where the role of training should come into a place where the junior workers could be educated on picking up signs of neglect or abuse so that in the future, even the junior medical professionals can report a case to the police.
Subtheme 2: Inadequate training and availability of training
While some training sessions were made available in these hospitals, most of the healthcare workers needed to wait for their turn to participate in such events. The frequency of such training was also inadequate to accommodate the increasing number of healthcare professionals that are new within the department. As explained by one of the specialists, the ministry is unable to provide enough fundings for these courses, thus some may fund themselves to attend courses. Apart from lack of funding, other reasons of not going to training was given such as not having enough human resources in their department to take charge in their absence, and also not having an available place in the training course.
For those who are interested in understanding more about child protection, or recognizing signs of child abuse in the clinical setting, they opt for self-directed learning where they would find their own sources of information either through medical textbooks or online journals. Again, this depends on their initiative to find the appropriate materials to enhance their knowledge and skills. If not, they will only learn through hands-on experience from the clinical setting or through direct teaching and supervision by their superior. This could be an advantage or disadvantage because it depends on how much transfer of knowledge had transpired within the setting, some might gain more while others not so much. Consequently, it creates a knowledge gap amongst healthcare professionals.
Subtheme 3: Content of training
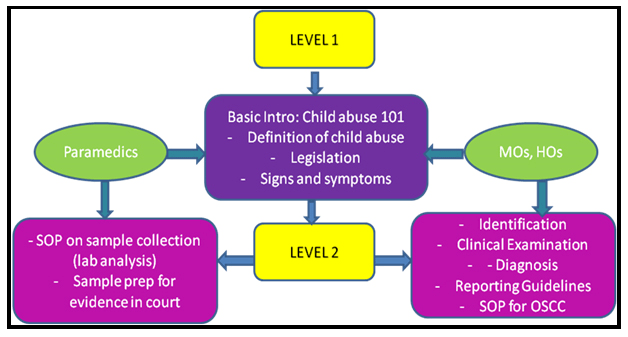
According to the professional healthcare workers interviewed, the content of the current training included a basic introduction on child abuse (definition, signs and symptoms), the procedure needed to be done in dealing with child abuse, the policies, and so on.
As stated above, paramedics (staff nurses and medical assistants) are in charge of supporting and assisting medical officers in handling child abuse cases. They are also in charge of collecting evidence for processing and to produce in court and to the police. Hence, most training for these paramedics are only limited to understanding procedures in collecting and processing specimens for the purpose of producing evidence in court, if the child abuse case would proceed to the court.
II. Key theme 3: Risk Perception
Healthcare professionals were not sure how to distinguish between child abuse and disciplining a child because as it is perceived as an extremely thin line. The act of disciplining a child physically is the norm in the Malaysian culture. However, this could lead to the possibility of a lot of missed signs of child abuse. One of the participants interviewed shared her opinion on disciplining a child where she said that physical acts towards the child such as hitting them in order to discipline them was fine as long as it did not lead the child to be bruised, wounded or to the point of the child being unconscious.
There were also issues where the healthcare workers were not sure where to draw the line when it came to distinguishing between an abuse and an accident. Where the case of abuse by intracranial bleeding can be misdiagnosed as it could be an accident. One participant mention that caretaker might accidentally shook the baby in order to make him or her to sleep, due to lack of experience and knowledge of a proper childcare, causes the baby to suffer intracranial bleeding from the shaking.
These findings suggest there is a real lack of awareness within hospitals as to what defines neglect and abuse, and confirms there is a definite grey area that needs to be addressed so that all findings of child neglect and abuse can be defined, standardized and identified.
Another issue that was discovered was the appropriate time toward non-physical abuse, especially neglect.
One doctor took this matter into the light where she said that Malaysia is a country where multiple cultures and beliefs are allowed to be practised freely. However, some of the cultures involved not believing in immunization by which it denies the right of the child to access healthcare services (such as treatment) and this lead to the medical officers not knowing how to act since the act of reporting it would interfere with the basis of human rights while the act of not reporting it would mean they had become an accessory to neglect.
Again, all of these are the effects of not having a high suspicious index in order to pick up children coming in with presentation that raises certain “red flags” due to lack of knowledge in understanding in depth what is child abuse.
III. Key theme 4: Awareness of detection tools
Most healthcare workers that were interviewed were not aware of the presence of child abuse detection tools in the hospital. However, participants indicated that checklists were in use in the participating hospitals. Most of the checklists that are currently present are those that provide guidelines regarding the procedure (Standard Operating Procedure (SOP) for One-Stop Crisis Centre(OSCC)) of dealing with child abuse such as taking samples, making a report, and a clerking sheet which is used mainly by medical officers and specialists whereas case report is used by nurses. Again, this SOP will only come into play when the child has already been suspected of being abused by the attending medical officer before full examination to determine the suspicion is being carried out in the OSCC.
When asked to comment on the benefits of screening tools, the majority of participants gave a lot of positive attitudes and agreement with the development of a screening tool for child abuse as it can be used to standardize the screening for all children attending the department regardless of their presenting symptoms. They will be screened in or out based on the checklist/screening tools. As such healthcare professionals would benefit a lot from having such a tool, especially for new staff in the frontline such as medical assistant, as the assessment is based on the tool rather than their own perception or high index suspicion. This is of great importance as it will potentially save a life of a child.
In regards to what should be the content of a checklist for a detection tool, most healthcare workers mentioned the importance of looking at physical signs such as bruises, atypical fractures, foreign cutaneous marks, body weight and also radiological images that could suggest a possible atypical injury. The inconsistency of the history and the child’s injury was also suggested as one of the most important components of the detection tool. Some of the healthcare workers also recommended including the family history because certain family situations could lead to child abuse. The participants mentioned about family history composing of drug abuse and forensic records.
Major Theme 2: Determinants of Motivation of Healthcare Professionals
Key theme 1: Attitude
Most healthcare professionals had adopted discipline and professional attitudes when dealing with patients of all ages coming in for treatment. But the different responsibilities and authorities given to different levels of personnel divided the healthcare teams where it affects roles and task performed. As such, only medical officers and specialists are given the authority to diagnose and report child abuse cases whereas nurses and medical assistants are given the task to assist them. Therefore, most of the time nurses and medical assistants tend to not alert a case to the attending medical officer even though they suspect that the child might be potentially at risk of abuse for fear of overstepping their boundaries or not being their responsibility as discussed and shown in subthemes below.
Subtheme 1: Responsibility
Many of the medical officers mentioned that they felt responsible to report a case, especially if the signs of abuse are obvious, such as fractures, bruises or intracranial bleed.
Some would refer the case to the Suspected Child Abuse and Neglect (SCAN) team if they felt that something is not right with the child regardless and would make a police report once the case is diagnosed as suspected child abuse. However, many medical officers are still reluctant to make a report if they only suspect that the child had been abused if the child came in with subtle signs.
As for nurses and medical assistants, the majority feel the responsibility to inform or report to the attending medical officer if they have the suspicion that a child may possibly be abused. One of the nurse that was interviewed mentioned she prefer to report and be wrong about the suspicion rather than letting a child being abused and not attended to.
Although sometimes they are worried that the diagnosis might be wrong, but at least they had fulfilled their responsibility to report a case even with the slightest suspicion. But there are those who work just to make a living, but lack passion in pursuing the best interest of the patient. They would not go out of their way to talk to the patient and really find out whether the patient is actually being abused, because most children would not talk or say anything if they are abused, especially in the presence of the perpetrator themselves. Therefore, nurses play an important role in eliciting information outside the consultation room.
Subtheme 2: Work culture
The working culture in the government hospital is that they are given a set of task and role to undertake in which they have to follow. But what they are expected to do may not transpire in their work. For example, one of the nurses mentioned that they were instructed to take patient’s vital sign and input into the system whether the patient came in with an injury or not hence they need to check “trauma” into the system. Unfortunately, this was not done most of the time. This is due to lack of the feeling of responsibility towards the patient.
Subtheme 3: Negative aspects
In certain cases, some participants felt it was difficult to detect child abuse because of the child is reluctant to inform what had happened to them. If they were abused by one of the parents, they would not tell what actually had happened and who had done it to them because of the fear that the parent might be put away.
There is also a fact that in most child abuse cases, the child will be taken away from his/her family and put into the care of a protection officer and placed within a government institution if there is no next of kin who can take care of the child. Hence, the child will be placed in the institution throughout the investigation period until the case is being heard in court. As such, the child will be in the system where the child will not be able to enrol in school due to being in transition. The experience of going through such process could be scary and detrimental for a child who is separated from his/her family for the first time not knowing what is in store for them next because court cases could take months. In this instance, the outcome for the child if suspected of being abused may not be better.
Key theme 2: Social influences
It is important to understand what drives and motivates healthcare professionals to alert a case or report a case suspected of abuse.
Subtheme 1: Internal support
The healthcare system itself provides support to healthcare professionals by providing clear guidelines and procedures and who is responsible for making a diagnosis and report when there is a case suspected of abuse. Senior officers such as the head of department and specialists also provide ample of support to the subordinates by reminding and encourages staffs to highlight a case to the attending medical officer if he/she has a high suspicion that the child may be potentially abused.
For medical officers, if they are uncertain whether to diagnose a child with suspected of being abused can always refer the case to the SCAN team or consult with a specialist before proceed in making a diagnosis and report. Every hospital will have a SCAN team on standby if any child abuse case is detected.
One of the nurses supported the same sentiment when asked about whether they are being encouraged to inform the medical officer if they are suspicious of a child being abused because of was the child behaves around the parent (eg. body language, timid and quiet). Having a written SOP and guideline in managing suspected child abuse and neglect case also helps to encourage healthcare professionals to make a report knowing that everything is formalised and documented, pieces of evidence are collected properly, etc.
ii. Subtheme 2: External support
Apart from the Department of Social and Welfare (DSW), the Royal Malaysian Police provides 24-hour support to the hospital ETD.
iii. Subtheme 3: Lack of support
Most participants mentioned repetitively during the interview is that the Department of Social and Welfare (DSW) although provide external support in handling child abuse cases in the hospital, unfortunately, they are only available during office hours and not able to attend any cases after that or during the weekend or public holidays. This proved to be challenging and difficult for the healthcare professionals because at certain times they would receive cases over the weekend in which they had to admit the patient for the duration of the weekend until Monday before the DSW officer is able to attend the patient. Although there is a 24 hours hotline that they can call and SMS to inform about a case, but the DSW officer will only attend the case on the next working day and during office hours. Even the Medical Welfare Officer (MWO) is only available during working hours to interview and take the further history of the patient and liaise with the DSW officer.
It was noted that sometimes when the patient had to be admitted during the long weekend, there is a possibility that the patient may abscond and return home with the family and suspected perpetrator without the knowledge of the hospital administration. Even with tight security and monitoring, the patient can still leave the hospital without raising an alarm.
Major Theme 3: Determinants of Action of Healthcare Professionals
Key theme 1: Dealing with child abuse cases
There was not much difference between the three hospitals when it comes to dealing with child abuse cases. Most of the healthcare workers in all hospitals had similar processes and Standard Operating Procedures (SOPs) in place in managing child abuse cases. The management of the child started from when the child was brought in by another person to the emergency department.
There are three zones in each hospital: the Green Zone, the Yellow Zone, and the Red Zone. All severe cases which require resuscitation are sent to the Red Zone. The less severe cases are sent to the Yellow Zone while mild cases are sent to the Green Zone. Patients who came into the ETDs are first seen by the medical attendants at the first triage.
At this stage, the medical assistants (MAs) would decide the severity of the child’s complaint and would send the child to their respective zones. For example, if the child is able to walk, the child will be sent to the green zone where their vital signs will be taken by designated nurses stationed at the secondary triage. Once their vital signs are recorded, they will have to wait for their turn before being seen by the medical officers in one of the consultation rooms available. Once they are seen by the medical officer, the medical officer would ask them what their complaints are and then proceeded with the clinical examination. If during one of these stages the medical officer suspects the child of being abused, the child would be sent to the OSCC.
The Suspected Child Abuse and Neglect (SCAN) team would also be informed. One of the specialists informed that most hospitals would have at least one SCAN team and the members of the SCAN team are a pediatrician, gynaecologist, medical officer from both fields and a medical social worker from the hospital.
The child will be attended based on the injury that he/she had sustained. Any physical injuries will be seen by a Pediatrician, likewise, any sexual injury will be observed by a Gynecologist and any sodomy cases will be observed by a surgeon and so on. From the OSCC, the child will be admitted to the ward and the history will be recorded again. Children who are under the age of 12 will be admitted to the pediatric ward. While those who are 13 years above or those suspected of being sexually abused will be admitted to the Obstetrics and Gynecology (O&G) ward. At the same time, a police report will be made by either the medical officer who diagnosed the case in the ETD or by the SCAN team. The Department of Social and Welfare (DSW) will also be notified by the SCAN team.
One of the medical officers mentioned another way for a child to be admitted into the OSCC other than being suspected by a staff in one of the zones.
In this case, if a child came in with a police report or a teacher who suspected the child was abused, the child would immediately be taken into the OSCC for further evaluation. The role of emergency department ended when the child was sent up to the ward to be seen by the SCAN team. After being sent to the OSCC, the child would be admitted to the ward. If the suspects who abused the child were the parents, the child would be separated from their parents. According to one of the medical officers interviewed, they would also notify any family members to inform them the state of the child. Afterwards, the case would be seen by the police and would be taken to court. Once a court order had been obtained to put the child under the care of a protection officer, consequently, the social welfare department would find a proper placement for the child so that the safety of the child would be secured. As such, the child is placed in a shelter home under the guardianship of the department throughout the court hearing.
i. Subtheme 1: Barriers
Several professional healthcare workers mentioned a few barriers they encountered when trying to report a child abuse case. One of the commonest hardships that they encountered was the refusal of the parents themselves to report a case.
Other than that, parents were also scared that they would make a mistake by pointing their fingers to the wrong person who might or might not be a perpetrator. Other reasons including not having enough evidence, facing a system default where parents had to wait too long to the point that they may abscond, and also not wanting to face the hassle of having to go to the court. Others may be afraid that if their partner or spouse is being arrested, they would lose the breadwinner of the family as most of them rely on their partner or spouse financially.
Other than the refusal by the parents or guardians, there were also many system limitations identified especially in the social welfare department. Most of the professional healthcare workers expressed their dissatisfaction towards the service of the social welfare department. The current social welfare department only worked during the weekdays and only responded to cases during office hours. They also did not take any case during the weekend. This lead the delay in placing the child into a proper placement and the child ended up having to extend their stay in the hospital.
This is probably due to the lack of manpower in the department, as mentioned by one of the medical officers. One medical officer also highlighted that in the emergency setting, it was difficult to detect a child who was emotionally abused or neglected, this was justified with the constraint of time.
This is notable since there is a high number of patient influx coming into the department ranging from hundreds to thousands per day which can be daunting as time spent for each patient is roughly around five minutes. During that time, the main task of any healthcare professional is to treat the patient first. Communication skills to extract certain information are not apparent as it requires a lot of specific training to elicit such information, especially from children. This it would seem is still lacking in the current system and quite visible among the healthcare professionals. In addition, in order to gain the trust of the patient, medical officers need to build a good and strong rapport, which requires time and unfortunately, that would not be possible in the ETD setting.
Other than that, there was also a stigma in Malaysia surrounding child abuse. Child abuse in Malaysia is not something that is being widely explored, therefore, the detection or suspicion of child abuse could lead to parents being offended.
ii. Subtheme 2: Action Plans
The Malaysian Law stated in the Child Act 2001 that any medical officer, who suspects or sees a child that might have been harmed or abused, must report the incident to the authorities. Any medical officer who fails to do so will be considered of having committed an offence.
This law is being brought on by one of the medical officers:
However, they would refer to the specialist first before taking any action. Discussions would be made between the medical officers and the specialists before they reached a confirmation that the child had been abused. The house officers, however, were not allowed to make a police report by themselves. One medical officer justified this situation in the interview by saying that lawyers will be questioning the doctor’s experience, thus to make a solid case inexperienced doctors are dismissed.
The nurses were aware of their duty to assist the medical officers who are dealing with child abuse cases. Most of them reported that they would inform any medical officers if they discover any signs of abuse in a child who came in for consultations that were missed by the medical officers. One medical officer mentioned, however, that in the hospital setting, most subordinates would not voice their opinion to their superiors and the superiors rarely take an advice from their subordinates.
Medical assistants also face the same situation, although they are the frontliners and the first ones to be in contact with these children, they are powerless to make any report. The best they can do based on their jurisdiction is assign the child straight to OSCC for concerns and suspicions that the child might be abused. As such apart from medical officers or specialists, other healthcare professionals are not allowed to make a police report. If unsure whether to diagnose a case of suspected child abuse, medical officers would have to consult their specialists or the SCAN team for further action.
DISCUSSION
Medical healthcare professionals, being the first point of contact and frontliners in the medical setting, provides an opportunity for children potentially at risk of being abused and neglect to be identified. During the course of the interviews, the researcher found that a two-tiered system exists within the healthcare setting, with medical practitioners on one end and paramedics (such as nurses and medical assistants) on the other (Figure 2).
Figure 2. Flowchart of Patient Coming into the ETD
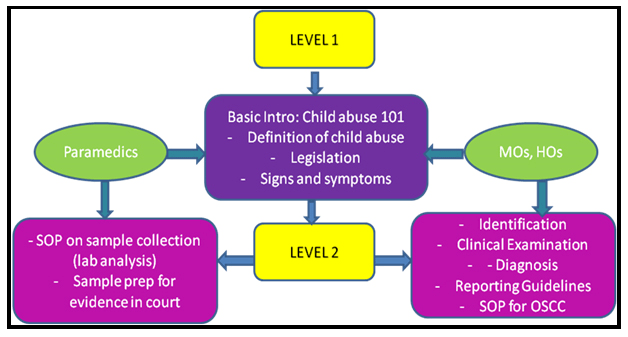
Often enough, paramedics were reluctant to raise any warning signs to the attending medical officer if he/she found that a child coming into the ETD could be potentially at risk of being abused/neglect. There were contradicting statements coming from both ends whereby medical practitioners said to have encouraged paramedics to bring up warning signs of abuse to them but observed that most of the time none of the nurses or medical assistants would do so. But when nurses and medical assistants were prompted on whether they would bring it up if these warning signs occur, most of the time they said that they would say yes but in practice, they would not do so. It could be because they felt that they might be overstepping their boundaries as their role is mainly to assist and provide support to attending medical officers or could be because they don’t have the authority to diagnose hence may not have adequate knowledge to do so. The same sentiment was reported in the study done by Lazenbatt and Freeman, where they found that nurses may also feel some discomfort and anxiety from dealing with CAN cases and they might have fears from the consequences of their actions.16
It could also be the fact that being paramedics in the ETD, they are usually extremely busy carrying out their respective duties and tasks that are at hand, any other additional tasks would be an added burden and overwhelming for them. It should also be noted that because of the standard operating procedure in the ETD clearly stated what their roles and responsibilities are, any other instruction given verbally usually does not carry much weight. Anything that is not stated in the SOP, protocols or guidelines might also incur repercussions, which also added to the lack of motivation for paramedics to take on the initiative to raise the alarm in the first place. There should not be any issue or concern about raising the false alarm because if all children are being screened in the first place, there are fewer chances of children who may fall under the radar.
In other countries such as Australia, nurses’ duties to report CAN are expressed in legislation, or in occupational policy documents.17 The Australian Nursing & Midwifery Federation (ANMF) also had issued a policy statement in 2007 which clearly stated “It is essential for anyone working with children or young people to recognise their vulnerable status and the special protection they may require if they appear to be at risk”.18
Similar legislation and systems are being implemented in Taiwan where the nurses have their own position in the healthcare settings and have their own voice in reporting CAN case within their respective setting.
Therefore, it is important that paramedics are also held accountable to provide more than just assistance and support in terms of services to patients (screening in the first triage and taking vital signs in the second triage). Being frontliners as the initial first contact in the first and second triage, they play a very important role but are currently heavily underutilized. This should be done at all hospitals and if possible to be included in an addendum to the current SOP. So that it can be formalized in such a way that identifying child who are potentially at risk of neglect abuse, and bring it to the attention of the person in charge are also part of their duty and not just those who are assigned to the SCAN team.
Likewise, attending medical officers carry the responsibility to identify children who are suspected of neglect or abuse, but they also need support, encouragement and empowerment on their vital role in identifying children who are at risk of neglect or abuse. This would encourage them to spend extra time on children whom they have high suspicions of potentially being abused and neglect.
I. Knowledge Gap
There is a gap in terms of understanding early warning signs of abuse among the healthcare professionals.
Some of the points highlighted during the interview were:
1. Inadequate training on CAN/ child protection;
2. No standardized training across all hospitals on CAN/ child protection;
3. Different level of training provided for medical officers and paramedics;
4. Uncertainties in identifying in the level of severity of neglect for diagnosis;
5. Inability to ascertain emotional and psychological abuse masked by other presenting signs and symptoms;
Even for those who are at a senior/specialist level were still unable to confirm that throughout their career they had never missed a sign of abuse. The same medical healthcare professionals reiterate again that more specialized training is needed focusing only on CAN or child injury prevention or protection. Paramedics (nurses and medical assistants) should be included in all levels of training and emphasized on their role in identifying and reporting to their superior of any children who are potentially at risk of being abuse in their respective setting. This would enable them to receive the support, encouragement and empowerment to undertake their duties in promoting awareness on the CAN in the clinical setting.
Therefore, if several warning signs have been raised in the first and second triage there is ample enough evidence for the attending medical officer (MO) to do further examination on the child away from the suspected perpetrator(s) (eg. parents, caregivers or any other family members). This would set a precedent to inculcate the culture of screening in all children presented at the ETD as oppose to screening out.
Therefore, it is important that paramedics, MOs and HOs are able to attend a more specialized training looking at more in depth information of child abuse and neglect detection regardless of their position. For example, in the United Kingdom (UK), each hospital has the responsibility to provide adequate safeguarding children training. In King’s College Hospital, they are responsible in providing all clinical staff with child protection awareness training. They also ensure that all staff are given information about the importance of child safeguarding and how they can support the needs of vulnerable children and young people. They also provide dedicated help through their specialist Safeguarding Children team to identify, protect and care for those at risk. And they also work with General practitioners (GPs), social services and other professionals to ensure the needs of vulnerable children and young people are met.19
Providing adequate to specialise training is important but providing regular training is also critical to the development of a skilled medical healthcare professional and to achieving outcomes of safety, permanency, and well-being for children entrusted to the public health system. Having this knowledge not just assist the technical aspect of identifying children potentially at risk of abuse, but it also increases the level of awareness of such case but also increases one’s level of suspicion if they do come across cases that may potentially be a CAN case, hence, increase the sensitivity or obligation and responsibility of officers in the ETD. And this cuts across all levels let it be paramedics or medical officers or specialists and consultants.
II. Community and Work culture
Organisational culture in the healthcare setting has been long discussed in the Western world, but not so much in the ASEAN region. According to the Organizational Culture Profile (OCP) instrument, performance orientation culture is shaped by the following characteristics: enthusiasm for the job, results orientation, highly organized employees and high-performance expectations.20 Supportiveness and constructive organizational culture are also needed to generate a sense of collectivity and emotional attachment that develops a community focused on organizational goals. Working as a team encourages more exchange of information and because of the frequent contacts, members are aware of who possesses the knowledge to solve specific problems.20
But what was found and observed during this study was that nurses were less enthusiastic with their work and more dependent on the senior staff nurse when encountered with complex cases such as child abuse and neglect cases. This was noted visibly among junior nurses, who were highly dependent on community nurses who manage the OSCC when it comes to SOPs and guidelines in handling CAN cases. Because the fact that they are on rotational basis, they would not have the opportunity to undergo any OSCC training, hence, did not feel the need to undertake additional initiative to understand more on CAN.
Community culture also acts as a barrier for nurses to respond towards CAN cases. This is particularly true especially when they have more experience working with children and had dealt with a lot of CAN cases as it was found in this research. While other nurses considered CAN to be a personal and family issue in which they had no role or say, hence, the reluctance to highlight the matter and bring it to the attention of MOs or attending physician.21 This is especially true within the Malaysian cultural context, which is quite similar with other Arabs and eastern culture where child-rearing can be it is considered socially acceptable for parents to practice physical punishments and yelling to their children as a normal part of child-rearing.22,23
III. Screening tools for child abuse
This study managed to establish that there are no screening/ detection tools being used at the ETD or any other clinical department in the public hospital as of current. What is currently available is Form 9, which is used by MOs once a child is being diagnosed as CAN case and is brought into OSCC for further examination and investigation. Prior to that, there are no checklist or screening tools being used at the first triage or second triage at the ETD.
This study found that most healthcare professionals interviewed were not aware that screening or detection tools for child abuse are available and being used worldwide. Only specialists in the ETD and paediatrics were aware of such tools but were not sure whether they were being used in the ETD or any other clinical departments in the hospital. Currently, there are several screening/detection tools being used in the US, Europe and Australia. Some of the most well-known tools are the SPUTOVAMO, SPUTOVAMO-R and the most recent one SPUTOVAMO-R2 (it does not only look at the injury, but also at the interaction with parents and child) and is used widely in the ETD. The ESCAPE orm is also another instrument which is widely used in the ETD. There are other tools/ instruments that can be used such as the ISPCAN Child Abuse Screening Tools (ICAST), but this instrument is not being used at the ETD, but more in the community and homes.
For healthcare professionals, having a standardized screening/detection tool would assist them greatly in identifying children who are potentially at risk of abuse in the ETD especially at the first and second triage, where paramedics are stationed as shown by Louwers et al in the study they conducted in 2014.24
LIMITATION OF THIS STUDY
The main challenge was scheduling times for interviews, due to participant’s lack of time available, especially during working hours. Almost all of the interviews were conducted in the ED itself. The ED was very hectic, noisy and full of patients requiring emergency care, families, therefore was not a conducive environment to conduct full length qualitative in-depth interviews. As such, there were plenty of distractions (red zone emergency cases, patient required resuscitation, enquiries from patient’s family, etc.) that affected the quality time for the researcher to elicit in-depth responses and relevant information, as some interviews were conducted in a hasty manner. Another limitation is that this study was done only in three major public hospitals. If the study could be expanded to other hospitals in order to obtain more representative sample of hospitals throughout Malaysia, including urban, rural and regional areas.
Lastly, given the small proportion of CAN cases, some participants’ lacked experience and training in dealing with CAN cases. This may result in some biases in the information extracted during the interview.
CONCLUSION
Other medical healthcare professionals such as nurses and medical assistants or also known as paramedics although do not have the mandate to diagnose or report of CAN cases, they need to have the basic knowledge and awareness on CAN. They should also be encouraged and empowered to take an active role in identifying or raising the ‘red flag’ with high index of suspicions so that these children can be brought in for further examination by medical officers. Likewise, those who had been in the force for the longest would have more experience in dealing with CAN cases, they are more skilful aware and empowered to bring the matter to the attention of the attending medical officer compared to those who are quite new in the department.
Amongst medical healthcare professional has some impact in creating awareness on CAN in the clinical setting. Specialised and intensive standardized training in child protection and awareness on CAN are needed and should be made available for all healthcare professionals to attend and improve their knowledge and understanding of the differentiation between accidental and non-accidental injuries as it present at the ETD. And these training should be on-going with reviews and updates on the latest information on detection of CAN cases.
The healthcare system itself needed to be enhanced and strengthened to ensure that strategies are in place such as screening tools, checklist are available to assist healthcare professionals in making the diagnosis and speed up the process of identification and reporting more efficiently. Early diagnosis of CAN is important, as without early identification and intervention, about one in three children will suffer subsequent abuse. Based on the findings of this study, there is a need to implement such tools in the ETD. Because these tools are standardized, it can be used cutting across all hospitals. There are several tools that can be used for pilot implementation (eg., ESCAPE form, SPUTOVAMO-R), therefore, it is envisaged that these can be done as a post-doc research study in one of the hospitals.
ACKNOWLEDGEMENTS
The authors would like to thank the Director General of Health Malaysia for his permission to publish this article and would like to acknowledge Head of Departments, Dr Sabariah Jamaluddin of Sg Buloh Hospital, Datuk Dr Alwi Abdul Rahman of Selayang Hospital as well as the Dr. Rohaizah Binti Borhan of Serdang Hospital. And Dr Hazlina Mohd Noh and Dr Noor Azyati Mohd Yusooff for their kind assistance during data collection at their respective hospitals.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.