INTRODUCTION
Human papillomavirus (HPV) infection is the most commonly occurring sexually transmitted infection (STI) in the United States. Approximately, 79 million women in the country are infected with HPV, and 14 million new infections occur annually.1 More than 80% of American women will have contracted at least one strain of genital HPV by the time they reach 50 years of age.2 Sexually active women below the age of 25 such as college students have the highest rates of genital HPV infection.3 College students are considered to be a high-risk group for contracting STIs because they are likely to have multiple sexual partners (MSP) and have unprotected sexual intercourse.4,5
While HPV infection is usually benign or asymptomatic, it can result in serious health consequences, such as genital warts and even cervical cancer.6 HPV infection is necessary for cervical cancer to develop.7,8 Cervical cancer is the second most commonly occurring female-specific cancer worldwide, accounting for about 8% of total cancer cases and total cancer deaths among women.9 This disease claims 2,66,000 lives worldwide10 and over 4,217 in the USA annually.11
HPV vaccination is an effective method of preventing cervical cancer. Three HPV vaccines namely; Gardasil, Cervarix, and Gardasil-9 are licensed to combat cervical cancer in women in the USA.12 The HPV vaccination is recommended for males and females of ages 11 to 26-years-old.1 Gardasil and Cervarix have been shown to be efficacious, safe, and well-tolerated.12 Gardasil reduced the combined incidence of infection with types 16 or 18 by 94.5% in participants.13 The protection against types 16 and 18 lasts for at least eight years after vaccination with Gardasil and more than 9 years after vaccination with Cervarix.12 After the introduction of the vaccines, the prevalence of HPV infection (types 6, 11, 16, and/or 18) fallen by about 88% among vaccinated women in United States, and the annual cost of cervical cancer treatment decreased from $6,000 million to approximately $400 million in the country.14,15
However, about 60% among college-aged women did not receive HPV vaccination in the USA.16 This may be due to inadequate understanding of HPV infection, cervical cancer and the vaccine. As the American college students are at high risk for HPV infection, their sufficient awareness and accurate information about cervical cancer, HPV transmission, and its prevention are imperative to increase HPV vaccination coverage. Therefore, the objectives of this study were to examine the level of knowledge about HPV, cervical cancer and its association with HPV vaccination among college students in the USA.
METHODS
Study Participants and Sample Size Determination
This study was conducted at a large multiethnic public university in the state of Florida, in January-May 2013. In 2013, there were 21,287 female undergraduate students in the Institute. There were 55 required university core courses offered in the institute in 2013 spring semester in the areas of Global Learning, English Composition, Humanities with Writing, Quantitative Reasoning, Social Inquiry, Societies and Identities, Natural Sciences, Life Sciences, Physical Sciences, and Arts. Out of the 55 courses (which we treated as clusters), 10 courses/clusters were randomly selected for this study. On average there were 42 students registered for each course selected for this study. All female students who were attending classes in the aforementioned courses during the study period were eligible for this study. In those clusters, a total of 151 female students present on the day of the survey, were approached, and 141 female students completed the survey. The sample size (n=141) was determined based on the Rules of Thumb (n>104+m) for studying the relationships of an outcome with individual ‘m’ predictors as suggested by Harris, 1985 and Green, 1991.17,18
Questionnaire
The questionnaire consisted of 24 items, most of which were multiple-choice questions in which students were asked to choose one among several predefined categories. Items were selected from the previously published peer-juried literature that assessed knowledge about HPV and cervical cancer.19,20,21 The questionnaire was divided into four sets. The first set contained questions on socio-demographic variables (e.g., Year spent in college, Major subject, Race/ethnicity). The second set consisted of items used to assess information about the participants’ knowledge about HPV and cervical cancer and the participants’ primary source of health-related information (Sexual activity is a risk for cervical cancer, sexually transmitted diseases (STDs) and MSP are risk factors for cervical cancer, Human Papilloma virus causes cervical cancer, Cervical cancer is preventable). The third set contained items asking participants about their own preventive behaviors concerning HPV and cervical cancer (e.g., When did you have a most recent medical check-up from the day of the survey?). The fourth set consisted of items used to assess if students received an HPV vaccine or will consider receiving in the future (considering receiving the vaccine in the future) it in the future (e.g., Received HPV vaccine at least one dose).
Data Collection Procedures
Before data collection, the course instructors briefly introduced the survey team to their students. There were five graduate students that were trained to administer the questionnaire. After the instructor introduced the survey, one of the two team members described the research objective and importance of the study, confidentiality and that no personal information is part of the survey. Then, students who agreed to participate in the study completed a questionnaire in a period of 10-12 minutes at the beginning or end of their class. By the Course Instructors’ plan either at the beginning or during the end part of the class the survey was conducted. In the case of students, who were attending two courses, data were collected only once when they were contacted for the first time.
Data Analysis
The data for this study were analyzed in the Statistical Package for the Social Sciences (SPSS).22 The outcome variable was HPV vaccination status (0=not received any dose or 1=vaccinated at least partially). The explanatory variables were age (continuous), health insurance (0=no or 1=yes), race/ethnicity (non-Hispanic White, Hispanic white, Black, and other) and knowledge about cervical cancer (0=incorrect or 1=correct). The knowledge about cervical cancer was assessed using four items: a) Sexual activity is a risk for cervical cancer; b) STDs and MSP are risk factors for cervical cancer; c) Human Papilloma virus causes cervical cancer; and d) Cervical cancer is preventable. Responses for each item was recorded as ‘incorrect’ or ‘correct.’ For each participant, a composite knowledge score was calculated by adding their responses to the four items. Total scores can range from 0 through 4, and the composite score achieved an acceptable reliability measuring knowledge (Cronbach’s alpha=0.68, p=0.0001). Then a dichotomous variable was created from the composite knowledge score (0=knowledge scores less than the median; 1=knowledge scores greater or equal to the median) to be included in the regression models. A Chi-square test was used to test the relationship of race/ethnicity, health information sources, health insurance status with annual health checkup and HPV vaccination status. A multiple logistic regression model was used to estimate the association between participants’ knowledge about cervical cancer and HPV vaccination status.
Ethical Consideration
The Institutional Review Board approved the study, and consent was obtained from each participant. No personal information about the study participants (e.g., name, address, phone number) was recorded.
RESULTS
A total of 153 female students, who were attending 10 major courses in a Multiethnic Institute, were contacted. However, 12 students could not complete the questionnaire because arrived late in class, less time to complete the questionnaire, or had some other time commitment. Thus, the sample for our study consisted of 141 female undergraduate students. The response rate was 91.5%. The mean age of the sample was 21.7 years. The majority of the participants were non-Hispanic Whites (51.5%), followed by Hispanic Whites (30.8%). Higher percent (41.2%), of the students were in their junior year of college and the commonly reported (40.0%) majors were subjects in the health sciences. About 60% of the students did not receive HPV vaccine. Of those students who had not received an HPV vaccine, 68% listed a lack of trust, apathy, and fear of side-effects as reasons for not being vaccinated (Table 1).
| Table 1: Selected Sociodemographic Characteristics of the Study Participants and Health Seeking Behaviors. |
|
Variable
|
Categories |
Number |
Percentage
|
|
Year in college
|
Freshman |
31 |
22.8 |
|
Sophomore
|
23 |
16.9 |
| Junior |
56 |
41.2
|
| Senior |
26 |
19.1
|
|
Majoring in
|
Health sciences |
56 |
40.0 |
|
Basic sciences
|
38 |
27.1 |
|
Arts
|
30 |
21.4
|
| Business |
12 |
8.6
|
| Engineering |
4 |
2.9
|
|
Race/ethnicity
|
White (non-Hispanic) |
70 |
51.5 |
|
White (Hispanic)
|
42 |
30.8 |
| Black (non-Hispanic) |
14 |
10.3
|
| Other |
10 |
7.4
|
|
Health information source(s)
|
Online |
87 |
61.7 |
|
Print media
|
20 |
14.2 |
| Online (& others) |
18 |
12.8
|
| TV (& others) |
15 |
10.6
|
|
Top two major health issues*
|
STDs± & mental health disorders |
56 |
39.7 |
|
STDs± & overweight
|
49 |
34.8
|
| Mental health disorders & overweight |
36 |
25.5
|
|
Health insurance status
|
Yes |
101 |
71.6
|
|
When most recent medical check-up from the day of survey
|
Within 12 months |
54 |
38.3 |
|
In 13-24 months
|
55 |
39.0 |
| In 25-36 months |
18 |
12.8
|
| Never or do not remember |
14 |
9.9
|
|
HPV vaccine received at least one dose
|
Yes |
56 |
39.7
|
|
Reason for not receiving HPV vaccine
|
Lack of trust in effectiveness, fear of side-effects, or apathy |
28 |
68.3 |
|
Overaged or not sexually active
|
9 |
22.0
|
| Doctor did not advise them to receive the vaccine |
4 |
9.8
|
|
Considering receiving vaccine in the future
|
Yes |
25 |
29.4
|
| Note: *Students were asked to choose which two health issues they felt were most important for their age group.STDs±= sexual transmitted disease |
Annual Health Check-Ups and HPV Vaccination
Of 141 students, 39.7% of the students had received an HPV vaccine and 38.3% had undergone a medical checkup in the year prior to completing the questionnaire. The percentage of students who received an HPV vaccine was greater among those who attended an annual health check-up within the last three years from the day of the survey (43.8%) as compared to those who did not (15.4%) (p=0.04). The percentage of students who attended an annual health check-up during the three years prior to the survey were greater among those who had insurance coverage (93.1%) than those who lacked insurance (82.5%) (p=0.05) (Table 2).
| Table 2. Annual Checkup, HPV Vaccination, and Median Knowledge Score by Selected Characteristics of Students (n=141). |
|
Variable
|
Category |
Annual health checkup within the 3 years (%) |
Received HPV vaccine (%) |
Knowledge score ≥median (%)
|
|
Race/ethnicity
|
White (non-Hispanic) |
88.6 |
48.6 |
28.6 |
|
White (Hispanic)
|
90.5 |
35.7 |
33.3 |
| Black (non-Hispanic) |
100.0 |
35.7 |
35.7
|
| Other |
90.0 |
20.0 |
10.0
|
|
Health insurance status
|
Yes |
93.1* |
42.7 |
28.7 |
| No |
82.5 |
36.8 |
32.5
|
|
Majoring in
|
Health sciences |
92.9 |
33.9 |
35.7 |
|
Basic sciences
|
94.7 |
52.6 |
31.6 |
| Arts |
83.3 |
33.3 |
31.6
|
| Business |
83.3 |
33.3 |
25.0
|
|
Engineering
|
75.0 |
50.0 |
0.0
|
|
Health information sources
|
Online only |
90.8 |
36.8 |
32.7 |
|
Print media
|
85.0 |
40.0 |
25.0 |
| Online (& others) |
94.4 |
44.4 |
38.9
|
| TV (& others) |
86.7 |
53.3 |
13.3
|
|
Most recent medical check-up
|
Within 3 years |
— |
43.8* |
29.1*** |
| Never or do not remember |
— |
15.4 |
0.0
|
| Note: *p=0.05, **p=0.01, ***p=0.001 STDs & multiple sexual partners are risk factors of cervical cancer |
Knowledge about Cervical Cancer and HPV Vaccination
The mean and the median knowledge score of students about cervical cancer/HPV on the basis of four points was 2.87 and 3.0, respectively. Most students understood that HPV (75.7%) and having MSP and other STDs (83.0%) were each risk factors for developing cervical cancer. However, there were key areas of misunderstanding among participants. More than one-third of the students were unaware that cervical cancer is preventable. In general, the participants were not thoroughly knowledgeable about cervical cancer, with only 13.5% of participants reporting that they knew of all the causes of cervical cancer and 9.9% reporting that they knew about all the aspects of cervical cancer.
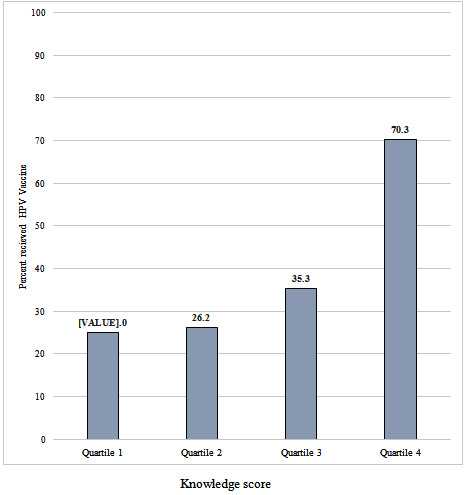
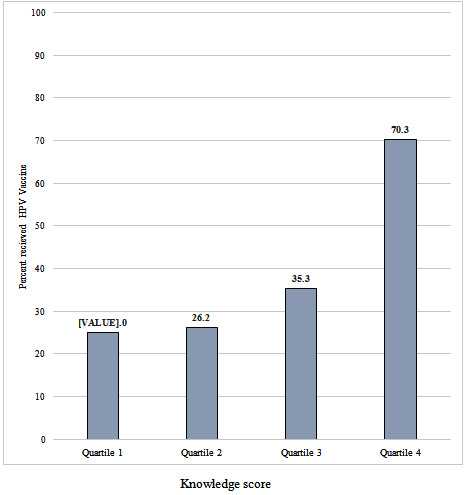
The prevalence of HPV vaccination was significantly positively associated with knowledge scores, with 70.3% of those students in the highest quartile of scores having been vaccinated as opposed to 25.0% in the lowest quartile (p=0.001) (Figure 1). The odds of receiving HPV vaccine was nearly five times as much for the students who achieved knowledge scores about the causes of cervical cancer greater than or equal to the median compared with the students with knowledge scores about the causes of cervical cancer below the median (adjusted odds ratio [aOR]:4.85, 95% confidence interval [CI]:2.15, 10.92). Particularly, students who knew that HPV is a cause of cervical cancer were almost three-times odds of receiving HPV vaccine as compared to students who did not know that HPV is cause for cervical cancer (aOR:2.90, CI:1.1, 8.2). Those who knew that cervical cancer is preventable were over 2.5-times odds of getting HPV vaccine as compared to those who did not know; however, after adjusting for other variables, the difference was not statistically significant (Table 3).
Figure 1: HPV Vaccination Status among Students based on Knowledge Score Level.
| Table 3: Odds Ratios of Receipt of HPV Vaccine for the Knowledge of Students about Cervical Cancer (n=141). |
|
Knowledge assessment item
|
Response |
Frequency |
Receipt of HPV vaccine (%) |
Odds ratio (95% CI) |
Adjusted odds ratio (95% CI)
|
|
Sexual activity is a risk for Cervical cancer
|
Yes |
95 |
46.3* |
2.1 (0.9, 4.6) |
2.1 (0.90, 5.8) |
| No |
41 |
29.3 |
— |
—
|
|
STDs & multiple sexual partners are risk factors of cervical cancer
|
Yes |
117 |
41.0 |
1.4 (0.6, 3.5) |
1.4 (0.6, 3.5) |
| No |
24 |
33.3 |
—- |
—
|
|
Human Papilloma virus causes cervical cancer
|
Yes |
103 |
47.6*** |
3.4 (1.3, 8.4) |
2.9 (1.1, 8.2) |
| No |
33 |
21.2 |
— |
—
|
|
Cervical cancer is preventable
|
Yes |
90 |
47.8** |
2.7 (1.3, 5.7) |
2.1 (0.9, 5.8) |
| No |
51 |
25.5 |
— |
—
|
|
Knowledge assessment
|
Yes |
37 |
70.3*** |
5.8 (2.6, 13.2) |
4.8 (2.2, 10.9) |
| Score ≥median |
No |
104 |
28.8 |
— |
—
|
| Note: Multiple logistic model, variable controlled for in the model are Age, Insurance, and Race/ethnicity. *p=0.05; **p=0.01; ***p=0.001 Nasar fix the decimal point for odds .00 |
DISCUSSION
Vaccination is one of the most effective and least complex ways to address the public health problems especially cervical cancer. Cervical cancer is one of most preventable types of cancer, and HPV vaccination plays a central role in this effort. Despite the safety, effectiveness, and simplicity of the vaccination program, the uptake remained quite low among the high-risk group-college students. This study showed that HPV vaccination is positively associated with students’ knowledge about cervical cancer. The association of HPV vaccination with knowledge about cervical cancer was particularly strong among students who knew that HPV infection is a causal factor for cervical cancer and cervical cancer is preventable. This finding is consistent with several other studies which showed a significant positive association between knowledge of college students about HPV and/or cervical cancer and intention to accept HPV vaccine or actual receiving of the HPV vaccine.23,24,25 Studies had also shown that members of communities at higher risk for HPV infection tend to be less knowledgeable about the transmission mechanisms of HPV and its impacted morbidities.23,26
In addition to knowledge about causes of cervical cancer, annual health checkup attendance played a significant role in HPV vaccination in the study. This finding is corroborated by previous studies conducted in Germany27 and the United States.28 Possible reasons for this finding could be because healthcare providers recommend the HPV vaccination to their patients during their visits for a medical checkup. Physicians have a greater opportunity to teach their patients one-on-one about the importance of HPV vaccination during annual check-ups, which usually last much longer than other visits. Studies consistently showed that healthcare providers’ recommendations strongly predict HPV vaccination,29,30 suggesting that recommendation and subsequent administration of the vaccine when adolescents visit healthcare providers for check-ups are crucial to increase the HPV vaccination rate.31,32 However, only 38% of the students had undergone the annual health checkup within a year before the survey was conducted. This shows that larger number of students had missed the opportunity of recommendation and/ or administration of the HPV vaccine, and this might also explain the finding of the low percentage of students who received HPV vaccine in the current study (39.7%). In fact, the percent received HPV vaccine in the current study is similar to the recent national percentage estimate (40.2%) among females aged 19- 26 years in the USA.16
However, as college students are at higher risk of HPV infection, increased HPV vaccination coverage in this age group would be more useful. Health education efforts which help increase students’ interest in attending regular health check-ups and receiving pap smearsis necessary to increase HPV vaccine coverage among college students. Additionally, physicians should be encouraged to counsel their female patients more frequently about receiving the HPV vaccine and address HPVrelated issues.
Majority of the study participants who did not receive HPV vaccine claimed lack of trust, fear of side effect, being careless as the reasons why they did not get the HPV vaccine. Consistent with our findings, other studies have also documented lack of trust, fear of adverse effects, and general apathy as common barriers to HPV vaccination in a variety of communities.33,34 The lack of trust and fear of side effect of HPV vaccination among college students could be due to the low level of knowledge of about HPV, cervical cancer, and HPV vaccination. Indeed, the median knowledge score of these students about risk factors of cervical cancer based on eight points was quite low. The literature also indicates most sexually active people-college students know little about HPV and were not practicing appropriate cervical cancer preventive behaviors.35 Hence provision of information about cervical cancer prevention emphasizing HPV vaccine is safe and effective may help to increase HPV vaccination coverage. Information campaigns about the benefits of the HPV vaccine and the risks that result from infection with HPV have shown some success in correcting misperceptions about the vaccine.36 In addition, the proportion of students who received HPV vaccine was almost three times higher among students who attended an annual checkup than those who did not attend an annual checkup. This perhaps indicates that students are more likely to receive the HPV vaccine if they have an opportunity to discuss their risk of HPV infection and the benefits of vaccination with their physician. The discussion with the physician could address many of their concerns including trust, barriers, and effectiveness of the vaccine.
Implication for Policy and Practice
The current study findings have several implications for planning public health policy and practices. The results suggest that HPV vaccination programs should include education of young women about the benefits of HPV vaccination and causes and methods of prevention of cervical cancer. The education program needs to be designed to reduce the lack of trust, fear of side effect and other concerns about HPV vaccine among college students. In effecting this, provision of information that HPV vaccine is safe and effective might be useful. This can be implemented during the annual health checkups where doctors will have the opportunity to deal details with their patients.
LIMITATIONS
The current study involved college students with highly diversified ethnic backgrounds. Thus, the present study provides information on the relationship between HPV vaccination and knowledge of individuals about HPV or cervical cancer amongstudents with the heterogeneous ethnic background. The findings of this study are based on a cross-sectional design and should be interpreted in light of several limitations. Data were from all self-reported response. Additionally, poor memory about annual medical checkups, pap smears, and vaccination might have affected the results. Moreover, the sample was not very large, which might have limited power to detect true association between vaccination and several other variables. Also, while the sample had a heterogeneous composition, it consisted mostly of students majoring in the basic sciences or health sciences. Thus, the findings might not be fully representative of college women students in general. The results should be treated as correlational not as causational.
CONCLUSIONS
Receipt of HPV vaccination was associated with knowing that HPV infection is a cause of cervical cancer and that cervical cancer is a preventable disease. HPV vaccination was also associated with annual health checkup status. Educational efforts that create awareness about the linkage of HPV infection with cervical cancer and benefits HPV vaccine would help to increase uptake of HPV vaccination rates among college students in the USA.
AUTHOR DISCLOSURE STATEMENT
The authors declare that they have no conflicts of interest exist to report.
FUNDING
The study did not receive any external funding support.