INTRODUCTION
Manipulative therapy is becoming a more and more popular type of treatment and is actively used not only in the management of spinal painful syndromes.1,2 This treatment approach can also effectively suppress the pain occurred in other parts of the musculoskeletal system.3,4 The musculoskeletal pain where manipulative therapy is really effective and more preferred than other types of pain management is usually associated with minor displacement of the articular surfaces in relation to each other, known as subluxation (partial dislocation).5
Although subluxations could potentially develop in all bone articulations, the reports about the effectiveness of manipulation in the treatment of peripheral joints mostly describe the ones affecting
large or medium-sized joints.6 There is relatively less information in the literature regarding subluxation in smaller peripheral joints of the body. The proximal tibiofibular joint (PTFJ) is one of these small articular structures. Less common attention paid to this joint subluxation, could be associated with its low frequency,7,8 or with uncommon misrecognition of this clinical pathology and therefore, with untimely assistance.9,10,11
In this article, we present a case report about a relatively rare happening of PTFJ subluxation in a child that was found to cause lower leg pain and cramps in fact for at least two-years, and in whom we were able to successfully eliminate these symptoms and their cause by manipulation on these joints.
CASE DESCRIPTION
Patient R., 5-years old, female, was brought by her mother to the doctor’s office with complaints of moderate to severe pain and cramps in her lower legs and feet. These symptoms occurred almost every night, often making her to cry and even scream because of the pain. The mother explained that these symptoms had begun two-years ago without any visible cause: no falls, visible traumas, peripheral nerve disorders, etc. Usually, these clinical manifestations developed 3-4 times a week during the nights, when after 1-2-hours of sleeping they suddenly awoke her up. The duration of attacks at the beginning was 30-40-minutes, increasing later sometimes up to 2-3-hours. During the daytime the girl was physically active, having no complaints.
The mother stated that she attempted the conservative care of changing shoes, padding, use of analgesics (Advil or Tylenol), and limitation of physical activity. However, none of these approaches helped. The girl was examined by a pediatrician who found her healthy. A podiatrist did not establish any specific diagnosis, although noticed the pronation type of both feet, with decreased arches. He suggested she might need foot surgery in the future.
In our office, a thorough examination was performed. The musculoskeletal system was also examined using the specific evaluation system, activator protocol.12 The examination revealed no neurological dysfunctions, muscle weakness, or restrictions of range of motion. Posterior subluxation of both proximal fibular heads was the only finding.
Manipulation was used as a treatment. For this, the corrections of subluxation of both proximal tibiofibular joints by applying a high-velocity, low-amplitude thrust to both fibular heads were carried out each visit.
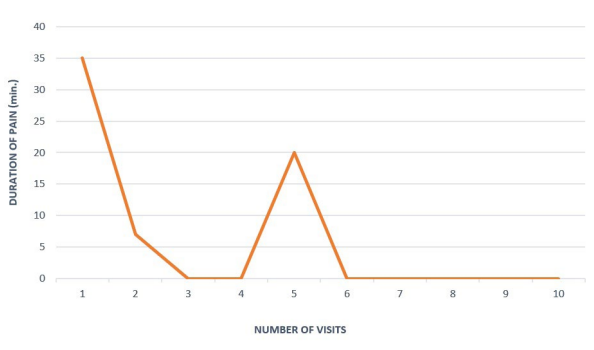
After the first visit (three-days later), the mother informed that the duration of pain and cramps attacks during the nights was reduced to 5-10-minutes instead of 30-40-minutes before the treatment. By 3rd visit (five-days later) the patient’s mother stated that these symptoms were completely absent during the night. The subluxation of the right proximal tibiofibular joint was eliminated after four visits, but on the left one only by the 9th visit (three-weeks later). During this time the pain and cramps occurred just once in the left leg, which could be associated with the longer presence of left tibiofibular joint subluxation (Figure 1). After that, the aforementioned attacks, accompanied by only mild pain, occurred in the patient just a couple of times during the next eight-years of follow-up observations.
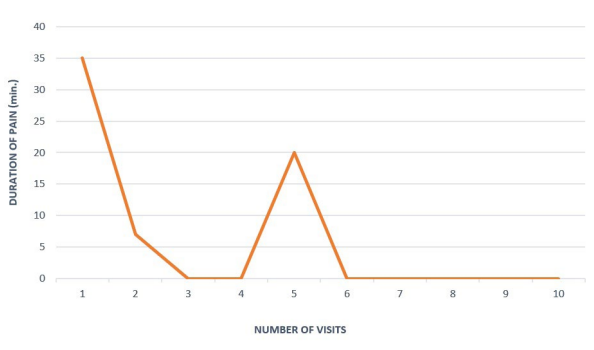
Figure 1. Duration of Night Pain in Lower Legs and Feet Before Each Visit
DISCUSSION
Thus, in the present case, the pain and cramps in the lower legs and feet seem to have been associated with the subluxation of both proximal tibiofibular joints. This was confirmed by the results of our examination and the rapid and high effectiveness of the performed manipulations.
The PTFJ is a small, plane-type synovial joint with minimal movement.9,10,13,14 This joint is quite stable articulation due to bony congruency and ligamentous and muscle support.9,11 Pathology of PTFJ is relatively rare,7,13,15 potentially it could be associated with a number of diseases such as osteoarthritis,16,17 neoplasms,18 ganglion,19 pigmented villonodular synovitis, etc.16 However, despite the relative stability of PTFJ, its damage most frequently results from injury, and is often accompanied by its dislocation,13,14,20 fibula fractures,14 rupture of ligaments around the joints and muscle tendons.21 This kind of problems occurs more frequently in young males, and usually is the result of sports activity,11,13,22 but also was described in ballet dancers, soccer players, equestrian jumpers,7 parachutists.15 The clinical experience shows also that in the case of just PTFJ subluxations without visible joint dislocation, these damages often are less recognized,14,20,23 remain undiagnosed due to difficulties with radiographic identification,14,24 lack of emphasis in the literature and textbooks,16 in polytrauma scenario,10 or in children.20,25
In the classification of the PTFJ injury in the modification of Ogden made in 1974,14 the traumatic damage of these joints is divided into four types: type I–subluxation, usually atraumatic, without visible dislocation; type II–antero-lateral dislocation; type III–postero-medial dislocation (usually as a result of direct knee trauma); IV–superior dislocation. The majority of PTFJ trauma (up to 85%) is type II injury.10,13,14 It is often associated with common peroneal nerve palsy, ligamentous injury, and bone fracture, which certainly requires surgical intervention.8
Quite frequently PTFJ trauma, as shown above, involves the common peroneal nerve with various degrees of damage.18 Depending on the nature and degree of involvement, this damage could be manifested by some sensory or minimal motor disturbances, or more serious peroneal nerve palsy8,26 whose hallmark clinical manifestation is foot drop.27 Sarma10 stated that in any knee injury accompanied by common peroneal involvement, occult PTFJ dislocation or subluxation should be clinically suspected and ruled out.
The case presented demonstrates the pathology of both proximal tibiofibular joints. Neither the child nor the mother could recall any visible trauma, and the examination found no neurological dysfunctions, muscle weakness, or restrictions of range of motion. Only the use of the special evaluation system, however, made it possible to identify postero-medial subluxation of both PTFJ. Based on Ogden’s classification,14 this pathology corresponds to Type I of PTFJ injury and fits the definition of this joint subluxation as “excessive, symptomatic motion without frank dislocation”,28 or as symptomatic hypermobility of the PTFJ.20
Evidence of the relationship between the symptoms and subluxation, as mentioned above, is suggested by the rapid and high effectiveness of the treatment. The restoration of the congruency of both joints in our patient just through the mechanical correction (posterior-to-anterior push of the proximal fibular heads) made it possible to eliminate the night pain and cramps in both lower legs and feet in fact permanently within a very short time of only two-visits. This is essential because the complete stabilization of PTFJ subluxations usually requires a longer time.13,29
It is interesting to analyze the nature of pain and cramps in the present case. Potentially, any subluxation could result in pain due to the involvement of the enthesis.30,31 In this situation, the pain would have been localized just in or around the involved PTFJ. However, the patient complained of pain in the areas which are at a certain distance from the involved joints. We assumed that the common peroneal nerve can be involved in the pathological process because a part of it is located exactly behind the proximal fibular head.
The common peroneal (common fibular) nerve is a branch of the sciatic nerve. It is well-known that the nerve passes over the posterior aspects of the proximal fibular head, where it is susceptible to injury.10,25,32 Just inferior and lateral to the fibular head at the fibular neck, it divides into two nerves – the superficial and deep fibular nerves.16,33 In addition to innervating the muscles that compose the anterior and lateral muscular compartments of the lower extremity, the common peroneal nerve carries afferent cutaneous sensory fibers. They are responsible for sensation in the anterolateral aspect of the lower extremity that extends from midway down the leg to the majority of the dorsal aspect of the foot and toes.33
The distribution of pain in our patient exactly corresponds to the areas innervated by the sensory fibers of this nerve. We assume also that with a high degree of probability the cramps can be caused by the irritation of the motor fibers of the common peroneal nerve. The causative factors of the nerve involvement, in this case, are posteriorly subluxated proximal fibular heads which can compress or stretch the common peroneal nerve before it divides into superficial and deep fibular branches. This irritation of both sensory and motor fibers, in our opinion, can be the plausible explanation for why the child experienced night attacks of both pain and cramps in the legs in this case. Although during the day examination no objective neurological signs were revealed, the disappearance of these symptoms after elimination of the subluxation represents the good evidence and confirmation of our assumption about common peroneal nerve involvement.
Therefore, this compression could compromise both sensory and motor functions of the nerve. We found the possible confirmation of our concept in the article of Hardin and Devendra.33 These authors noted that incorrect or too tight placement of a splint or cast under the knees, across the fibular head after a trauma or burn, can result in compression of the common peroneal nerve. We believe that one of the likely mechanisms of the nerve compression in these cases could be the posterior proximal fibular head subluxation caused by this tightness.
In our present case, the treatment of both PTFJ subluxations turned out to be correct and highly effective. Lower leg pain and cramps ceased to bother the child already after the second visit, which occurred quite soon after the beginning of the care. The previous treatment (use of analgesics, changing shoes, padding) was ineffective.
In general, the treatment of PTFJ injury depends on many factors. In the case of tibiofibular instability, some clinicians recommend surgical treatment, even if the injury is not associated with trauma.25 Other specialists, however, prefer to use the surgery only when the conservative treatment is ineffective,14,23 or only when chronic problems or neurological symptoms exist, and surgery is generally considered a last resort.30 After analyzing 44 publications, Kruckeberg34 found that such surgical approaches as fixation and fibular head resection are not safe and are associated with high complication rates.
Based on the data of other clinicians, the character and duration of the treatment should depend on the type of PTFJ injury and its severity.15,23 In the case of PTFJ subluxation (taking into account Ogden’s classification) the conservative treatment is usually the first choice,35 but with varying degrees of efficiency and therapy duration: immobilization,14 anti-inflammatory drugs,15 physical therapy,29 wearing a supportive strap around the involve PTFJ,20 mobilization,15,36 manipulation.21,24,37 Although subluxation of this joint is less recognized than its dislocation,20,23 the use of manipulation in this type of injury can be quite successful.21,37 For example, De Franca38 reported immediate and dramatic relief of knee and thigh pain after the manipulation of the PTFJ. Beazell37 used the PTFJ manipulation in a young runner with three months of knee pain, and this patient was able to resume running without pain in just one week after the initial intervention. Taking into consideration the
objective finding (posterior subluxation), we have chosen the most logical and easiest treatment approach which resulted in the alignment of the PTFJarticular surfaces. It was the manipulation. And this approach has led to a rapid and stable clinical effect.
CONCLUSION
1. Lower leg pain and cramps could be associated with PTFJ subluxation.
2. In the case of posterior PTFJ subluxation, the subluxated proximal fibular heads can compress and/or stretch the common peroneal nerve.
3. The common peroneal nerve involvement can be the most likely causative factor of lower leg pain and cramps in the case of PTFJ subluxation.
4. The high-velocity low-amplitude thrust manipulation could be the primary and optimal treatment in the case of PTFJ injury if its damage is limited just by subluxations of these joints.
ACKNOWLEDGEMENT
We would like to thank Professor Brent Russell from Life University for his help and recommendations in the process of preparation of this article.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.