INTRODUCTION
Sarcoma in general is very rare tumour contributing with only 0.7% of all malignant tumours while angiosarcoma is even rarer contributing with only 1% all sarcomas. The presence of an angiosarcoma in the lung is usually a consequence of metastasis from another primary site but in very few cases it has been described with a primary origin in the lung.
CASE REPORT
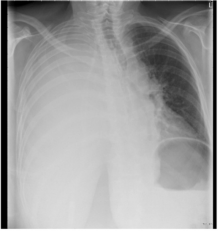
A previously healthy 57-year-old woman was admitted to the Emergency Department with shortness of breath and in general poor conditions. The oxygen saturation was 91%, blood pressure 113/68 mmHg, and heart rate 119 beats per minute. Blood samples revealed hemoglobin (Hb) at 4.2 mmol/l (reference 7.0-10.0), white blood cell count 24.3 x 109 /l (3.0-10.0) and C-reactive protein 128 mg/l (<10). A chest X-ray at the primary survey demonstrated pleural effusion on the right side (Figure 1). A 24 Charrière chest tube was inserted, with immediate drainage of about 1200 ml coagulated blood. Anemia and the general poor clinical condition demanded blood transfusions. The patient had continuously blood loss (over 3000 ml) and decreasing hemoglobin (Hb 3.4 mmol/l) during the next 24 hours leading to a thoracotomy. ><10). A chest X-ray at the primary survey demonstrated pleural effusion on the right side (Figure 1).
Figure 1: Chest X-ray demonstrates pleural effusion.
A 24 Charrière chest tube was inserted, with immediate drainage of about 1200 ml coagulated blood. Anemia and the general poor clinical condition demanded blood transfusions. The patient had continuously blood loss (over 3000 ml) and decreasing hemoglobin (Hb 3.4 mmol/l) during the next 24 hours leading to a thoracotomy.
Intraoperative findings were multiple lesions in the lung parenchyma and diffuse bleeding from multiple small abnormal nodules on the surface of the lung and chest wall. Despite transfusion with blood products (thrombocytes, red blood cells) during the next days, there was still ongoing bleeding and on seventh postoperative day, the patient underwent re-thoracotomy in order to achieve hemostasis. Intraoperative findings were less diffuse bleeding from lung and chest wall than at the primary operation and the hemostasis was achieved.
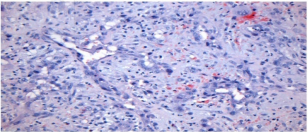
Biopsies from multiple sites from the lung and chest wall were sent for histological investigation. Microscopically the material was made of disorganized fibromyxoid tissue with massive bleeding and some necrosis. In areas of preserved tissue there were irregular vascular or cystic structures or solid angulated groups of malignant cells. The tumour cells were large with plump or polygonal nuclei with vesicular chromatin pattern and prominent nucleoli (Figure 2).
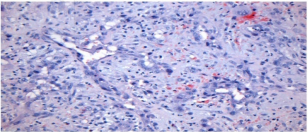
Figure 2: The figure demonstrates irregular vascular structures and diffuse infiltrating cells with variation in size and atypical nuclei (Hematoxylin-eosin x200).
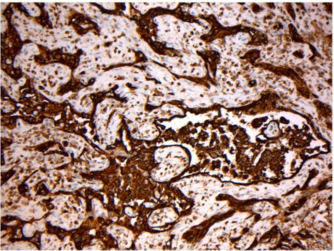
In a broad panel of immunohistochemical markers the tumour cells were negative for epithelial, mesothelial and melanocytic antibodies. There was positive staining for vimentin, CD31 (Figure 3).
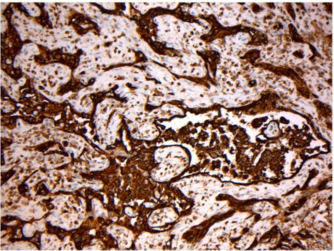
Figure 3: The figure demonstrates intraluminal proliferation and solid groups of cells with positive staining for CD31 (x100)
Von Willenbrand Factor VIII, and partly for podoplanin (D2-40) and WT1, but was negative. The pattern was high lightened by staining for collagen IV.
The vascular pattern with intraluminal proliferations of malignant cells together with immunohistochemical positivity for endothelial markers made the diagnosis of angiosarcoma and with the primary tumour burden in the lung parenchyma, primary pulmonary angiosarcoma.
DISCUSSION
In this rare case the patient presented with a hemothorax, which is most often caused either by chest trauma, iatrogenic event or intrathoracic carcinoma. Hemothorax should be suspected in hypovolemic patients with chest X-ray demonstrating pleural effusion. Blood loss in pleural cavity may be massive and even minor injury can lead to significant blood loss.
Only 0.7% of all malignant tumours are sarcomas. Angiosarcoma (AS) is a malignant tumour of vascular endothelial origin contributing with only one percent of all sarcomas.1,2,3,4,5 The presence of AS in the lung is usually a consequence of metastasis from another primary site.1,2,3,4,5,6,7,8 The most common primary sites for AS are the skin (60%), soft tissue (25%) and in the visceral organs predominantly the heart, liver and spleen. In English spoken literature there have only been reported a few cases describing primary pulmonary angiosarcoma.2
AS in the lung can be uninodular involving one vessel or airway or multifocal with ill-defined, soft, red nodules in the lungs and pleura3,7,9,10 as it was demonstrated perioperative in this case. Primary pulmonary angiosarcoma is characterized by insidious growth, where the tumour usually demonstrates extensive local invasion and haematogenous metastases by the time of presentation2,4,8 therefore curative intended treatment is not an option and the treatment of choice is palliative therapy.
The prognosis for angiosarcoma is in general poor and the survival rate range from 1-9 months after initial diagnosis.1,2,3,9,10,11 Only patients with surgically resectable primary sarcomas of the extremities, breast, head and neck have long-term survivals while patients presenting with primary sarcomas in respectively thorax and abdomen or recurrent AS and metastatic AS have poor survival.8
Different therapeutic modalities have been attempted, but none of them have shown to change the course of the disease.1,5,11,12
The few reported primary pulmonary AS all presented with bleeding either as intractable haemoptysis, massive intra-parenchymal bleeding or intrapleural haemorrhage.3 The symptoms are unspecific but described as chest pain, haemoptysis, dyspnoea, cough, and malaise.5,7,9,10,12 At the primary operation the priority was to achieve haemostasis that went successful but after seven days we had to do re-thoracotomy in order to achieve haemostasis again. The disease was too widespread in the lung and at the chest wall at that time accordingly curative radical surgery was not an option. Her poor general condition did that she died one day after discharge from the hospital.
CONCLUSION
Primary pulmonary angiosarcoma has a poor prognosis in itself but can also cause serious and life-threating intractable intrathoracic bleeding.