INTRODUCTION
Globally and in the United States, public health officials continue to monitor the prevalence of coronavirus disease-2019 (COVID-19) cases along with incidence, mortality, and the population vaccinated.1,2 The U.S. Department of Veterans Affairs (VA) also publishes similar COVID-19 data from the population that utilized VA medical facilities.3 Elected leaders, public health professionals, and clinicians remain concerned about the number of new COVID-19 cases and individuals who have received COVID-19 vaccinations. The COVID-19 delta variant and its possible impact on the population is a concern to elected leaders, public health officials, and clinicians.4 This variant is one of four “variants of concern” for public health and medical professionals (Table 1). Throughout the COVID-19 pandemic, genetic variants of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have been circulating around the world.
| Table 1. Classification-SARS-CoV-2 Variants of Concern, as of June 29, 2021 |
| Pango Line-age |
WHO Label |
First Identified |
Attributes |
| B.1.1.7 |
Alpha |
United Kingdom |
• ~50% increased transmission
• Potential increased severity based on hospitalizations and case fatality rates
• No impact on susceptibility to EUA monoclonal antibody treatments
• Minimal impact on neutralization by convalescent and post-vaccination sera |
| B.1.351 |
Beta |
South Africa |
• ~50% increased transmission
• Significantly reduced susceptibility to the combination of bamlanivimab and etesevimab monoclonal antibody treatment, but other EUA monoclonal antibody treatments are available
• Reduced neutralization by convalescent and post-vaccination sera |
| B.1.617.2 |
Delta |
India |
• Increased transmissibility
• Potential reduction in neutralization by some EUA monoclonal antibody treatments
• Potential reduction in neutralization by post-vaccination sera |
| P.1 |
Gamma |
Japan/Brazil |
• Significantly reduced susceptibility to the combination of bamlanivimab and etesevimab monoclonal antibody treatment, but other EUA monoclonal antibody treatments are available
• Reduced neutralization by convalescent and post-vaccination sera |
| Source: Centers for Disease Control and Prevention (CDC)4 |
The history of public health is marked by several areas of success. Vaccine-preventable diseases are of public health significance.5 For example, vaccines, like immunizations, are important public health interventions. The history of public health in the United States is filled with many successes. In the 20th century, the greatest public health achievements in the United States included the following6,7:
• Vaccination
• Motor-vehicle safety
• Safer workplaces
• Control of infectious diseases
• Decline in deaths due to coronary heart disease and stroke
• Safer and healthier foods
• Healthier mothers and babies
• Family planning
• Fluoridation of drinking water
• Recognition to tobacco use as a health hazard
The response to the COVID-19 epidemic included biomedical and vaccine research, identification of COVID-19 cases, contact tracing, community health promotion and disease prevention, and community vaccination. COVID-19 vaccinations remind public health professionals and non-professionals alike of this essential public health intervention for controlling infectious diseases. Actions that seek to improve existing vaccination efforts are equally important for effective public health programming and should be driven by evidence and considerations of professional practice. As we consider sustained public health action to protect populations from COVID-19 in the foreseeable future, it might be useful to explore the relationship between the number of COVID-19 cases and vaccination at a systems-level and discuss our point of view on the possible implications of the data for public health programming.
METHODS
This project explored the association between the aggregate number of COVID-19 cases identified within a healthcare system and the aggregate number of COVID-19 vaccinations administered within the same system as well as the implications of the findings for public health action. Secondary data analysis techniques were combined with an ecological study design to examine any possible associations between the number of COVID-19 cases identified at medical facilities (facility names not identified) within the VA healthcare system and the number of COVID-19 vaccinations administered within the system. The public data (n=141 medical facilities) were accessed using the VA ‘Open Data’ portal: VA COVID-19 National Summary (updated: June 16, 2021). The data presented aggregated counts on the number of COVID-19 veteran patients who had been tested or vaccinated at VA facilities throughout the United States and Puerto Rico. The data fields found in the dataset used in this project included each facility name along with counts for VA Total Confirmed COVID Cases, Convalescent Cases, Dose 1 of 2 for Pfizer or Moderna Vaccine, Dose 2 of 2 for Pfizer or Moderna Vaccine, and Dose 1 of 1 for Janssen Vaccine. An assumption made in reviewing the data was that the type of vaccination recorded is mutually exclusive: That is, data were recorded in situations where individuals who received the two-dose vaccine could also not receive the single-dose vaccine, and vice-versa, during the period of COVID vaccination administration. The number of Convalescent Cases and other aggregate data fields were not used.
Statistical scatter plots were constructed using NCSS 11 Statistical Software.8 A loess curve was plotted to help to identify if a curvature pattern was present. The loess method (or the locally weighted regression scatter plot smoothing method) was used to obtain a smooth curve representing the relationship between the values (x, y). Unlike linear regression, the loess method does not have a simple mathematical model. It is an algorithm that, given a value of x, computes an appropriate value of y. The algorithm was designed so that the loess curve travels through the middle of the data, summarizing the relationship between x and y.8,9 An increasing pattern (indicated by an increasing curvature pattern of the loess curve) in the number of confirmed COVID cases to the number of COVID vaccination might have public health implications.
RESULTS
In each plot (Plot 1, 2 and 3), the number of vaccinations administered for each type of vaccine by the number of confirmed COVID-19 cases at each of the 141 medical centers is graphed (x, y). The two-dose Pfizer and Moderna COVID-19 vaccines along with the Janssen single-dose vaccines are reported. A loess curve was included with each plot. It is very unlikely that during the current COVID-19 pandemic that individuals in the population received both types of vaccines.
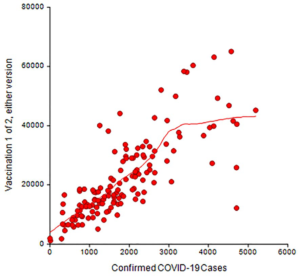
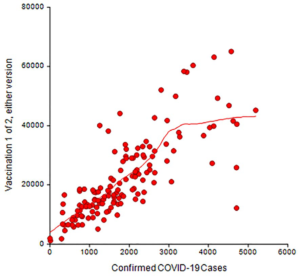
Plot 1. Number of confirmed COVID-19 cases among veterans using VA medical facilities and number of COVID-19 vaccinations administered (i.e., Pfizer and Moderna) 1 of 2 at the same VA medical facilities, updated June 16, 2021
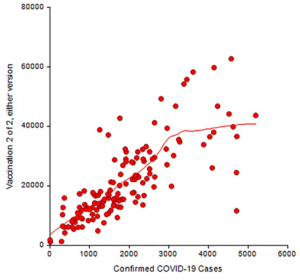
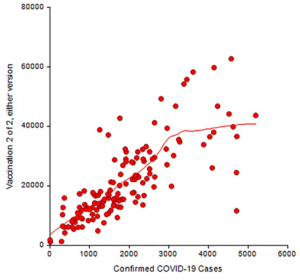
Plot 2. Number of confirmed COVID-19 cases among veterans using VA medical facilities and number of COVID-19 vaccinations administered (i.e., Pfizer and Moderna) 2 of 2 at the same VA medical facilities, updated June 16, 2021
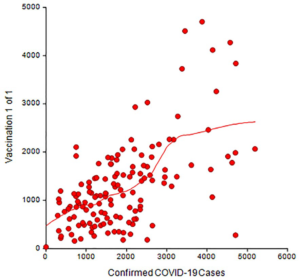
Plot 3. Number of confirmed COVID-19 cases among veterans using VA medical facilities and number of COVID-19 vaccinations administered (i.e., Janssen) at the same VA medical facilities, updated June 16, 2021
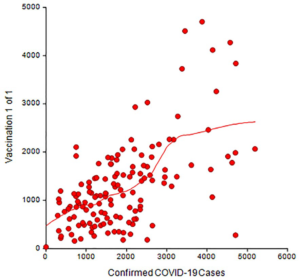
The red symbols in each plot represent the number of vaccinations administered and the number of confirmed cases of COVID-19 at each medical facility. The statistical algorithm for the loess curve identified an increasing curvature pattern. All plots showed that the red symbols became more separated in moving from left to right.
DISCUSSION
We found that within this healthcare system, the loess curve showed a gentle, upward association between the number of confirmed cases of COVID-19 at medical facilities and the increasing number of COVID-19 vaccinations (Plot 1, 2, and 3). Many facilities performed near the loess curve while others did not. For example, consider facilities with approximately 1,000 confirmed COVID-19 cases and the curve in Plot 1: Some facilities reported a high number of vaccinations for the number of confirmed COVID-19 cases compared to other facilities. For some reason, facilities in the lower right portion of each plot did not report vaccination administration at a level near or above the loess curve although the number of confirmed cases was high. By contrast, this was not the case in the upper right portion of each plot.
Refinement 1
Explore the reasons for differences between facilities: It might be useful to further explore the efforts at the facilities that are well above and well-below the loess curve to understand the differences. These differences might yield a collection of “best practices” in community vaccination to share among medical facilities. For example, the differences found in the prior plots could be related to a number of characteristics pertaining to individuals who chose to receive a COVID-19 vaccination, including the decision to receive it, perhaps, outside of the healthcare system and that information not being part of the data collection and reporting efforts of the system.
Refinement 2
Provide vaccination outside traditional settings: The COVID-19 pandemic has been addressed by a combination of biomedical re search related to vaccine development, clinical treatment, vaccine administration and public health interventions in developed countries. In middle income and developing countries, the pandemic has been addressed by clinical treatment, vaccine administration (where available), and public health measures. Efforts to identify cases of COVID-19 along with community vaccination activities could illustrate the importance of making available prevention services outside of the traditional clinical setting in order to achieve better community-wide, public health prevention outcomes.10
Refinement 3
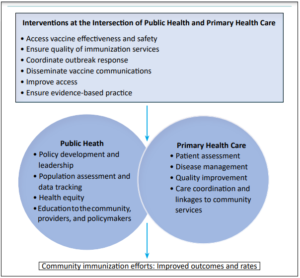
Public health and primary care partnerships for community vaccination: The Association of State and Territorial Health Officers (ASTHO) has posited that public health and primary care partnerships in the U.S. and, perhaps, other countries, might be useful in advancing immunization efforts for the population. ASTHO considered the partnership using a graphical representation (Figure 1)10:
Figure 1. ASTHO Public Health and Primary Care Partnership: Immunization (from policy brief)
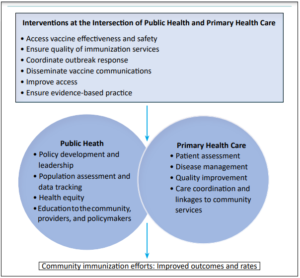
It might be that some of the ideas from ASTHO regarding immunization at the community-level could be applied to future COVID-19 vaccination efforts. It is important to note that public health work could not be accomplished without health administrators and health managers.11 Furthermore, community engagement and collaboration are commonly used techniques of public health practice. Public health administrators and managers might consider using these techniques with the community and among primary health care professionals in efforts designed to produce increased COVID-19 vaccination rates in the population.
Refinement 4
Addressing vaccine knowledge-gaps in the community and other barriers to vaccination: While vaccinations are effective for preventing vaccine-preventable diseases in a population, some members in a population refuse to receive vaccination.12 The control of communicable diseases relies on the application of public health sciences, and study of how members of a population understand a communicable disease and disease prevention efforts in a cultural context. Small-area questionnaires might be useful for examining how populations understand a communicable disease and related prevention activities.13 The topics of vaccine misinformation and refusal may have a cultural dimension and was found in a systematic review exploring disparities in H1N1 vaccination rates and synthesis of insights to inform COVID-19 vaccination efforts. Some recommendations for improved COVID-19 vaccination equity resulting from the systematic review included14:
• Vaccines should be offered at no-cost.
• Target vaccination outreach to communities with large ethnic populations or lower-income populations, especially in areas with fewer healthcare resources.
• Make use of non-traditional settings for vaccine administration.
• Provide vaccination in or near workplaces.
• Engage with trusted, community messengers.
• Address issues of vaccine safety.
These recommendations might be applicable to various populations around the globe.
CONCLUSION
This aggregate pattern in number of COVID-19 cases and number of vaccinations administered might be present in other public health settings or healthcare systems. Four refinements were proposed. A discussion of vaccination “best practices” is always useful for public health decision-makers, health system managers, and clinicians. In some public health settings or healthcare systems, there might be a role for a group practice manager to facilitate the adoption of some vaccination best practices, along with collaboration of effort, to effectively administer vaccinations to a population outside traditional settings. This might lead to public health and primary health care collaboration on issues of vaccination and other related prevention services.
Conducting small-area questionnaire among the unvaccinated population in selected, geographic areas might produce useful results. A better understanding of vaccination refusal might permit local public health leaders and the community to address issues in the local population that could facilitate vaccination acceptance. Collectively, vaccination “best practices” and findings from small-area questionnaires, and the involvement of various agents in collaborative efforts might help public health decision-makers and health system managers to better understand the system-level resource needs and issues of vaccine acceptance. Refinements could lead to higher COVID-19 vaccination rates in a public health setting or within a healthcare system.
ACKNOWLEDGEMENTS
None.
DISCLOSURES
No financial investments—stock, stock options—connected with this work. Public/Open Data available from the US Department of Veterans Affairs “Open Data” Portal.
DISCLAIMER
The views in this paper are those of the authors and do not represent any official position of the US Government.
SOURCE OF FUNDING
None.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.