INTRODUCTION
Cervical spine fractures are rare in children as compared with adults with a reported rate of incidence of 1.5 to 3% of all traumatic lesions of the spine.1,2,3,4,5,6,7 The estimated annual incidence of pediatric cervical spine injuries is about 7 per 100,000 patients and around 1 per 100,000 patients for children less than 11 years of age.1,2,3,4,5,6,7 When analyzing cervical spine injuries, the upper cervical vertebrae are more susceptible to trauma as compared to the subaxial levels. This is more than likely due to the fact that the head of the upper vertebrae are proportionately larger. Furthermore, the odontoid process of the axis remains the most vulnerable part of the upper cervical spine when compared with spinal injuries in small children.8,9,10,11,12,13,14,15,16,17,18,19,20,21 This occurrence is attributed to the anatomical characteristic that the odontoid and the axis are separated by an apophyseal plate. Since this cartilaginous plate does not ossify until a child is 7-years-old, this developing region of the spine remains an area of potential weakness in preschool children.5,8,9,10,13,14,15,16,17,22,23 Although, rare in the overall incidence of spinal trauma, odontoid synchondrosis fractures are some of the more common fractures that occur in young children.1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21
The treatment of acute odontoid synchondrosis fractures in children depends on the amount of broken dense present, its forward displacement, and the angulation at which the injury is inflicted. In a majority of cases, displacement and angulation of the broken part of the odontoid varies from mild to moderate, and most authors advocate for a closed reduction and an external stabilization with either a Minerva jacket or a Halo-vest. These undertakings are then monitored very closely during a radiographic follow-up.1,11,12,13,22,23
Despite the fact that there is a 43% complication rate and up to 10% of the failure of fusion was reported, Halo orthosis has been observed to be the most beneficial approach in the two limited clinical series.12,18 New modifications in the Halo crown and pins’ design, as well as its applied torque, have recently demonstrated a dramatic reduction in the complications attributed to this procedure. The changes have yielded a successful set of data supporting Halo-vesting to be the most commonly used orthoses for treating unstable pathologies of the cervical spine in small children.11,13,15 This is supported by evidences confirming the low incidence of complications and high fusion rates reported in the more recent medical publications. Modifications to the Halo crowns and pins in children as well as proper pin site wound care might be the key components to be addressed to ensure optimal results and negligible complications.21,22,23,24,25,26
In certain situations, the posterior C1-C2 fixation may be warranted for individual cases with a complete translation of the broken dense. Fixation of C1-C2 may likewise be necessary, if there is a marked angulation that adequately shows the disruption of the corresponding posterior ligamentous structures.27,28,29 Another indication for the need of surgical intervention is the non-union of separated structures despite the long-term application of an external fixation.26 Herein, the case report of 3 children including one toddler and 2 preschoolers have been presented. Each patient possesses an acute odontoid synchondrosis fracture in which perfect bony fusion at the site of the synchondrosis plate was observed with the application of Halo-vesting. Immobilization with orthosis continued for a duration of 8 to 10 weeks without the occurrence of any Halo-related complications. This empirical data may well indicate the need and the overall safety of this important device in very young patients.
CASES
Three children including two girls and one boy were referred to our institute within a few days to a week after sustaining neck traumas. The girls were 2.5 and 4-years-old respectively and the boy was 4.5-years-old. The youngest girl was injured after a fall from the stairs. The older girl sustained a fracture after being hit by a heavy book falling on her head while she was playing below a bookshelf. The young boy sustained a neck injury in a car accident while he was sitting unrestrained in the back seat of the vehicle. All children were admitted shortly after the injury to the nearest local hospital. From there, each of the patients was referred to our institute within 4 to 7 days.
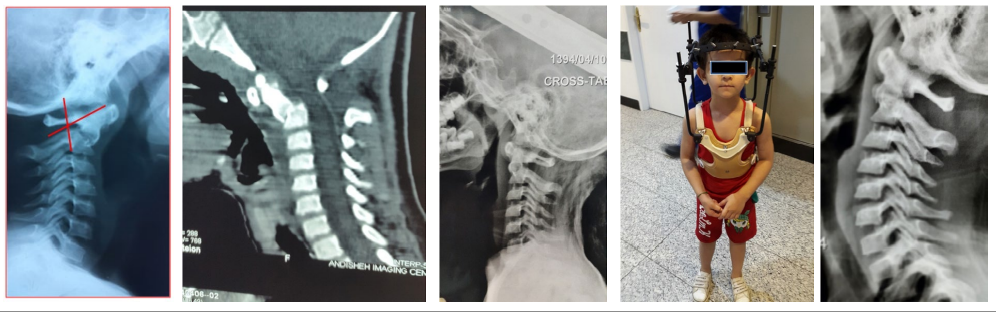
Odontoid synchondrosis fractures were detected in the plain radiographs in each of the three children. Each case was then reconfirmed in the computerized tomography (CT) scans that followed. The flexion deformity could be corrected with neck hyperextension in two of the cases and with cranial skull traction in the third. After an approximation of the fractured dense and body of the axis, the neck of each patient was immobilized with Halo orthosis in all the three cases. This was continued for 12 weeks in the preschool children and 8 weeks in the toddler. Solid bony fusion was observed in all the three patients. The information about these three cases is clearly demonstrated in Table 1. The radiographs and CT scans for these cases and the corresponding therapeutic legends of these 3 patients are illustrated separately (Figures 1, 2 and 3).
Figure 1: a) Lateral Cervical Radiograph of a 4-Year-Old Girl Showing Odontoid Fracture with Anterior Displacement,. Note: 60 Degree Fracture Angle, Compatible with Type. b) Odontoid Synchondrosis Fracture. b) Reconstructed CT San Confirms the Pathology. c) Reduction of the Fracture with Halo Traction. (d) The Child in Halo-Vest, (e) after 12 Weeks, Good Ossification Observed at the Site of Fracture.
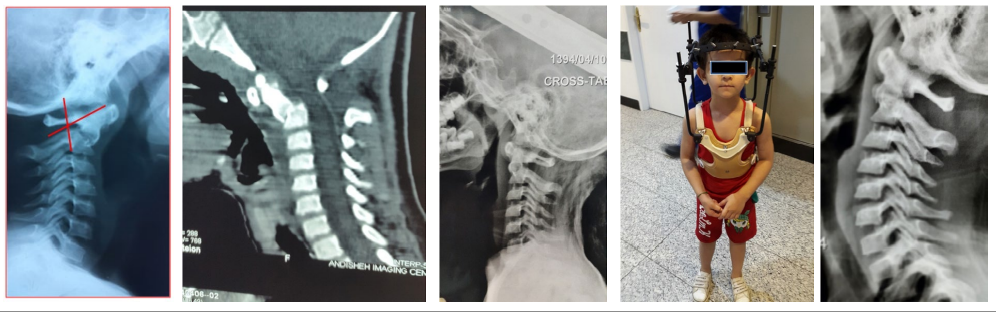
Figure 2: a) Lateral Cervical Radiograph in a 2.5-Year-Old Girl, with Odontoid Synchondrosis Fracture with Minimal Angulation and Displacement. b) Reconstructed CT Scan of the Same Child. (2c) Lateral Cervical X-Ray in Halo-Vest. 2d) The Child in Halo-Vest. 2e) Cervical Radiograph after 8 Weeks of Treatment Showing Good Fusion.

Figure 3: a) Lateral Cervical X-Ray of a 4-Year-Old Boy Showing Odontoid Synchondrosis Fracture, the Fracture Angle being 30 Degree. b) Reformatted CT Scan Showing the Same Pathology. c) The Child in Halo-Vest. d) The Only Available X-Ray Taken 4 Months Later.

| Table 1: Indicates the Gender, Age, Etiology, Reduction Technique and the Treatment of Three Clinically Reported Cases. |
|
No
|
Sex |
Age |
Cause |
Reduction technique |
Treatment strategy |
| 1 |
Girl |
2.5 years |
Fall from the stairs |
Neck hyperextension |
Halo-vest 8 weeks
|
|
2
|
Girl |
4 years |
Hit by heavy object |
Skull traction |
Halo-vest 12 weeks |
| 3 |
Boy |
4.5 years |
Car accident |
Neck hyperextension |
Halo-vest 12 Weeks
|
DISCUSSION
Spinal injuries in small children are rare with a reported incidence of 0.2 to 0.5% of all skeletal fractures or dislocations. Among the spinal injuries, those occurring in the cervical spine are infrequent and are fundamentally different from their adult counterparts.1,2,3,4,5,6,7 The reason for this difference is the greater flexibility and resilience of the pediatric column. Such resilience allows the force of injury to be dissipated more easily over a greater number of spinal segments.1,2,3,4,5,6,7,23 More specifically, cervical spine injuries in children have an estimated annual incidence of about 7 per 100,000 patients and around 1 per 100,000 patients for children less than 11 years of age.1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23
The upper cervical spine is more susceptible to trauma in the small and preschool children. It has been shown that the younger the child is at the time of injury, the more likely the injury is to occur in the region of the upper cervical spine.8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23 This specific region has several characteristics that predispose it to such injuries including: increased ligamentous laxity, more horizontally oriented facet joints, less mature bone ossification, weak neck muscles, higher fulcrum of the cervical spine, and most importantly, the child’s greater head-to-body ratio. It is because of this greater ratio that more forces are directed towards the junction between the larger head and the smaller body.8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23
Among the upper cervical injuries, the odontoid remains the most vulnerable part in small children. Within this age group, the odontoid process and the axis are separated by a cartilaginous plate which does not ossify until the age of 7 years. Therefore, the shear forces bypass this plate resulting in an odontoid synchondrosis fracture.8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29 The average age at which children sustain odontoid synchondrosis fractures was recorded as 4 years irrespective of sex.
Etiology
In children who are less than 11-years-old, motor vehicle accidents account for 38% of all odontoid injuries. Previous biomechanical investigations using simulations have shown vehicle speeds greater than 40 km/h to be sufficient to create shearing forces capable of causing such injuries in children below the age of 7 years.
Pathogenesis
The pathogenesis of these types of fractures is usually the sudden flexion of the neck with regards to a child’s large head size. These conditions will then result in an injury at the weakest part of the upper end of the cervical spine; the odontoid synchondrosis plate. As a result of such a flexion injury, the fractured dense tends to be displaced anteriorly marked by the presence of a resultant variable angulation.8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23 Extension injuries of the plate will occur rarely, being manifested only with the posterior displacement of the dense.
Clinical Picture
The clinical reflection of children with odontoid synchondrosis fractures will depend on the amount of displacement or angulation of the dense and the associated ligamentous disruptions that are present. These separate phenomena together reveals the intensity of the causative trauma. Therefore, the corresponding clinical picture can be variable and is best described by a spectrum. On one side of the spectrum are cases with elaborate spinal cord injuries and even casualties due to severe atlantoaxial dislocations.17,19,27 The cervical spine injuries with less severity may cause myelopathies with variable features ranging from mild hand numbness and changes involving the fine movements of the fingers and unsteady gait, to a more severe and crippling spastic quadriparesis.17,23,29 On the other side of the spectrum, there may be mild to moderate displacement or angulation of the dense for which the affected child might remain asymptomatic.20,23 In the middle of the spectrum, are the children experiencing neck pain, flexion deformity and limited neck mobility or torticollis.17
According to Fassett et al16 about two thirds of the patients remain asymptomatic or report only neck pain. In these patients, the correct diagnosis raises a high index of suspicion. Delays in diagnosis may cause the surgeon to enter the most problematic situations involving these types of injuries or to discover chronically neglected cases.
Imaging
Prompt radiologic evaluation of children with neck pain or stiffness following an accident causes a forced hyper-flexion of the neck, which is absolutely necessary to determine the possibility of an odontoid synchondrosis fracture.8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23 As was described earlier, shear stress at the synchondrosis between the body and the odontoid in hyperflexion, leads to an anterior angulation in 94% cases and a forward dislocation of the odontoid in more than 90% of such cases. When this type of injury is suspected, a proper assessment can be achieved through the use of lateral cervical radiographs. The resultant severity of an odontoid synchondrosis fracture can be determined by the measurement of the fractured dense angulation or its forward displacement.18,19,20,21,22,23 The fracture angle is defined as the angle between the perpendicular line of the base of the vertebral body of axis and the tangent to the posterior surface of the odontoid process. The degree of displacement is then measured as the percentage of forward displacement of the broken dense with respect to the upper surface of the axis.18,19,20,21,22,23
It should be noted that in children it may be difficult to distinguish a non-displaced acute synchondrosis fracture from a normal apophyseal plate. In case of any existing confusions, flexion/extension views may be helpful. However, CT and in particular, reconstructed sagittal and coronal images may allow the physician to arrive at the correct diagnosis.30 An increased C1-C2 interspinous distance that is demonstrated through lateral cervical spine radiographs and within a sagittal reformatted CT scan is indicative of a complete or partial disruption of the posterior ligamentous injury.23 Such findings are typically seen in type III odontoid synchondrosis fractures. This specific subtype is considered to be the clinically most severe subtype. In case of such reported findings, an magnetic resonance imaging (MRI) is very helpful in detecting the ligamentous structures as well as the degree of canal compromise and myelopathy associated with the AA dislocation. The posterior ligamentous disruption in T2 weighted images may present as a hyper-intense area existing between the C1 and C2 spinal processes. Being able to view an associated demonstration of myelopathy at the cervicomedullary junction, is also an advantage of using MRI.
Despite the clinical picture and imaging features of this pathology, diagnosis of odontoid synchondrosis fracture might be missed or arrived at following a significant delay. This suggests that to ensure the correct diagnosis of odontoid synchondrosis fracture, a high-level of suspicion has to arise necessarily.15,23,31 A delayed diagnosis and consultation are not uncommon in instances of apophysial odontoid fractures.15,23,31 In well-developed countries, about 90% of the cases with odontoid fracture are diagnosed without a delay and only 10% of the cases are neglected. However, in the developing world, missed cases are seen more often. Eventually, late diagnosis is inevitably associated with an increased risk of developing neurological deficits due to atlantoaxial dislocation.
Treatment
The treatment of odontoid synchondrosis fracture is quite different in acute and chronic cases. In this paper, we will not discuss about the treatment of chronic conditions in which the diagnosis is usually undertaken after a significant delay. This paper aims to address the approaches towards treating acute post-traumatic cases where imaging and time are utilized for best possible outcomes.
Odontoid fractures in children and adolescents have been classified into 2 types. Type I refers to odontoid fractures in young children occurring before the closure of the basilar synchondrosis plate. Type II, or odontoid fractures in older children, refers to fractures occurring after the complete ossification of the corresponding synchondrosis plate. Whereas the clinical picture and management in the latter group is quite similar to adult odontoid fractures, odontoid fractures in small children are managed quite differently from adults and require a more specialized approach.
Treatment of Type I or Acute Odontoid Synchondrosis
Fractures
The management of acute odontoid synchondrosis fractures in preschool children depends upon the type of fracture according to the classification described originally by Hosalkar et al18. According to this classification, odontoid fractures are categorized into three subtypes with a consideration of the severity of angulation and displacement of the broken dense.
Type Ic which is commonly associated with an angulation of more than 30 degree and a translation greater than 100%, requires C1-C2 surgical intervention. While, type Ia and type Ib can be managed successfully with a conservative approach of treatment.
Type Ia: The most basic form of fracture. This subtype is described aptly as fractures that are associated with either mild odontoid process displacement or mild angulation at or below 10 degrees.8,23 This type is usually easily reducible and will respond without difficulty to hyperextension of the neck.
Type Ib: These are fractures with a displacement of the dense with respect to the axis varying from 10% to less than 100% with an associated angulation that is below 30 degrees. This specific type of fracture will usually respond successfully to cranial traction.9,17,19 Reduction through traction should be a progressive process. It will typically be initiated with 8% of the patient’s body weight and have a gradual increase to a maximum of 7 kg. Digital transoral reduction of the fracture has been undertaken in a few cases and is another mode of reduction that may yield appropriate alignment.32 Close observation and daily sequential lateral cervical radiographs should be obtained in order to monitor this reduction and to avoid distraction and misalignment at the site of fracture.12
In both Type Ia and Ib, after optimal alignment and approximation of the fractured parts either with hyperextension of the neck or skull traction,9,17,19 external immobilization is a standard method for the healing of fractures. This can be achieved either by Minerva cast/orthosis or the use of a halo-vest.20,21,22,23,24,25,26,32,33 However, both Minerva-cast and Halo-cast, despite their use in a few case reports, might be associated with skin sores.17,32 Nonetheless, optimal approximation of the dense to the axis is ideal for solid fusion, it has been shown that 50% of the anatomical contact is sufficient for appropriate solid fusion to occur.
Furthermore, with regards to the capacity of remodeling in children below the age of 3 years, malunion of the odontoid process with respect to the axis and its kyphotic angulation are not problematic but is regarded as a serious sequel of conservative management for older children.34 However, to date, no data exists to validate the occurrence of spontaneous realignment and remodeling during further growth in older children. Nonetheless, overall fusion success across synchondrosis, in type Ia and Ib, with external immobilization, has been observed in 80% -100% of cases, with a mean of 93%.12,18,23,25,26 It should be noted that a lower rate of fusion occurs with Minerva orthosis rather than with Halo orthosis. With Minerva orthosis, non-union and malunion with the displacement of the fractured dense and its angulation is possible. This may occur in spite of the primary anatomical alignment, in particular in non-compliant children. This situation has been directly attributed to reduced immobilization provided through Minerva orthosis. Conversely, Minerva orthosis has been found quite useful in the series reported by Griffth et al and Sherk et al.9,11
Halo Orthosis
Addressing the importance of a high fusion rate, the Halo device has been shown to provide the greatest therapeutic results. Halo was introduced by Perry and Nickel in 1959.35 Its advantages include a rigid external fixation that is accomplished by decreasing cervical motion by 30%-96%. The device adds a level of precise postural control as well. Through the years, Halo has remained a mainstay in the treatment of different cervical spine pathologies due to its consistent attainment of results.36,37 Absolute contraindications for the use of Halo orthosis include cranial fracture, infections, and severe soft-tissue injury at the proposed pin sites. Relative contraindications include severe chest trauma, obesity, advanced age, and a barrel-shaped chest. Kopits and Steingass were the first to use Halo orthosis in children aged between 3 to 10 years. Subsequently, the apparatus was used in the treatment of toddlers and infants. As an example, Mubarak et al25 described the technique he utilized for Halo placement in infants. His study described in detail the successful use of the Halo orthotic in 3 infants.25 A unique consideration for this age group is the presence of open cranial sutures and fontanels in children who are less than 2-years-old .Other notable reports have further illuminated the advantages of using the Halo device in the pediatric population.
Complications in the Use of Halo
Halo-vesting has long been regarded as a useful modality in the treatment of cervical spine trauma in children but has also been associated with a high incidence of complications; the foremost among which are pin-related complications.38,39,40,41,42,43,44,45 The overall complication rate was reported as 53% (36/68) by Limpaphayom et al.43 In this series, 10% (7/68) of the children required unanticipated surgery for the treatment of these complications.43 Indeed the most common complications inherent in the use of Halo fixation in children aged between 3 to 11 years include loosening of the pins and pin site infections. Skull penetration, dural tears, skin breakdown and dysphagia are observed. Spinal fluid leakage and brain abscess formation should be mentioned and can be serious complications associated with this apparatus. According to Baum and Hanley, halo fixation is safe in small children and has a complication rate similar to that found in the older children.40 Pin problems can be treated effectively by standard means. Unique to this age group, toddlers may be more prone to falls than older children, and for this reason, limited ambulation should be recommended.41,45
Pin Site Infection
Pin site infections are the most commonly reported complications of the Halo-vesting when implemented in small children. As an example, out of 68 cases (25%) reported by Limpaphayom et al43 17 cases were indicative of pin site infections following vest placement. Dormans et al39 compared the major and minor complications associated with Halo-vest immobilization in school children and noted that 68% of the children in their study developed some type of complication, the most common of which were pin site infections. Pin site dislodgement and loosening remain the next most common complication followed by skull penetration. If redness and pus drainage occur at the pin site, culture of the sample should always be examined to ensure patient safety.41,45 Appropriate oral antibiotics should be administered blindly after a culture is taken and continued if the culture were to render a positive result. In case of complete failure, the involved pin or pins should be promptly removed, but prior to removal, new pins will be inserted in a new anchoring site. In one study, 13 of the 17 cases with pin site infections reported by Limpaphayom et al43, were resolved with the use of oral antibiotics alone. In the same series; however, it is noted that four pins needed to be removed along with the insertion of a new one.43 Brain abscess is an uncommon but serious consequence of untreated pin site infection.46,47
Pin Loosening and Dislodgement
With the consideration of thinner and much softer skulls of children, skull penetration and pin loosening are more frequent in this age group.39,40,41,42,43,44,45,48,49 Prevention will often require a great amount of care during insertion and some modifications in the number, and perhaps the shape of the pins being used. Furthermore, routine daily activities will increase the potential fordamaging, jarring, and falls, which can result in pin loosening and compromise the Halo fixation.39,40,41,42,43,44,45,48,49 The true reason for pin loosening is thought to be the resorption of bone at the tip of the pin. If pin loosening occurs, it should simply be retightened. Attention to the pins that are being retightened should be given as there is also an existing risk of over-tightening the hardware which could penetrate the skull. If a pin continues to remain loose, the affected pin should be removed. Prior to its removal, placement of a new pin adjacent to the loosened pin will be necessary to ensure the stability of the apparatus. Pin dislodgement and loosening can be minimized through the use of shortened application periods and by using 8 to 12 pins instead of the standard 4 pins. Such an approach will allow for a well-distributed set of pins having low torques but not compromise the overall stability of the device. These modifications can also increase the maintenance of alignment and the chances for optimal fusion with less of a risk for pin loosening.45 Different studies analyzing an eight-pin halo fixation have shown that it can provide greater stiffness than the traditional 4-pin system with a reduced incidence of dislodgement or loosening.51,52 In addition, the crown should also receive more pins which will provide a lower torque insertion with torque values less than 6 inch/pounds.53 To achieve the targeted values, well-calibrated wrenches must be utilized. Skull penetration is much less common than the two previously described complications.
However, every precaution must be undertaken, to counteract the harmful consequences it may render. In order to avoid penetration of the cranial vault, a computed tomography scan of the head should be obtained before the pin placement to determine cranial thickness.48,49,50 Besides the determination of skull thickness, modification in the pin design with a wide flanged and short pin tip might well decrease the possibility of penetration.45
Pin Site Care
All of the above-mentioned three complications can be reduced by means of proper pin site care.54,55,56 Medical literature contains several articles indicating that the use of the Halo device can be relatively safer through daily care and maintenance of pin sites. Caregivers should be monitored weekly by a well-trained family physician or surgeon. Training for the care giver should be a necessary addendum in the undertaking of the Halo procedure in order to ensure the best overall outcome for the patient. This point is best elaborated in a study conducted by Baum et al40 which concluded that in children, the rate of complications can be decreased with close supervision and daily pin site care.
Preferences for cleaning solutions of the pins should be provided daily within the hospital and should be continued daily once the child returns home. Removal of any crusts that may form around the pins should be performed once or twice per day. If drainage is reported, methods of pin site care should be applied up to three times per day as would be needed. A clean cotton tip applicator or gauze should be used for each individual pin site. Cotton applicators should never be shared between pin sites. The pin site should be wrapped with normal-saline-soaked gauze for 15 to 20 minutes and wiped dry following the removal of the gauze.55 Ointments and solutions such as peroxide and chlorhexidine should be avoided because they can be irritating to the skin and potentially lead to skin breakdown. Betadine should not be used since it is known to have corrosive effects on stainless steel pins.55
Other Halo-Vest related Complications
Other less common complications of the Halo-vest are skin breakage, dysphagia and cerebrospinal fluid leakage. Skin breakage may occur along the path or track of the pins as they ascend upward on the individual’s skull. The small tears in the surface of the skin have the potential to become larger open wounds under the pin sites. Though noted, it has seldom been shown to occur as a post-surgical event. To counteract the potential for possible skin rupture, perpendicular pin insertions may be used and have been associated with a lesser likelihood for developing this unwanted complication. Dysphagia is another Halo-related problem once the crown is tightened during hyperextension.57,58 An exaggerated extension positioning of the head and neck may result in swallowing difficulties.58 In the event that this difficulty is developed, a 10 degree correction of the neck position will often eliminate dysphagia.58 CSF leakage and brain abscess formation are extremely rare Halo pin related complications which can be diagnosed and properly treated with a high level of suspicion and proactive monitoring.
CONCLUSION
The treatment of odontoid synchondrosis is not simply confined to subtypes Type Ia and Ib. Type Ic odontoid synchondrosis fractures are more often associated with significant translation and angulation anomalies which are suggestive of a posterior ligamentous disruption. In such cases, a primary posterior C1-C2 fixation must be considered as a potential mode of treatment. C1-C2 screw-rod techniques are generally thought of as the best approaches in the treatment of this subtype of odontoid fracture. However, even within the current decade, cases utilizing posterior laminar wiring or suturing have been reported.
To summarize, the detection of odontoid synchondrosis fractures in recent decades has been frequently reported. Increasing awareness and an increase in the number of global case reports of this condition has supported its identification. Halo orthosis has remained a mode of stabilization in type Ia and Ib acute odontoid synchondrosis fractures which demonstrate mild to moderate angulation and displacement. Each of the three pediatric cases we reviewed within our clinic, have genuinely represented the characteristic aspects of this reasoning. Despite a paucity of contemporary data, the application of Halo-vesting in odontoid synchondrosis fractures has continued to render acceptable results.
ACKNOWLEDGEMENTS
The authors appreciate Dr. Naser Asgari and Mr. Alireza Mojtahed for their efforts in preparing this article.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONSENT
I accept all responsibilities regarding the informed consents of these 3 children which will be published in Orthopedic Research and Traumatology – Open Journal. The informed consents of the parents of these patients has been taken for the study.