INTRODUCTION
Genital Human papillomavirus (HPV) infection is the most common sexually transmitted infection. Although most infections are asymptomatic, a proportion of these infections will result in development of genital abnormalities. Persistent infection with high-risk HPV types is considered necessary for the development of cervical cancer whereas infection with low-risk types is associated with the development of genital warts or condylomata acuminata. Exuberant growth of a condyloma acuminatum is termed ‘giant condyloma’. Giant condylomas usually present in young patients and growth has been associated with impaired immunity (such as infection with the Human Immunodeficiency Virus (HIV)) or pregnancy. Most common sites involved are the vulva, anus, perineum or perianal skin, penis or, more exceptional, at the cervical site. Giant condyloma might result to significant clinical concern as these tumors might mimic malignant tumors. Here, we report, to our knowledge for the first time, a unique presentation of a giant condyloma that had been ‘migrated’ from the cervical site into the uterine cavity.
CASE PRESENTATION
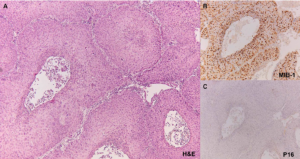
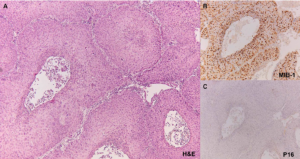
A 59-year-old woman was referred to the gynaecologist because of postmenopausal bleeding and a high-grade abnormality in her cervical Papanicolaou (PAP) test. The medical history included Insulin-dependent diabetes mellitus type 2, hypertension, hypercholesterolemia, heterozygous alpha thalassemia and obesity (Body Mass Index 41.7). The obstetrical and gynaecological history revealed two vaginal deliveries and one abortion. Since 1993, multiple cervical smears with alternating low grade abnormalities (n=3) and normal PAP tests (n=4) were diagnosed. During this period multiple cervical biopsies (n=8) had been performed showing viral changes with low-grade Cervical Intraepithelial Neoplasia (CIN 1). The gynaecologist took a cervical biopsy that showed a condylomatous aspect of the squamous epithelium with viral changes consistent with condyloma acuminatum. However, an endometrial biopsy that was taken at the same time showed an atypical squamous proliferation with severe dysplasia and viral changes (Figure 1). Although contamination from a primary cervical lesion was strongly suspected, immunohistochemical staining for p16 and high-risk Human papillomavirus (HPV) testing by PCR were both negative, which is unusual in highgrade HPV related genital lesions.1 Because of the discrepancy between the low-grade abnormality found in the cervical biopsy and the high-grade abnormalities found in both the cervical PAP test and the endometrial biopsy specimen, a Large Loop Excision of the Transformation Zone (LLETZ) was decided. Again, histopathological evaluation was consistent with condyloma acuminatum. Subsequently, the patient underwent a cervical conisation and additional endometrial curettage, both with the same outcome: condyloma acuminatum in the cervical cone and a high-grade dysplastic squamous lesion in the endometrium. Low-risk HPV testing by PCR turned out to be positive and additional typing showed positivity for HPV type 11. The possibility of a giant condyloma was considered. Given the high-grade dysplastic squamous morphology in the endometrial biopsies, which is an unusual feature in low-risk HPV infections, and the differential diagnosis of an underlying squamous cell carcinoma at the endometrium, a total laparoscopic hysterectomy with bilateral salpingo-oophorectomy had been performed.
Figure 1: Histologic findings of the endometrial biopsy specimen revealed an atypical squamous proliferation with a papillomatous architecture lined by high-grade neoplastic epithelium (A, H&E objective 10x) with increased proliferation activity over full thickness of the epithelium of the epithelium (B, MIB-1 objective 10 x) that was negative for p16 immunohistochemical staining (C, p16 objective 10x).
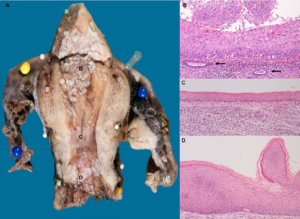
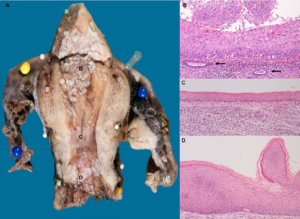
Gross inspection showed exophytic lesions in the cavum uteri (Figure 2). Consistent with the previous findings, microscopic evaluation of the lesions showed viral changes with high-grade dysplasia at the fundus uteri site and low-grade dysplasia at the cervical site. There were no signs of stromal invasion. A line of flat squamous epithelium with normal maturation and without viral changes interconnected the two lesions. Given the presence of HPV type 11 and resuming all histopathological findings, a low-risk HPV positive giant condyloma with highgrade dysplasia was diagnosed. After surgery, the patient recovered well and during a follow up period of 3 years no signs of residual HPV related anogenital disease were present.
Figure 2: Gross specimen of the uterus showed exophytic proliferations at both the fundus and the cervical/isthmus site of the corpus uteri (A). At the fundus site a verrucous high-grade lesion over laid the normal endometrial mucosa (B, H&E objective 10x, arrows indicate underlying endometrial glands). At the cervical/isthmus site (status after prior cervical excisions by LLETZ and cone), a verrucous low-grade lesion with viral changes (D, H&E objective 10x) was present. The verrucous lesions at the fundus uteri and the cervix were connected by flat squamous epithelium without dysplasia and without viral changes (C, H&E objective 10x).
DISCUSSION
Giant condyloma of the anogenital region was first described by Buschke in 1896 and is also known as a BuschkeLöwenstein tumor.2,3,4 This uncommon lesion is caused by HPV.
HPV is the most prevalent sexually transmitted infection and its genotypes can be divided into different groups according to their ability to induce malignancy. Infection with low-risk types can result in genital warts or respiratory papillomatosis whereas infection with high-risk types can lead to malignant transformation of the epithelium in the anogenital or head and neck regions. Mostly, HPV infections are asymptomatic. It is unclear whether HPV infections can silently affect the reproductive function as it appears that HPV can be associated with apoptosis of sperm and embryonic cells and alterations in semen quality.5
Giant condyloma presents clinically as an exuberant exophytic growth of a condyloma acuminatum that typically appears after an infection with the low-risk HPV types 6 or 11 with the anus, penis, perineum, vulva, and to a lesser extent the cervix being the most common affected sites.3,4,6,7 Although invasive squamous cell carcinoma have been reported in about half of the cases it is unclear whether these invasive cases represent true malignant transformation or misclassified cases.6 Because of similarities in exophytic growth patterns the differential diagnosis between giant condyloma, warty, papillary, and verrucous squamous cell carcinoma can be difficult.8,9 In contrast to giant condyloma, warty and papillary squamous cell carcinoma usually show high-grade neoplastic epithelium with areas of typical infiltrative stromal invasion. As these later tumours are positive for high-risk HPV, p16 immunostaining and/or HPV typing can be helpful to differentiate these tumours from giant condyloma. Verrucous carcinomas are not HPV related.8
To our knowledge this is the first report about a giant condyloma that had been ‘migrated’ into the uterine cavity. Although the finding of a squamous proliferation in material derived from the uterine cavity is probably more likely to be the result of extended growth or contamination from a cervical neoplasia, true endometrial involvement by squamous epithelium should be considered as well. Despite the unusual finding of high-grade morphology, lack of stromal invasion in our case supports the benign nature of infections with low-risk HPV types.
CONFLICTS OF INTEREST
There are no potential conflicts of interest to disclose.
CONSENT
We have obtained informed consent of the patient.