INTRODUCTION
The cornea, supplied by the ophthalmic artery throught the ciliary arteries that come to an end near the limbus in the so called pericorneal plexus, is an avascular and transparent tissue. Under normal conditions, such transparency is due to the high level of anti-angiogenic molecules and thus a low level of angiogenic molecules. Any alteration of this balance may cause corneal neovascularization, defined as the growth of new blood vessels from previous capillaries and venules from the pericorneal plexus, which invade the cornea leading to inflammation and chronic corneal edema, lipidic exudation, estromal hemorrhage and corneal scarring. Subsequently, corneal neovascularization may lead to reduced visual acuity and worsening of penetrating queratoplasty prognosis after the alteration of the well-known immune privilege of the cornea.1-4
Prevalence of corneal neovascularization in the United States is known to be 4.14%, presenting 12% of the cases in association with visual loss.1,2 The leading causes of corneal neovascularization are known to be infections, contact lens misuse and the vascular response associated to corneal transplantation.
Now-a-days there is a variety of treatments for corneal neovascularization such as topical corticoesteroids and non-steroidal anti-inflammatories, anti-angiogenic therapies such as bevacizumab, ciclosporine A, diathermy direct occlusion of vessels, topical ascorbic acid, criotherapy, photodynamic theraphy, laser photocoagulation and superficial queratectomy.1,5
The aim of the present paper is to evaluate the efficacy and security of intraestromal bevacizumab combined with fine needle diatermy of corneal neovascularization.
CLINICAL CASE
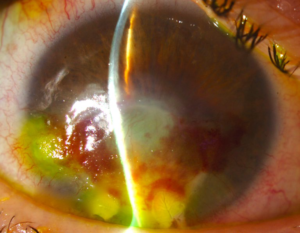
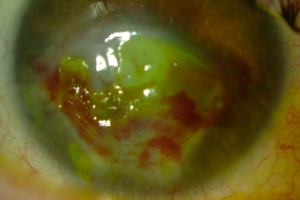
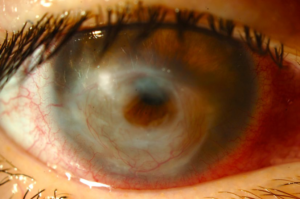
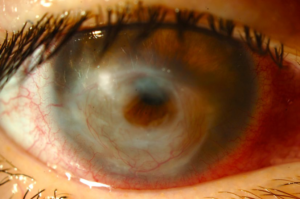
A 44 year-old female presents with lagophtalmos in her right eye (RE) secondary to post-operative facial palsy after acoustic neuroma. Previously treated with hialuronic acid injections in the upper lid, lateral tarsorrhaphy and gold weight eyelid implant, the patient presented with relapsing corneal ulcer and corneal inferior neovascularization resistant to conservative treatment, which led us to treat with fine needle diathermy and intraestromal bevacizumab. Previous topic anaesthetic, intraestromal bevacizumab 2.5 mg/0.1 ml injections were performed with 30 gauge needle along corneal periphery between III and X hours followed by individual cauterization of new vessels located at VI, VII and IX hours with diathermy pencil for phacoemulsification equipment, coagulation mode and fine needle of 27 gauge and 40-50% power until light whitening of corneal estroma. Topic moxifloxacin drops were prescribed during 7 days. First day after, estromal hemorrhages and light epitelial edema on the sites of diathermy needle insertion were found (Figure 1). One week after, some intraestromal hemorrhages still remained but epitelial edema had already solved (Figure 2), observing afterwards a complete resolution of hemorrhages and angioregression of treated corneal new vessels (Figure 3) without ocular perforation.
Figure 1: First day after treatment.
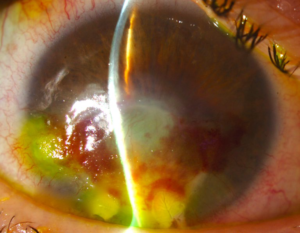
Figure 2: One week after treatment.
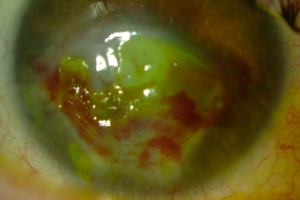
Figure 3:Complete resolution of hemorrhages and angioregression of treated corneal new vessels
DISCUSSION
Corneal neovascularization secondary to a disbalance tipped toward angiogenic factors is a vision threatening complication. The aim of corneal neovascularization treatment is to prevent vascular endothelial cells from proliferating and migrating in response to pro-angiogenic stimuli and thus, the regression of stablished vessels.
Choosing the best treatment depends on the maturation of new vessels. Mature or stablished vessels do not depend on angiogenic mediators and therefore require surgical intervention such as fine needle diathermy. Nonetheless, angiogenic mediators blockage help preventing new vessels to grow if the harmful stimuli persists. Other therapeutic options for mature new vessels are argon laser photocoagulation, photodynamic therapy and cryotherapy.5
First line therapy in every day practice for corneal neovascularization are topical corticosteroids, inhibiting the associated inflammation but not the underlying angiogenic stimuli, effect that was firstly reported in 1950.1 Nevertheless, corticosteroids are mostly effective when administered within the first 24 hours after corneal injury.1,5,6
Vascular endotelial growth factor (VEGF) plays an important part in pathological corneal neovascularization due to his role in the activation, proliferation, migration and vascular endothelial cells differentiation.5 Isoform VEGF-A is known to be the most important hemangiogenesis mediator, playing also a significant role in linphangiogenesis.1,3 Bevacizumab, initially approved by the US Food and Drug Administration (FDA) to treat metastatic colorectal cancer, is a humanized murine monoclonal antibody capable of blocking all VEGF-A isoforms and therefore inhibiting new vessels abnormal formation and diminishing vascular permeability.
Current anti-angiogenic therapy indications include corneal neovascularization, aggresive corneal neovascularization in recurrent pterygium and limbal stem cell deficiency, corneal and iris neovascularization secondary to neovascular glaucoma and corneal graft rejection. Reported Bevacizumab administration ways for corneal neovascularization are topical (5-25 mg/ml, 2-5 times a day), sub-conjuntival injection (1.25 mg/0.05 ml-5 mg/0.2 ml monthly and repetedly if necessary) and intrastromal injection (25 mg/ml: 100 ug per new vessel).1
Anti-angiogenic drugs such as Bevacizumab are known to be more effective in small and medium size vessels recently developed due to the more active release of VEGF and greater angiogenic stimuli. It might not be effective in patients where angiogenesis also depends on different citokines not blocked by Bevacizumab.1
Previous studies have shown the efficacy of topical and sub-conjunctival bevacizumab for corneal neovascularization. The disadvantages of these ways of administration are the diminished penetration and absorption of the drug through the intact corneal epithelium due to its high molecular weight (149 kDa) and the lacrimal clearance, the potential effects of sub-conjuntival administration such as thinning and erosion of the corneal epithelium, conjunctiva and sclera and the high costs of topical preparations.2,5 Nevertheless, higher scientific evidence studies would be needed in order to determine the most efficient way of administration and the dose required to reach and adequate therapeutic concentration and the maximal effect of Bevacizumab for the treatment of corneal neovascularization. Compared to topical corticosteroids, studies do not report important side effects, otherwise bebacizumab tends to be used as adjuvant to corticosteroids rather than to replace them.1
Intrastromal bevacizumab for corneal neovascularization studies have shown hopeful results5,7-9 due to its optimal intracorneal therapeutic levels and it also guarantees a better compliance compared to other ways of administration.4 Nontheless should the security of intraestromal injection be studied. Side effects such as intracorneal hemorrhage, spontaneously absorbed and without sequelae4,9 have been reported. Systemic side effects have not been reported.5,7-9
Few options for the treatment of corneal mature new vessels are available because its vascular wall covered by pericites do not depend of VEGF.6 Fine needle cauterization of afferent and efferent vessels was described by Pillai et al6 for the treatment of 14 patients with corneal neovascularization, obtaining the occlusion of all the vessels in 8 patients, 75% of the vessels in 4 patients and 50% in 2 patients. Four patients required to be retreated. Intraestromal haemorrhages in 3 patients and fine crystalline corneal deposits in one patient, all spontaneously resolved, were reported and no ocular perforation occured in any case.6 Intraestromal haemorrhage is known to occur when the efferent vessel is cauterized before the afferent one, nevertheless diathermy allows the occlusion of both vessels if they are close one another. Fine needle diathermy is a useful, effective, safe and low cost technique for the treatment of stablished or mature corneal new vessels. This technique can also be performed under topical anesthesia.6 Wertheim et al10 showed in 2007 a modified technique using a finer and more flexible electrolysis needle which produces a direct thermic cauterization instead of diathermy. They showed the occlusion of all the new vessels in 3 patients with corneal neovascularization after 8 months of treatment but 2 of them required to be retreated without complications.6
Fine needle diathermy of corneal new vessels attract pro-angiogenic inflammatory cells. Therefore, our aim was to moderate the angiogenic stimulus caused by mature new vessels cauterization through the use of intraestromal Bebacizumab and acting simultaneously over actively growing new vessels. Koenig et al5 reported a statistically significant regression of mature corneal new vessels treated with fine needle coagulation associated to topical bevacizumab (5 mg/mL) 5 times a day during at least 4 weeks in 14 of the 16 patients studied. They concluded that diathermy combined with topical anti-VEGF was a safe and well tolerated treatment for mature corneal new vessels.5 Pillai et al6 reported the occlusion of all mature corneal new vessels in 57.1% of patients using fine needle diathermy as single treatment while Koenig et al5 obtained the occlusion of all new vessels in 68.8% of patients using topical anti-VEGF combined with diathermy.5 This difference probably belongs to the additional use of bebacizumab.
Corneal neovascularization treatment and prevention is a challenge for ophthalmologists due to its significant impact in public health. Traditionally, the treatment of corneal neovascularization was based on corticosteroids, being its response variable. Fine needle diathermy associated with intraestromal bevacizumab allows corneal new vessels regression and should be considered as a simple, effective and low cost therapeutic option for corneal neovascularization. Prospective, double blind, randomized and controlled clinical trials would be needed in order to prove long-term efficacy and security of this therapeutic combination.
PATIENT CONSENT
The patient has consented to the submission of the case report entitled “Fine needle diathermy and intraestromal Bevacizumab: A combined treatment for corneal neovascularization” for submission to The Ophthalmology Open Journal.
CONFLICTS OF INTEREST
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in the manuscript entitled “Fine needle diathermy associated with intraestromal Bevacizumab injection: A combined treatment for corneal neovascularization”.