INTRODUCTION
Extrapleural Solitary fibrous tumor (Extrapleural SFT) is a rare soft tissue tumor originating from mesenchymal cells.1 Extrapleural SFT shows no gender predilection, affecting people across a wide age range, from 5 to 92 years.2 Extrapleural SFT is usually a benign, slow-growing tumor, but a malignant behavior has also been reported.3 Although Extrapleural SFTs most commonly occur in the pleura, numerous extrapleural sites of involvement have been reported.4 We describe a rare case of an Extrapleural SFT in the plantar area of the left foot.
CASE REPORT
A 77-year-old woman was admitted to our hospital for a mass lesion in the plantar area of the left foot. The mass was present for about 30 years but it had never been treated before because stable in size over time and asymptomatic. However, the patient recently complained of pain in the sole of her foot after long distance walking.
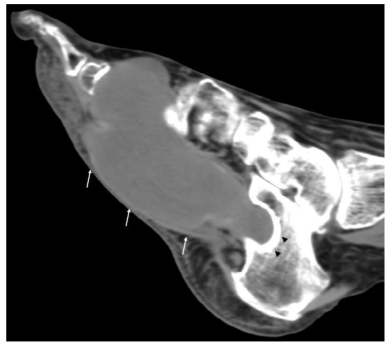
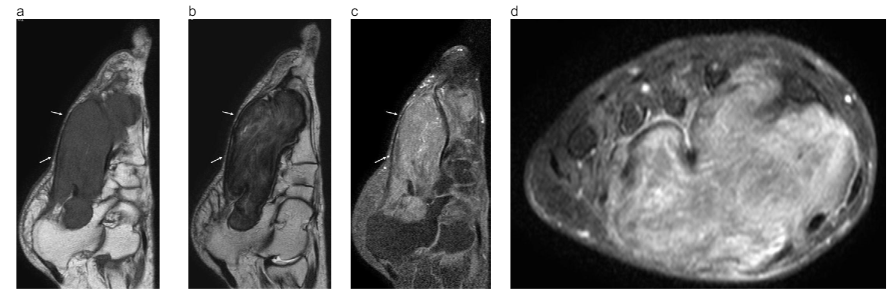
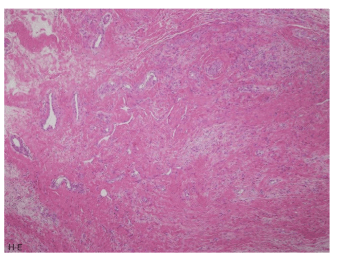
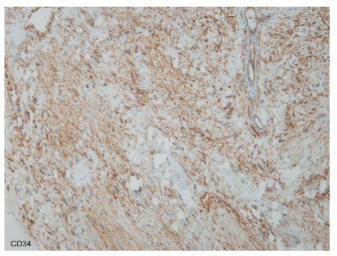
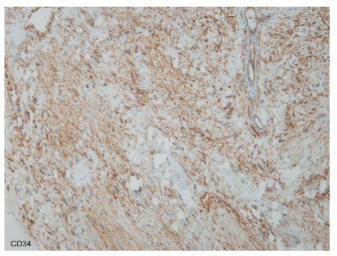
The patient was affected by Alzheimer-type senile dementia and by poor controlled diabetes mellitus. On physical examination, the plantar mass was about 7 cm in diameter, elastic and hard to move. The skin overlying the mass was not red or blistered. Foot X-rays showed marked pressure erosions in the second and third metarsal bones due to a compression by the mass (Figure 1, arrows). Toes of the left foot showed osteopenic change suggestive of osteoporosis. On foot CT, a low density tumor measuring 10 cm in diameter was present in the plantar area (Figure 2, arrows). The calcaneus showed erosive changes which sclerotic margin for the long-lasting compression by the tumor (Figure 2, arrowheads). The deformity of the metatarsal bones showed the same Computed Tomographic (CT) finding as the one of the calcaneus (not shown). Foot MRI (1.5 Tesla Achiva Philips, Netherlands, USA) reviewed a low signal intensity tumor on both T1 weighted (TR 465 msec, TE 12 msec, Thickness 3.5 mm, FOV 220 mm), and T2 weighted images (TR 2929 msec, TE 30 msec, Thickness 3.5 mm, FOV 220 mm) (Figures 3a and 3b), and well-enhancement on gadolinium-enhanced fat suppression T1 weighted sagittal image (TR 625.7 msec, TE 12 m sec, Thickness 3.5 mm, FOV 220 mm) (Figures 3c and 3d) in the left sole, from the calcaneus to the first metatarsal head. The tumor involved the adductor and the abductor hallucis muscle, the flexor digitorum longus and brevis tendons, the flexor digitorum brevis muscle and the quadratus plantae muscle (Figure 3d). Despite the tumor compression, the first to third metatarsal and the calcaneus bones showed no bone marrow edema. Considering patient clinical history and presentation and MRI findings, we initially suspected a fibroproliferative neoplasm like an aggressive fibromatosis. An open biopsy under local anesthesia was then performed. Histologically the lesion was benign fibroblastic spindle cell lesion with dense or loose collagen fibers. Cellularity was low and no mitotic figures were found (Figure 4). The tumor cells were positive for CD34 (Figure 5), whereas they were negative for α smooth muscle actin, desmin, HHF35 and S100 protein. Although blood vessels including stag-horn like ones were indistinct, we made diagnosis of extrapleural solitary fibrous tumor (extrapleural SFT). We tried to recommend a complete surgical excision of the lesion but the patient conditions due to the Alzheimer-type senile dementia progressed and she was eventually sent to a mental hospital.
Figure 1: Anterio-posterior view of left foot X-ray. A soft tissue density mass is present under the first to third metatarsal bones. The second and third metatarsal bones show a severe deformity due to the soft tissue density mass. Widening between the first and second metatarsal bone is visualized (arrows).

Figure 2: Foot CT (soft tissue window). A huge mass lesion is visualized in the sole (arrows). The mass lesion shows relatively homogenous low density with clear margin. The calcaneus is involved by the mass but the margin of it shows osteosclerotic change suggestive of slow glowing tumor.
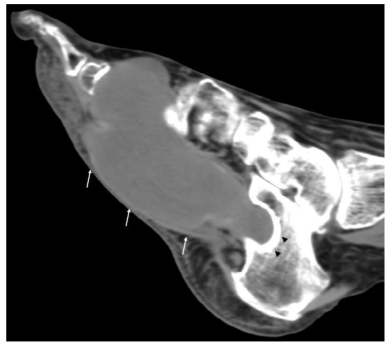
Figure 3: Foot MRI a) T1-weighted sagittal image, b) T2-weighted sagittal image, c) gadolinium-enhanced fat suppression T1-weighted sagittal image, d) gadolinium-enhanced fat suppression T1-weighted coronal image.
a. The mass lesion in the sole shows low signal intensity (arrows) on T1-weigted sagittal image. The plantar fascia is present along the mass lesion without involvement. Subcutameus fat tissue and the skin of the sole are intact. There are no bone marrow edemas in the calcaneus or other bones.
b. The mass lesion shows heavy low signal intensity on T2-weighted sagittal image (arrows). The mass includes some high signal contents suggestive of myxoid or hyalinized in areas.
c. The mass lesion is homogenously enhanced (arrows). Calcaneus and other bones are not enhanced.
d. The mass lesion involves almost plantar muscles: an adductor hallucis muscle, an abductor hallucis muscle, long and short digital flexor tendons, a flexor digitorum brevis muscle and quadratus plantae muscle.
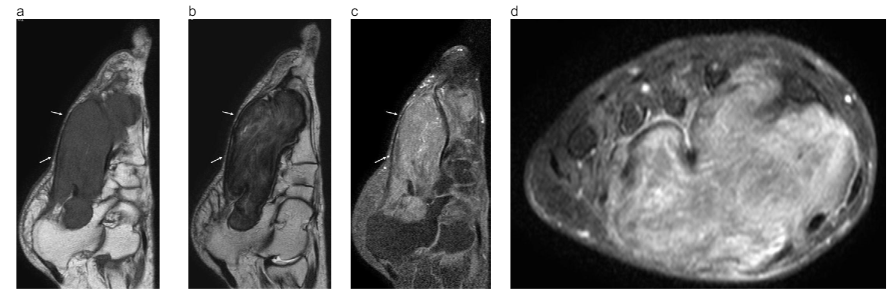
Figure 4: Hematoxylin and eosin stain (H-E stain). The tumor composes of small ovoid to spindle cells separated by thin bands of collagen fibers. Branching blood vessels and stromal hyalinization were visualized within it.
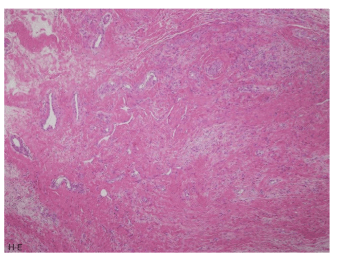
Figure 5: Immunohistochemical staining (CD34 staining). CD34 staining is positive. Both Desmin and S-100 protein staining are negative (not shown).
DISCUSSION
Extrapleural SFTs have been reported in several anatomical sites: nasal and paranasal sinus,5 spine,6 lung,7 mediastinum, pancreas,8 liver,9 kidney, retroperitoneal space,10 urinary bladder,11 and extremities.12 From the clinical point of view, an extrapleural SFT is usually a painless mass in the deep soft tissue without specific symptoms.13 extrapleural SFT can show both benign and malignant behavior. From 10% to 15% of the tumors are malignant, occurring with more frequency in the cellular than in the fibrous forms.14 In the literature only few authors have reported SFT involving the extremities.12,15,16 Musyoki FN et al16 highlighted the orbits and the extremities (proximal extremities muscles and subcutaneous tissues) as the most common extrapleural SFT extrapleural location. Despite that, foot and ankle involvement is even less described. Lee JY et al14 reported the first case of an extrapleural SFT arising from the ankle in a 69-year-old female patient and treated by total excision. Kean CA et al17 described a rare manifestation of extrapleural SFT in a 55-year-old male patient affecting the medial right hallux: also in this case the treatment of choice was represented by the excision in toto. To the best of our knowledge, this is never say “the first” report of an extrapleural SFT in the foot affecting the plantar muscles. In addition, many authors reported that the majority of these tumors (80%) showed hypointense or isointense on T1-weighted image relative to muscle, and hypointense on T2-weighted image.12,13,14,15,16,17,18,19 On the other hand, Shin JH et al20 reported that the extrapleural SFT in the buccal space showed hyperintense on T2-weighted image. Contrast enhanced MRI shows heterogeneous in as many as 82% of extrapleural SFT cases, and homogeneous enhancement effect in approximately 18%.16,18,19 In our case, the mass showed very low signal intensity on T2-weighted image. This peculiar aspect could be the result of 30 years of exerted compression on the extrapleural SFT which may have cause hemorrhage, reactive fibroplasia, and/or calcification. We didn’t detect any hemosiderin deposits or calcification on MRI and we therefore considered it as a reactive fibroplasia occurred on this tumor.
Considering the histo-pathological features, World Health Organization (WHO) classification of tumors of soft tissue and bone has been revised since 2013.21 A notable point is what the expleural SFT has combinated two soft tissue tumors called hemangiopericytoma and giant cell angiofibroma because their pathological findings are similar to the extrapleural SFT. We might have to reconsider MRI findings of the extrapleural SFT. Generally, an extrapleural SFT can vary in size, ranging from 1 cm to 30 cm.22 On light microscopy, a common histological feature of both pleural and extrapleural solitary fibrous tumor is a mixture of three components, namely, fibrous tissue, cellular components, and highly vascularized areas that consist of numerous dilated small to medium-sized blood vessels. On Immunohistochemical staining, positive CD34 and negative S-100 protein staining are typical for the extrapleural SFTs. The extrapleural SFT should be included in the differential diagnosis of extrapleural lesions in which MRI suggests fibrous content. Moreover, the differential diagnosis of extrapleural SFT includes fibromatosis, myofibroblastoma, metastasis of spindle cell carcinoma, low-grade fibromyxoid sarcoma and hemangioma.16 Clinical and imaging features of extrapleural SFTs also overlap with other fibrous tumors such as fibrous histiocytoma, fibrosarcoma and synovial sarcoma. These entities exhibit a dense fibrocollagenous matrix that can produce low signal intensity on T2-weighted MRI images, similar to extrapleural SFT. Despite our patient conditions did not allow any therapy, the treatment of choice for extrapleural SFT is total surgical excision, associated with long-term follow-up in order to early identify possible recurrence or malignant changes.14 In case of inoperable extrapleural SFT or incomplete excision, the use of radiotherapy or chemotherapy can increase the survival rate.16
CONCLUSION
SFT has been reported in a wide variety of extrapleural locations and is extremely rare in foot and ankle. Prolonged weight-bering might cause bleeding and lead to a reactive fibroplasia, affecting the signal on MRI.
Diagnosis of extrapleural SFT is often challenging. In order to reach a proper diagnosis and treatment is essential to integrate a detailed patients’ clinical history and to perform a biopsy to collect cells for closer examination.
CONFLICTS OF INTEREST: None.
CONSENT
The patient has provided written permission for publication of the case details.