INTRODUCTION
Genuine stress urinary incontinence (GSUI) is a common bothersome medical condition affecting primarily parous older women. It is estimated that more than thirty million women suffer from the condition in North America alone1 and about 25% of women are expected to suffer from symptomatic GSUI at some point in their lifetime.2
Obesity, multiparity, chronic obstructive pulmonary disease and previous hysterectomy are all independent risk factors for the disease.3 GSUI is debilitating when patients are compelled to limit their fluid intake or to limit their physical activity in order to control symptoms of the disease.4
The underlying pathophysiology of GSUI is generally considered to be due to laxity of the pelvic floor muscles resulting from labor and delivery.5,6 As a result of this relaxation the bladder outlet continence mechanism does not function properly, and urine leakage can occur during episodes of increased abdominal pressure. The precise etiology and pathophysiology of the disease is still unclear and GSUI can also occur in nuliparous women.7
Weight loss,8 risk factor management and physiotherapy9 are all helpful in controlling the symptoms of GSUI. Symptomatic patients who do not improve with non-surgical management usually proceed to a minimally invasive surgical procedure involving placement of a polymer micromesh “tape” implant.
The tension free vaginal tape (TVT) procedure was first introduced in 2001 by Dr. C Falconer10 and it has revolutionized the surgical treatment of GSUI with an overall satisfaction rate of over 90%.11 A trans-obterator tape procedure for GSUI was first proposed by Delorme in 2001 and has gained in popularity as it is less invasive than the original TVT.12 The MonarcR-TOT procedure is a variation of tape suspension inspired by Delorme. TVT (and its variants) is not always successful however, and the reason(s) for failure are not always known.13
The normal physiology of the female pelvic floor has proved uniquely difficult to study.14 Beginning in the 1960’s multichannel urodynamics has been used to characterize pressure changes between the bladder and the urethra. Over the years ambulatory urodynamics was developed as an investigative tool to control for postural changes in incontinent subjects.15 The more recent addition of video-urodynamics and dynamic magnetic resonance imaging (MRI) has further improved our understanding of female pelvic floor function.16 However, a complete picture of normal pelvic floor function continues to elude us.
Contributing to the difficulty in female pelvic floor assessment is the problem of testing patients in the upright position.17 In addition, trans-urethral pressure probes can interfere with bladder functioning during testing by stimulating the rather sensitive surfaces within the urethra and within the bladder itself. The result of this iatrogenic stimulation can lead unwelcome artifact on urodynamics testing.18
The gradual advancement of MRI technology has led to the development of upright (open positional) imaging systems.19 The newer upright MRI systems were first introduced in 2008 and allow for the MRI assessment of anatomical changes related to position and weight bearing. Upright MRI is currently most used to evaluate vertebral changes created by stress loading. This prospective cohort study is the first to use upright MRI in the investigation of GSUI in women.
Aim
To gather anatomical data of the female pelvic floor using an upright MRI scanner in women who are known to have type 2 GSUI before and then after MonarcR Trans-obterator tape (American Medical Systems, Minnetonka, MN, USA) suspension. Concurrent collection of psychometrically valid symptom scores will allow for direct comparison of symptom changes to the anatomical changes noted on upright MRI.
MATERIALS AND METHODS
Thirty otherwise healthy multiparous female MonarcR TOT candidates with proven GSUI were recruited from participating surgeons to take part in the study. Subjects were excluded from the study if they had any element of an overactive, uninhibited, or small capacity (<200 ml) bladder. Any history of endometriosis or ongoing pelvic pain led to exclusion from the study as did any preoperative evidence of microhematuria or leukocyturia. A history of urinary tract infection within three-months of recruitment also led to exclusion from the study. These criteria were established during the process of recruitment by the participating surgeons.
Prospective trial protocol approval was obtained from the Western Institutional Review Board (IRB) (WIRB study # 1134614, protocol # 20121442) prior to, and at regular periods during, the course of the 22-month trial in accordance with the revised Declaration of Helsinki of 1989.
Each participant in the study had a history of GSUI type 2 with a diagnosis considered “very likely” after history and physical examination by a participating urologist or gynecologist. Each patient then completed an initial 12 question 48-point international consultation on incontinence questionnaire female lower urinary tract symptoms modules (ICIQ-FLUTS) questionnaire20 (ICIQ group, Bristol Urological Institute, Southmead Hospital, Bristol, UK). A comprehensive informed consent was then obtained from each subject. After completing the symptom score and consent form each patient was then asked to void completely.
After each patient had emptied their bladder completely, a sterile #14 French catheter was inserted in their urethra and 300 ml of sterile water was instilled into their bladder and left to dwell. Any residual urine was removed from the patients bladder at the time the catheter was inserted. After standardizing for bladder volume of 300 ml each participant was transferred to a nearby FonarR (Fonar Corporation, Melville, NY, USA) 0.6 T-upright MRI machine. Once inside the MRI suite each subject underwent a pelvic MRI scanning series while standing at rest. A second series of pelvic MRI images was then obtained as each subject was asked to perform a standardized Valsalva’s maneuver. In order to standardize the Valsalva21 maneuver a Laborie (Laborie International, Mississauga, Ontario, Canada) PeritronR digital pressure gauge was used. Each subject was asked to blow into a custom made 3 m tube producing an abdominal pressure of 53 mmHg. The PeritronR device was adjusted to deliver auditory and visual feedback to each research subject so that appropriate standardized pressure could be maintained for the eight seconds that were necessary to obtain an adequate image. During this process, each subject was monitored by the principal investigator in the study to ensure compliance. Finally, each subject was asked to void completely and subsequently an abdominal MRI series was obtained while each subject was supine.
After the MRI data was acquired it was saved to a secure database (McKesson, one post street, San Francisco California, USA) and each patient then went on to have a MonarcR-TOT type bladder neck suspension. Each MonarcR-TOT suspension was carried out in a standardized manner by one of five separate participating surgeons. After the surgery, each subject waited a minimum of three months before returning to the MRI suite for a follow-up MRI study series. Each follow-up study was performed using the same protocol as the preliminary study, but an abdominal series was not collected on the second study.
The second series of MRI images were again stored to a secure imaging database and symptom score results were stored to a secure Excel® database (Microsoft, 15010 Northeast 56th Street, Redmond, Washington, USA) which was operating on a PC compatible laptop computer.
The many MRI images that were collected were then evaluated by a qualified radiologist who classified and calibrated pelvic floor findings using the “Health Maintenance Organization (HMO)” grading system originally proposed by Drs. C. Comiter and S. Raz in 1999.22 Pelvic floor excursion was carefully mapped out using the HMO system and an ordinal number approach was used to allow for direct statistical comparison(s) between the ICIQ-FLUTS results and the MRI results.23
The pre- and post-operative MRI results were then carefully compared and correlated to the pre- and post-operative ICIQ-FLUTS symptom score data using the statistical method of Spearman’s rank correlation. The results of the analysis are presented below followed by a discussion of their significance.
RESULTS
Of the 30 patient subjects recruited into the study 27 completed the two-part MRI series and MonarcR-TOT surgery. Two subjects finished the first MRI series and the surgery but were then lost to follow-up. A third subject could not complete the first MRI series due to discomfort related to initial urethral catheterization.
The twenty-seven patients who completed the study had a median age of 51.5-years and an average age of 51.5-years. The observed population had an average weight of 75.5 Kg and the groups average body mass index (BMI) was 28.13. The youngest patient in the study was 35-years-old and the oldest was 82.
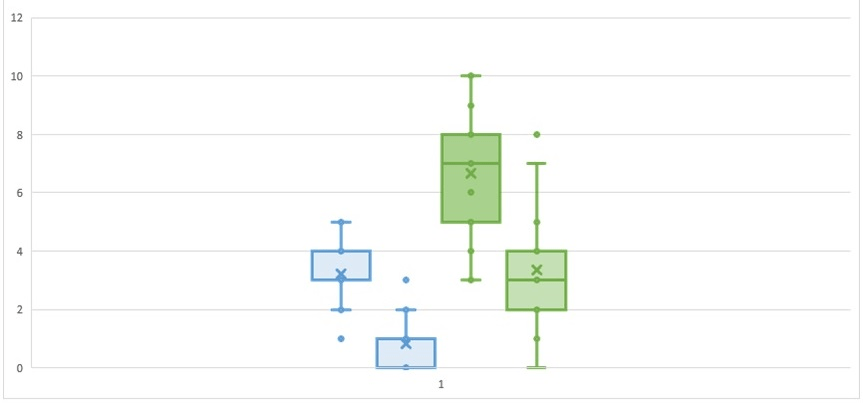
The average pre-operative ICIQ-FLUTS result was 19.96 (normal<5) improving to 11.15 post-operative. The average improvement in ICIQ-FLUTS was therefore 8.81 points (Figure 1).
Figure 1. Box and Whisker Plot Showing the ICIQ-FLUTS Scores to Question 11. A) Preand Post-Monarc Suspension with Upper and Lower Quartiles (Blue). The ICIQ-FLUTS Scores and Quartiles for Question 11. B) Pre- and Post-Monarc are Shown in Green
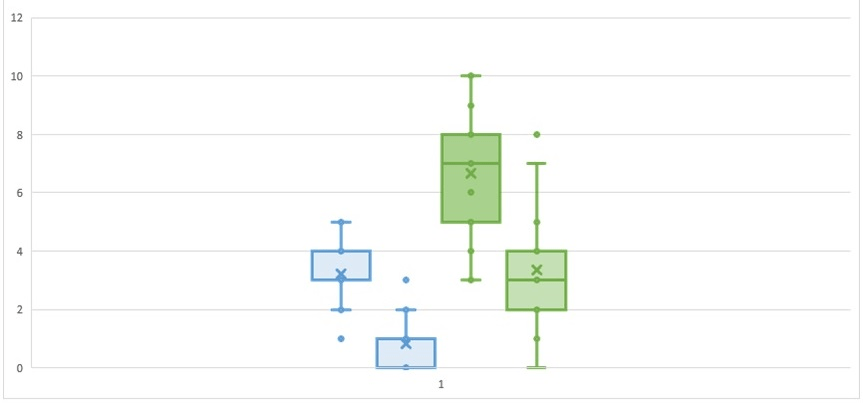
The above box and whisker chart illustrates the response by patients to Questions 11. A and 11. B before and then after MonarcR suspension. Question 11. A asks: “Does urine leak when you are physically active, exert yourself, or sneeze?” (score out of 5). Question 11. B asks: “How much does this bother you?” (score out of 10).
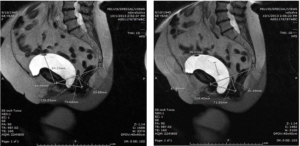
The MRI process, which included standardizing bladder volume and a standardized Valsalva’s maneuver, was well tolerated by all patients. There were no patient dropouts during either MRI series, or all the image outcomes were of diagnostic quality (Figure 2).
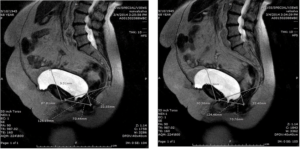
Figure 2. Sample of Two Pre-operative Images from One Patient (T2-weighted Image, Sagittal Section) in the First Upright MRI Series
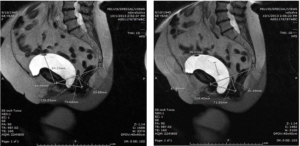
A sample of two pre-operative images from one patient (T2 weighted image, sagittal section) in the first upright MRI series. These two images show the measurements taken using the “HMO” system of S Raz. Image 1 was taken “standing at rest” while image 2 was taken “standing with standardized Valsalva”. The first image shows that the lowest point of the bladder floor reaches 24.1 mm below the pubococcygeal line (PCL) while the patient is at rest. With Valsalva this distance increases to 36.23 mm for a pelvic floor “excursion” of 12.13 mm.
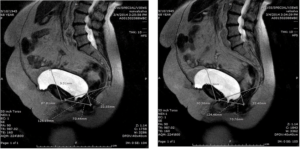
A sample of two post-operative T2 weighted MRI images developed from the same patient as in Figure 3. Again, the first sagittal image shows the patient while “standing at rest”. The second sagittal image shows the patient while “standing with Valsalva”. The most dependent portion of the bladder in image 1 protrudes 9.31 mm past the PCL while in image 2 the protrusion is measured at 14.18 mm for an excursion of 4.87 mm. Comparison of the pre-operative to the post-operative result indicates a pre-op to post-operative “reduction of excursion with Valsalva” of 7.26 mm.
Figure 3. Sample of Two Post-operative T2-Weighted MRI Images
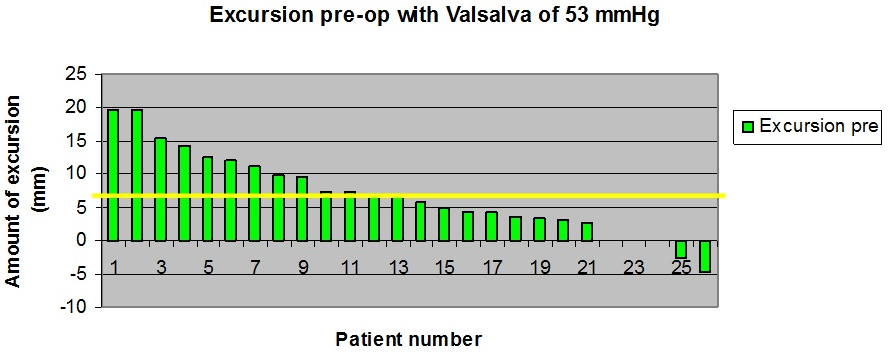
A wide range of pre-operative pelvic floor excursion results were obtained. The greatest degree of excursion prior to surgery with Valsalva was 19 mm and the least amount of excursion was positive 4 mm — that is 4 mm less protrusion with Valsalva than at rest (Figure 4).
Figure 4. Histogram Showing Pelvic Floor Excursion Results with Valsalva in mm for All 27 Subjects
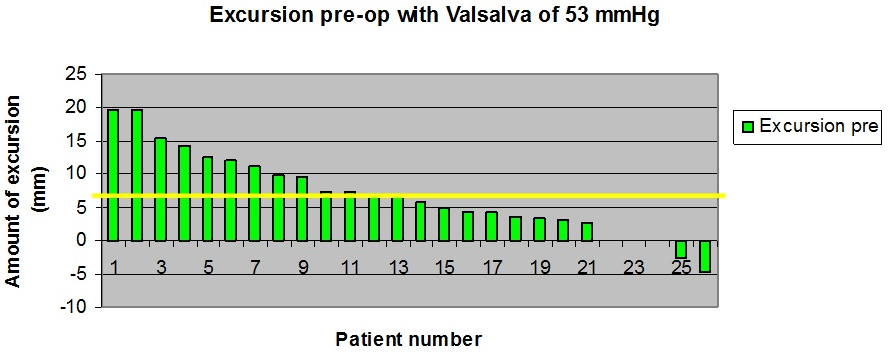
Histogram showing pelvic floor excursion results with Valsalva in mm for all 27 subjects. The greatest amount of excursion prior to MonarcR-TOT was 19 mm and the least amount of excursion was +4 mm. The pre-operative average excursion distance with standardized Valsalva’s maneuver was 6.83 mm.
When the same measurements were taken three months after MonarcR-TOT an average excursion with Valsalva of 4.41 mm was recorded. The average “reduction of excursion attributable to surgery was therefore 2.43 mm (Figure 5). Interestingly, eight patients had more pelvic floor excursion following surgery than before surgery. The cause of this result is not immediately apparent.
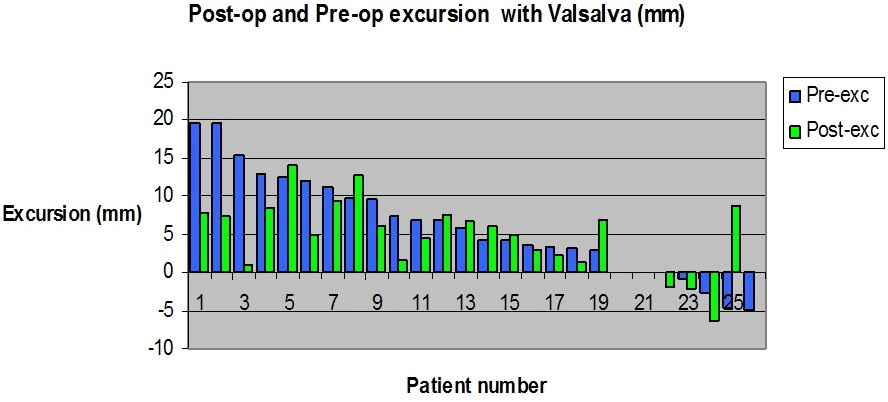
Figure 5. A Histogram with Direct Comparison of Pre-operative and Post-operative Pelvic Floor Excursion with Standardized Valsalva’s Maneuve
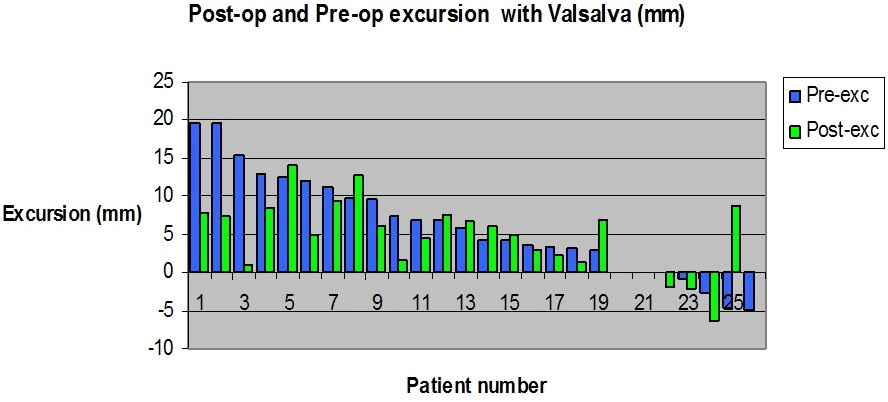
A histogram with direct comparison of pre-operative and post-operative pelvic floor excursion with standardized Valsalva’s maneuver is presented. Prior to surgery an average excursion with Valsalva of 6.83 mm was recorded. Following surgery this drops to 4.41 mm for an average reduction of 2.43 mm attributable to MonarcR-TOT surgery. It is notable however, that eight of twenty-seven patients had more pelvic floor excursion after surgery than before.
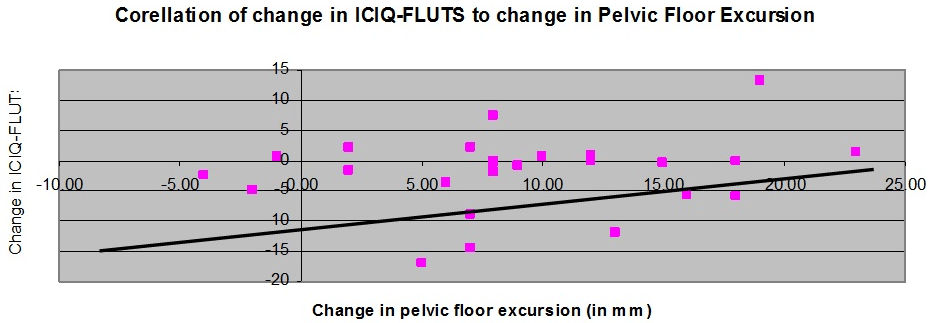
To compare and correlate the ICIQ-FLUTS results with the upright MRI results directly a Spearman’s rank correlation test was used. This statistical procedure was performed by making a comparison of pre-operative/post-operative change in pelvic floor excursion results with the pre-operative/post-operative change in ICIQ-FLUTS results. The Spearman’s rank correlation equation (rs=1–6 Σd2 /n(n2–1)) was used and the statistical operation was performed using ExcelR (Figure 6).
Figure 6. A Scatter Graph (with trend line) Comparing the Change in Pelvic Floor Excursion (vertical axis in mm) to the Change in the ICIQ-FLUTS Result (horizontal axis)
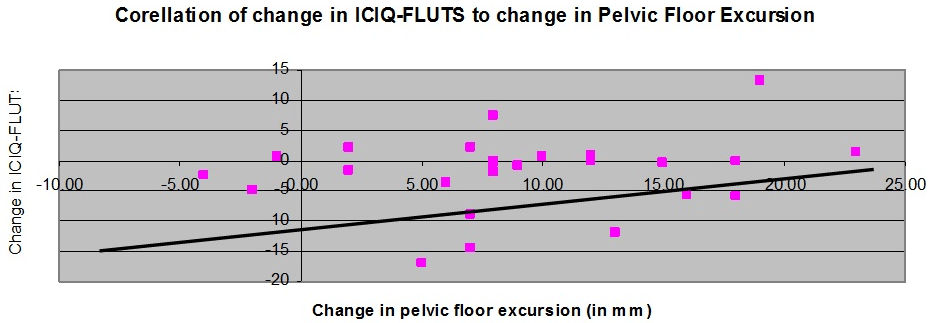
A scatter graph (with trend line) comparing the change in pelvic floor excursion (vertical axis in mm) to the change in the ICIQ-FLUTS result (horizontal axis). Spearman’s rank correlation rs=0.18206. The result indicates a moderate positive correlation and is statistically significant (p<0.001).
DISCUSSION
Almost as soon as MRI became clinically available efforts were made to use the imaging technique to investigate the female pelvis.24,25,26 The advantages of MRI include lack of ionizing radiation, a clear depiction of the soft tissues of the pelvic floor, and multiplanar imaging capability. Conventional MRI produces static T1-images and spin echo T2-weighted images. Although useful, standard MRI is limited by its long image acquisition time and by the requirement that the patient be in the supine position.
Using the above-mentioned techniques, the functional anatomy of the female pelvic floor was examined, and studies also began to use MRI to evaluate the soft tissue changes associated with GSUI. In 1995 several studies used conventional MRI to investigate anatomical changes associated with incontinence and prolapse surgery. One study used classical supine MRI to evaluate postural changes occurring in the pelvic floor of healthy continent women.27
The development of ultra fast MRI image acquisition (single-shot fast spin echo SSFSE and single-shot turbo spin echo HASTE) and the use of single shot sequencing with a cinematic (or dynamic) display added an additional improvement in the understanding of functional anatomy of the female pelvic floor.28,29 The introduction of dynamic MRI in 1999 generated great interest as the interaction of anatomical pathology and the pathophysiology of GSUI became clearly visible for the first time.30 In 1999 Drs. Comiter and Raz developed a standardized nomenclature for grading pelvic prolapse and pelvic floor relaxation in dynamic MRI imagery and this diagnostic system has been widely adopted.31
A practical application for MRI in the setting of incontinence has however not yet been developed. While interesting and less invasive, the techniques of supine MRI and dynamic MRI have not been generally adopted as routinely useful.32
In the present study upright MRI is used in combination with standardized testing to investigate a cohort of GSUI patients before and after MonarcR-TOT surgery. Twenty-seven human subjects with known GSUI were recruited and investigated prospectively with upright MRI. Pre-operative and post-operative MRI data was collected and compared with a psychometrically valid symptom score. Data were carefully collected over a two-year period and appropriate statistical tests were used to demonstrate a significant positive correlation between the changes in patient’s incontinence symptoms and the changes in pelvic floor movement.
This study marks the first time that psychometrically valid symptom score improvements and objective pelvic floor anatomy improvements have been definitively linked as being due to the same surgical intervention in GSUI patients.
This result is significant as it demonstrates that the reductions in pelvic floor excursion achieved by MonarcR-TOT can be objectively linked to the positive clinical outcomes recorded by ICIQ-FLUTS. The symptom improvements long known to be due to trans-obterator tape suspension are thus demonstrated to be objectively correlated to anatomical changes generated by the surgery.
CONCLUSION
In conclusion, upright MRI investigation using this methodology may prove to be useful as a less invasive alternative to urodynamic testing in a subgroup of patient’s prior GSUI surgery. As open positional and upright MRI systems become more widely available these methods may prove to be useful clinically for some GSUI patients.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.