INTRODUCTION
Cervical ossification of posterior longitudinal ligament (OPLL) is a common disease among the elderly population of East Asian countries, especially Japan, Korea, and China. The incidence of OPLL is 2.4% in the Asian population, and 0.16% in the non-Asian population.1 OPLL is twice as common in men as it is in women, and symptomatic OPLL such as cervical myelopathy and/or radiculopathy often at times manifests itself in the 5th and 6th decades of life.2 Cervical OPLL can be misdiagnosed in lateral radiography or magnetic resonance imaging (MRI). In the present study, the diagnostic accuracy of cervical OPLL in lateral radiography and MRI is compared to computed tomography (CT).
METHODS AND MATERIALS
This study was approved by our Institutional Review Board (IRB), and informed consent was obtained from all patients. A retrospective study was performed in the Tokyo Dental College Ichikawa General Hospital from January 2014 to December 2015. A total of 60 Japanese patients were diagnosed with cervical OPLL by CT. All patients acquired cervical X-ray, CT and MRI scan and underwent posterior decompression surgery after diagnosis. There were 53 males and 7 females (mean age: 63.6 years, age range: 40-81years). All patients had pain in the upper extremities, numbness, and paresthesia due to myelopathy with or without radiculopathy. First, a lateral radiograph was obtained and regarded a high-density structure along the posterior aspect of vertebral bodies as corresponding to a diagnosis of OPLL. Next, a T2 weighted MRI sagittal image was secured demonstrating a thick low-signal posterior longitudinal ligament. This phenomenon was regarded as OPLL. Finally, a cervical CT was evaluated and images were identified in which OPLL was present. The diagnostic accuracy of lateral radiograph and MRI was evaluated, along with speculations as to the probable causes of misdiagnosis. All images were reviewed by a certified spine surgeon and a certified radiologist, and the diagnosis was achieved by consensus.
Instrumentation/imaging modalities included: 1.5 Tesla Achiva Philips, Netherlands. T2 weighted sagittal (FOV: 250 mm, TR/TE: 3000/100 msec, slice thickness: 4 mm, gap: 0.4 mm, axial (FOV 180 mm, TR/TE 3000-7225/100 msec, thickness: 3 mm, gap: 0.7 mm), and T1 weighted sagittal (FOV: 250 m, TR/TE: 400/11 msec, slice thickness: 4 mm, gap: 0.4 mm) of MR sequences were performed. Axial and reconstructed sagittal cervical spine CT (Bliriance 64, Philips, Netherlands) was performed in order to correlate the MR findings and confirm the presence of ossification. Each CT scan was reconstructed using a 2 mm slice thickness.
Diagnostic Criteria of OPLL
The classification of OPLL is commonly formulated by the method described by Investigation Committee on OPLL of the Japanese Ministry of Public Health and Welfare.1 On the basis of this method, OPLL is classified as local type, segmental type, continuous type, and mixed type as determined by plain radiographic findings. However, we did not use this classification because our purpose was to investigate the accuracy of OPLL in each modality.
X-ray
OPLL was visualized by dots or band-like dense structures along the posterior aspect of vertebral bodies as observed in the lateral radiograph of cervical spine.
MRI
OPLL was diagnosed as a thick posterior longitudinal ligament with low signal intensity as compared to the one at the level of thoracic spine in contrast to the sagittal image obtained on a T2 weighted MRI. If both T1 and T2 weighted sagittal images showed partially high signal intensity within a thick posterior longitudinal ligament, the assumption was made of OPLL.
CT
OPLL was diagnosed as dots or a band-like high density structure at posterior longitudinal ligament on the reconstructed multi-planar reconstruction (MPR) sagittal CT image. The presence of OPLL was investigated at selected cervical levels. The OPLL on CT was the standard for comparison for both X-ray and MRI.
RESULTS
Overall diagnostic accuracy using lateral radiograph and MRI was 20% (12/60) (Figure 1) and 25% (15/60) (Figure 2) respectively. Only 5 out of the 60 cases showed evidence of OPLL in all three modalities (Figure 3). Regarding each vertebral level of OPLL on CT, C2 (18/6), C3 (36/18), C4 (49/60), C5 (47/60), C6 (47/60) and C7 (21/60) were detected. The accuracy in using lateral radiograph and MRI of each C2, C3, C4, C5, C6, C7 was C2 (88.8% (16/18) and 100% (18/18)), C3 (88.8% (32/38) and 100% (38/38)), C4 (79.5% (39/49) and 97.9% 48/49)), C5 (95.5% (45/47) and 110.6% (52/47)), C6 (42.5% (20/47) and 70.2% (33/47)) and C7 (23.8% (3/21) and 66.6% (14/21)). These results have been shown in Table 1.
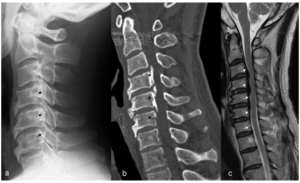
Figure 1: OPLL Diagnosis using X-rays and CT: 56-Year-Old Male.
a. Lateral radiograph: Band like ossification is present along the vertebral body at level of C4, C5 and C6 (arrows). Some spur formations and ossification of the anterior longitudinal ligament are also seen at the level of C4-5, C5/6 and C6/7.
b. MPR sagittal image of cervical spine CT after myelography: The longitudinal ligament shows high density suggestive of ossification at the level of C4, C5 and C6 (arrows). The ossification at the level of C6 is smaller than the one at other levels. Cervical canal is narrow due to the OPLL at level of C4 and C5.
c. T2 weighted sagittal MR image: The longitudinal ligament shows partial thickening at the level of C3, C4, C5, C6, and C7. This range is longer than both the X-ray and CT. Suspected cervical cord compression at C3/4 and C4/5 levels.
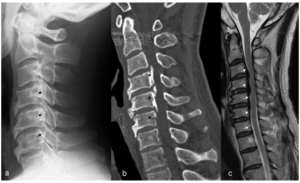
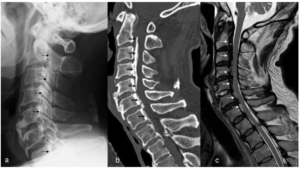
Figure 2. OPLL Diagnosis using MRI and CT: 72-Year-Old Male.
a. Lateral radiograph: Dense lesion known as ossification is present at the level of C2, C3, C4, C5 and C7 (arrows). Ossification at C6 level is indistinct. Some spur formations and ossification of anterior longitudinal ligament are visualized at level of C5/6 and C6/7.
b. MPR sagittal image of cervical spine CT: The longitudinal ligament shows diffuse ossification from C2 to C7 (arrows). Cervical canal is narrow due to OPLL.
c. T2 weighted sagittal MR image: Diffuse longitudinal ligament thickening with irregular margin is present from C2 to C7 (arrows). Suspected cervical cord compression from C3 to C6.
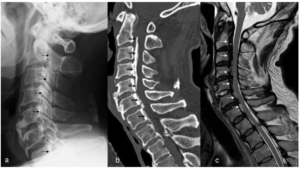
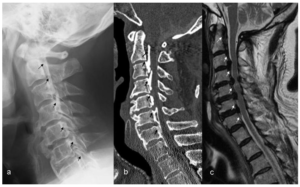
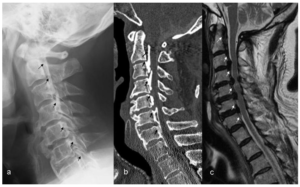
Figure 3. OPLL Diagnosis using Three Modalities: 73-Year-Old Male.
a. Lateral radiograph: Multiple ossifications are visualized along the vertebral bodies at the level of C2, C3, C4, C5, C6 and C7 (arrows). Bridging spur formations are visualized at the level of C4/5 and C5/6. Ossification of anterior longitudinal ligament is seen between C6 and C7.
b. MPR sagittal image of cervical spine CT after myelography: The longitudinal ligament shows severe ossification and thickening (arrows). Cervical canal is narrow due to the OPLL.
c. T2 weighted sagittal MR image: The longitudinal ligament thickening is demonstrated from C2 to C7 (arrow). Spotty high signal intensity area suggestive of myelomalacia is present at the level of C4/5.
| Table1: Distribution of OPLL. |
|
Level
|
CT n=60 |
X-ray n=60 (%) |
MRI n=60 (%)
|
|
C2
|
18 |
16 |
88.8 |
18 |
100
|
|
C3
|
36 |
32 |
88.8 |
36 |
100
|
|
C4
|
49 |
39 |
79.5 |
48 |
97.9
|
|
C5
|
47 |
45 |
95.5 |
52 |
110.6
|
|
C6
|
47 |
20 |
42.5 |
33 |
70.2 |
| C7 |
21 |
3 |
23.8 |
14 |
66.6
|
| The OPLL which was diagnosed by CT is based on the comparison of both X-rays and MRI. The OPLL was relatively prominent at level of C4, C5, C6 on CT. Both X-rays and MRI presented good accuracy of cervical OPLL at level of C2, C3 and C4. About C5, X-rays yielded good accuracy (95.5%), but MRI was prone to overestimation (110.6%). Accuracy of OPLL at level of C6 and C7 decreased in MRI and X-rays. The decrease in accuracy was more pronounced in X-rays. |
DISCUSSION
Cervical OPLL was first reported in Japanese population in 1960 by Tsukimoto.3 In 1964, Terayama4 defined the cervical OPLL as a clinical entity on the basis of histological findings. Recording cervical X-rays is the first step in the diagnosis of cervical OPLL. In the lateral radiograph, ossification appears as a continuous or segmental bony density projecting into the central spinal canal. However, severe spondylosis and hypertrophy associated with facet joints and pedicles hinder the detection of OPLL in the lateral radiograph. In addition, the appearance of OPLL-like dots within 3 mm thickness is difficult to detect on the lateral radiograph.5 Therefore, these X-rays’ findings would appear few if compared to the findings in CT. Conversely, there are difficulties in distinguishing ossifications from ligament hypertrophy via MRI.6 In MRI, OPLL presents two different types of patterns: The first displays a thick posterior longitudinal ligament with diffuse low signal intensity in both T1 weighted and T2 weighted images. The second pattern illustrates a thick posterior longitudinal ligament with mixed high and low signal intensity in both T1 weighted and T2 weighted images suggestive of bone marrow component. If the bone marrow component is included with the thick posterior longitudinal ligament, that area is absolutely consistent with OPLL. However, if a thick posterior longitudinal ligament with low signal intensity is only present in the MRI report, it would be difficult to diagnose the condition correctly. The diagnosis would then require the confirmation of ossification via CT.5 These MRI findings would identify a larger patient pool with OPLL in comparison to CT imaging.
Detection of OPLL on each vertebral body varied between X-rays and MRI. Both X-rays and MRI presented respectable accuracy of cervical OPLL at the level of C2, C3 and C4. As for C5, X-rays yielded good accuracy (95.5%), but MRI was prone to overestimation (110.6%). Okada et al7 reported that the presence of cervical disc degenerative changes was higher in patients with disc extrusion/hernia. Cervical disc hernia at C4/5, C5/6 and C6/7 is particularly more common than the ones at any other level. Accordingly, the overestimation of MRI at C5 could be caused by cervical disc herniation.
In addition, at C6 and C7, low accuracy was observed with MRI and X-rays. Lower levels of cervical spine such as C5, C6 and C7 present a lot of motion and would be associated with more severe osteoarthritis than the upper level of cervical spine.8 It interferes with the accuracy of X-rays. Regarding cervical OPLL treatment, cervical laminoplasty has become the standard technique for patients with myelopathy. Hori et al9 reported that young patients with continuous or mixed-type OPLL and C3 ossification had a risk of progression in OPLL thickness following surgery. From our study, detection of OPLL at level of C3 was note worthy. Therefore, a follow-up study would be possible in all modalities.
CONCLUSION
Cervical OPLL tends to be diagnosed with only plain X-rays or MRI. Diagnosing cervical OPLL using lateral radiograph is prone to underestimation, and diagnosing it using MRI is prone to overestimation. If severe spondylosis, facet joints and pedicle shadows occur, they would hinder the detection of OPLL in the lateral radiograph. Regarding the diagnosis via MRI, it would be difficult to distinguish ossifications from ligament hypertrophy. In addition, in the lower level of cervical spine (C6 and C7), low accuracy is observed with both X-rays and MRI. However, the use of X-rays and MRI presents a powerful tool in the diagnosis of cervical OPLL at C2, C3, and C4 levels.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.