INTRODUCTION
Neurodevelopmental disorders (NDDs) are a group of conditions that a child may be born with or develop during childhood1 are characterized by impairments in cognition, communication, behavior, and/or skills resulting from abnormal brain development.2 This group of conditions may cause disability during the life of the child.3 Social, academic, and occupational functions are some of the aspects that may be affected in their lives.1 Also, children affected by NDD may experience delays or deficits in achieving developmental milestones.1 According to international classification of diseases-11 (ICD-11), NDD are disorders of intellectual development, developmental speech or language disorders, attention deficit, and hyperactive disorder, stereotyped movement disorders, motor coordination disorders, developmental learning disorders, autism and other NDDs.4
NDDs can have similar symptoms5 or overlap in common symptoms of most co-occurrence which are related to cerebral dysfunction and cognitive problems. Also, poor motor abilities can be present in children with NDD affecting academic achievement.6 Furthermore, many of these children can present aggressive behaviors and sensory processing problems.7,8 Prevalence of NDDs’ in males twice the prevalence in females.9 The two most prevalent NDDs’ in the United States are autism spectrum disorder (ASD) and attention deficit and hyperactivity disorder (ADHD).10
The NDDs’ can co-ccur11 as well as, these children can suffer from other comorbidities.12 Other mental and physical diseases can be present, along with NDD. Furthermore, studies found a higher prevalence of psychiatric disorders in the family history of diseases of children with autism. A study concluded that the psychiatric disorders in parents of children with autism were higher compared to the parents of children without autism.13 Another study found that bipolar disorder in both parents increased the risk in the offspring.14 Also, another study in Denmark concluded that the history of any psychiatric disorder increased the risk of autism and suggested that the cause is a genetic link between schizophrenia and autism.15
Furthermore, in the United States in 1999, researchers found that children were twice more at risk of developing ASD in families where two or more family members had an auto-immune disease,16 this finding was confirmed by Hughes et al.17 The families with three or more members were 5.5 more likely, and the children whose mother suffered from an auto-immune illness were 8.8 more likely at risk of developing ASD. Asthma and allergies are two auto-immune diseases strongly associated18 with ASD. However, a meta-analysis was conducted to evaluate the association between suffering from asthma and autism. The study assessed the odds ratio (OR) from ten studies. However, although asthma may have a high prevalence in children with autism, no association was found.19
This study had the purpose of developing an epidemiological profile of children with NDD in southern Puerto Rico. Also, this study sought to identify the clinical characteristics and family history of disease in close relation to the individuals. Furthermore, to evaluate the association between comorbidities reported and family history of diseases reported with the NDD.
MATERIALS AND METHODS
This study is an exploratory study with a cross-sectional design carried out in a diagnostic center located in Ponce, Puerto Rico. Univariate analysis was performed to describe the sample under study. Bivariate and multivariate analyses were performed to determine associations between comorbidities, family history of conditions, and NDDs’. The study was approved by Ponce Health Sciences University Institutional Review Board (IRB).
Sample
The population under study was obtained from a secondary database created previously to the study in a diagnostic center in southern, Puerto Rico. The population sample sought was for children up to 18-years-old of both sexes with a NDD using either the diagnostic and statistical manual of mental disorders-4 (DSM-4) or DSM-5 published diagnostic criteria. All children in the database were considered for inclusion in the sample. Two hundred fifty-seven (257) children were ultimately deemed appropriate for analysis.
Data Collection
A secondary database created independently and prior to the study was explored for the analysis. This database was created using a single, unified data collection instrument based on several tools title “initial interview.” In the approach designed, a social worker interviews the child’s caregiver as a first approach using this questionnaire in the diagnostic center under study. The interview collects data about socio-demographic information, clinical history, and family history of diseases. Furthermore, a hand-writing record review was performed to obtain data related to the principal diagnosis of the children and comorbidities reported. The “Interdisciplinary Diagnostic Certification of the ASD” on the records was used to obtain the final diagnosis, comorbidities, and possible observations based on the DSM-4 for the cases evaluated before 2013 and DSM-5 for the cases evaluated after 2013. Also, the case report form document was used to collect and confirm sociodemographic variables of interest. Chart review provided an official principal diagnosis of any children included in the study.
Statistical Analysis
The statistical program used to perform the quantitative analysis was statistical package for the social sciences (SPSS) version 26. Forty-eight (48) cases were excluded out of two hundred fifty-seven subjects in the database. One child was excluded from the sample because it was a repeated case, and forty-seven were excluded due to missing information. Missing values were taken into consideration to perform the analysis. A Kolmogorov-Smirnoff test was performed to determine if the sample had a normal distribution because small samples in a study sometimes did not have a normal distribution.20 In the database, each condition reported appeared classified into categories. The categories available were developmental problems, neurological disorders, chronic diseases, mental diseases, and mental retardation. The variables were re-categorized because all the diseases appeared as an open fill. Each condition reported in the family was created as a dichotomous variable (Yes/No) to perform the bivariate and multivariate analysis.
Fisher’s exact test evaluated the associations between each NDD and each comorbidity reported, such as ASD, ADHD, mental disorder, and the association between each NDD and each disease reported in the family history of diseases. A multivariate analysis was performed through logistic regression to evaluate the odds of presenting each comorbidity among children with ASD as compared with other NDDs’ adjusted by age and sex. Children with autism were used as a reference group for the bivariate and multivariate analysis.
RESULTS
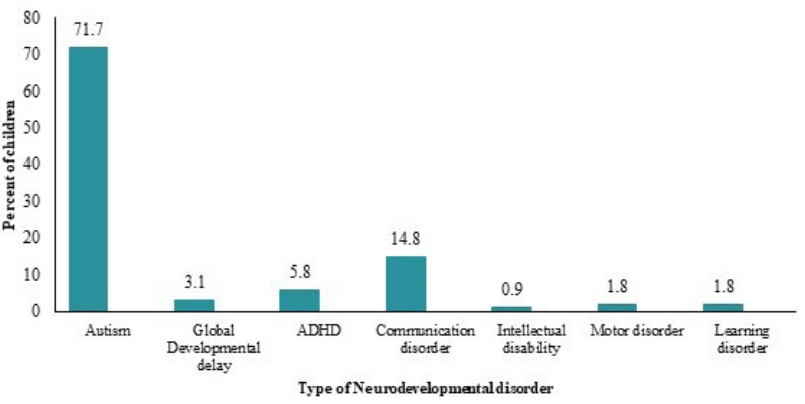
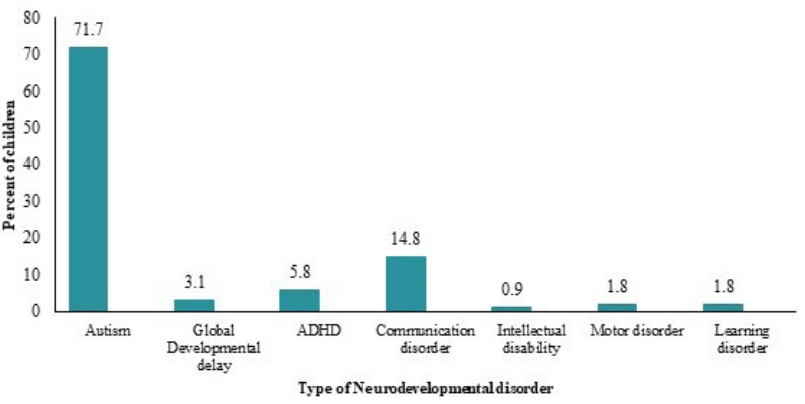
The mean age and standard deviation of the sample were 5.2±3.20, and 80.5% were males. Most of the children lived in Ponce, Puerto Rico. The normality test (Kolmogorov-Smirnov) performed revealed a statistical significance of 0.000, indicating that the sample does not have a normal distribution. Furthermore, 88.2% of the children received a previous evaluation related to the problem, and 70.5% received some treatment for the symptoms before coming to the diagnostic center. The most-reported previous diagnostic evaluations were speech and language, psychological and pccupational. The most-reported previous treatments were therapies, psychological treatment, and prescription drugs. The frequency of children by NDD diagnosis were calculated considering the missing values. There was no identified primary diagnosis for thirty-four children. 71.7% (n=160) autism spectrum disorder and 14.8% (n=33) were primarily diagnosed with communication disorder. These disorders represented 87% of all disorders identified. Other disorders diagnosed in the center were ADHD (5.8% (n=13)), global developmental delay (3.1% (n=7)), motor disorder (1.8 (n=4)), earning disorder (1.8% (n=4)) and ntellectual disability (0.9% (n=2)) (Figure 1).
Figure 1. Types of Neurodevelopmental Disorders Diagnosed20
Regarding the comorbidities, the two more reported were sensory problems (24.9%) and mental problems (24.9%). The two less reported comorbidities were cardiovascular diseases (0.5%) and vision problems (0.5%) (Table 1).
| Table 1. Comorbidities Report20 |
| Comorbidity Diagnosed |
n |
Percentage (%) |
| Sensory problems |
52 |
24.9 |
| Mental disorders |
52 |
24.9 |
| Feeding problems |
6 |
2.9 |
| Gastrointestinal problems |
6 |
2.9 |
| Metabolism disorder |
5 |
2.4 |
| Sleeping problems |
5 |
2.4 |
| Asthma |
5 |
2.4 |
| Allergies |
5 |
2.4 |
| Problems in diary skills |
4 |
1.9 |
| Audition problems |
2 |
1.0 |
| Neurologic disorders |
2 |
1.0 |
| Dysphagia |
2 |
1.0 |
| Cardiovascular diseases |
1 |
0.5 |
| Vision problems |
1 |
0.5 |
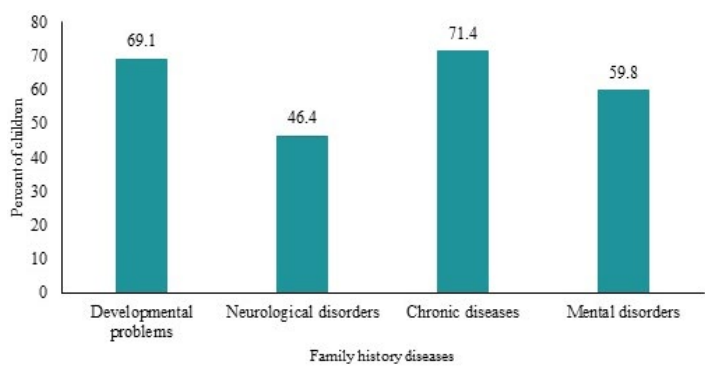
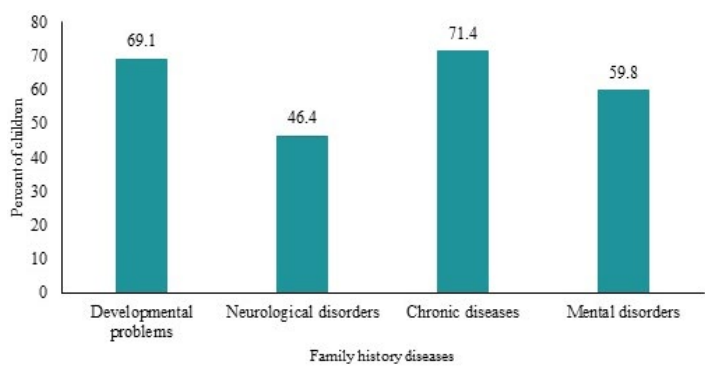
The most-reported diseases in family history were developmental problems (n=160) and chronic conditions (n=161) (Figure 2).
Figure 2. Family History of Conditions Reported by Caregivers during the “Initial Interview”20
The comorbidities and diseases most reported for each NDD and also reported in family history were given consideration. In children with autism, other NDD’s were reported. Also, mental disorders and sleep problems were present in this sample of children. A statistically significant association was found between autism and communication disorder (OR=6.9; IC 95%. 3.2, 15). Also, the analysis revealed that there exists a statistically significant association between autism and motor disorder (OR=2.18; IC 95% 987, 4.8). Furthermore, there exists an association between mental disorders and autism (OR=0.71; 0.079-0.373) (Table 2).
| Table 2. Association between Autism Spectrum Disorder and Comorbidities Reported20 |
|
Comorbidities
Reported
|
Autism
n (%) |
Other NDDs’
n (%) |
Unadjusted OR (CI) |
Adjust
OR (CI) |
p Value |
| ADHD |
| Yes |
36(25.2%) |
10(15.2%) |
1.8 [0.871-4.07] |
1.0 [0.460-2.4] |
0.888 |
| No |
107(74.8%) |
56(84.8%) |
|
|
| Communication Disorder |
| Yes |
103(72.0%) |
16(13.4%) |
8.0 [4.1-15.7] |
6.9 [3.2-15] |
0.000 |
| No |
40(28.0%) |
50(75.8%) |
|
|
| Motor Disorder |
| Yes |
52(36.4%) |
13(19.7%) |
2.3 [1.16-4.6] |
2.1 [0.987-4.8] |
0.05 |
| No |
91(63.6%) |
53(80.3%) |
|
|
| Learning Disorder |
| Yes |
17(11.9%) |
8(12.1%) |
0.97 [0.399-2.39] |
0.467 [0.151-1.4] |
0.185 |
| No |
126(88.1%) |
58(87.9) |
|
|
| Sensory Problems |
| Yes |
38(26.6%) |
14(21.2%) |
1.3 [0.669-2.6] |
1.0 [0.487-2.4] |
0.835 |
| No |
105(73.4%) |
52(78.8%) |
|
|
| Mental Disorder |
| Yes |
22(15.4 %) |
30(45.5%) |
0.21 [112-.0424] |
0.17 [0.079-0.373] |
0.00 |
| No |
121(84.6%) |
36(54.5%) |
|
|
| NDD’s: Neurodevelopmental disorders; CI: Confidence intervals; Adjusted by age and sex by each comorbidity reported |
In children with ADHD, a communication disorder were reported. Another comorbidity reported was mental disorders. Furthermore, a statistically significant (p-value=0.002) association between ADHD and mental problems (OR=0.028; IC 95% 0.003, 0.27) was found (Table 3).
| Table 3. Association between Children with Attention Deficit Disorder and Other20 |
| Comorbidities Reported |
Autism
n (%) |
Other NDDs’
n (%) |
Unadjusted OR (CI) |
Adjust
OR (CI) |
p Value |
| Communication Disorder |
| Yes |
103(72.0%) |
6(46.2%) |
3.0 [0.95-9.4] |
0.61 [0.09-3.9] |
0.609 |
| No |
40(28 .0%) |
7(53.8%) |
|
|
| Mental Disorder |
| Yes |
22(15.4%) |
11(84.6%) |
0.03 [0.007-0.15] |
0.03 [0.03-0.27] |
0.002 |
| No |
121(84.6%) |
2(15.4%) |
|
|
| DHD, Attention Deficit and Hyperactivity Disorder; CI, Confidence Intervals; Adjusted by age and sex by each comorbidity reported |
In children with a communication disorder (CD), motor disorders were reported (21.2%). Other comorbidities, mostly reported in children with CD were sensory problems and mental disorders. Besides, communication disorders and mental disorders (OR=0.35; IC 95% 12, 0.98) are associated (Table 4).
| Table 4. Association between Children with a Communication Disorder and Other20 |
|
Comorbidities
Reported
|
Autism
n (%) |
Other NDDs’
n (%) |
Unadjusted OR (CI) |
Adjust
OR (CI) |
p Value |
| Motor Disorder |
| Yes |
52(36.4%) |
7(21.2%) |
2.1 [0.86-5.2] |
2.7 [0.91-8.1] |
0.072 |
| No |
91(63.6%) |
26(78.8%) |
|
|
| Sensory Problems |
| Yes |
38(26.6%) |
8(24.2%) |
1.1 [0.47-2.7] |
0.80 [0.27-2.3] |
0.700 |
| No |
105(73.4%) |
25(75.8%) |
|
|
| Mental Disorder |
| Yes |
22(15.4%) |
12(36.4%) |
0.31 [0.137-0.739] |
0.35 [0.12-0.98] |
0.046 |
| No |
121(84.6%) |
21(63.6%) |
|
|
| CD: Communication disorder; CI: Confidence Intervals, Adjusted ORs’ were adjusted by age and sex by each comorbidity reported |
Regarding the family history of diseases, in children with Autism, a family history of NDD’s was reported. The NDD’s reported in family history was autism, speech and language disorders (LDs’), learning disorder (LDs’), and ADHD. Also, other chronic diseases were present in the family history.
DISCUSSION
The results in our sample revealed that most of the children who came for diagnosis and treatment to the diagnostic center were males. That coincided with Boyle et al9 research, where they conclude NDD male prevalence as twice female prevalence. Most of the children lived in Ponce, but the town of residence of many children was unknown. The majority of the children were older than three-years-old, and the mean age was 5.2±3.20-years. That coincides with Arora et al21 study, where they conclude that the higher prevalence of children with NDD in India was between 6-9-years-old. However, APA1 established that frequently the first symptoms onset in early development often before starting school. There were no differences between the mean ages by sex.
In the sample studied, 88.2% had already received a previous evaluation related to concerns expressed by the parents. The most-reported previous diagnostic assessments were speech and language, psychological and occupational. Also, 70.5% reported received in the past some formal treatment for the symptoms. The most-reported previous treatments were therapies, psychological treatment, and prescription drugs. This means that most children have a previous finding or concern evaluated by the parents before reaching a final diagnosis of a neurodevelopmental condition. In the United States, ASD and ADHD are the most common NDD diagnosed.10
ASD was the most diagnosed followed by CD and ADHD. NDDs can co-occur with each other.1,11 Our findings show the co-occurrence between them. In children with autism, communication disorders and motor disorders were reported. Our results confirmed that because CD was reported in children with ADHD.
The children with ASD have 6.9 times more possibilities of reporting CD and 2.18 times more possibilities of reporting motor disorder (MD) than children with other NDDs. Furthermore, results revealed that children with ASD have 0.112 times fewer chances of reporting ADHD than children with global developmental delay (GDD). Other comorbidities reported in the sample were sensory processing problems, sleep problems, and mental disorders.
Holland8 and Blackmer et al22 coincide with our findings that children with a NDD can present sleep problems. In this study, sleep disorders/problems were reported in children with autism and communication disorders. Also, in children with autism, asthma and allergies were reported. Nevertheless, no association was found. These findings coincide with the meta-analysis carried out in 2016 in which they found no association between the two conditions and ASD.18 It must be taken into consideration that were a few reports of these comorbidities in our sample.
In addition, mental disorders are associated with ASD, ADHD Communication disorder, and Learning disorder. Children with autism have 83% fewer possibilities of reporting a mental disorder than children with other NDDs. Besides, children with autism have 98% fewer chances of reporting a mental disorder than children with ADHD and 65% fewer possibilities of reporting a mental disorder than children with a communication disorder. Furthermore, children with autism have 93% fewer possibilities for reporting a mental disorder than children with a learning disorder.
Also, some diseases in family history can increase the possibility of reporting NDD. According to Comi et al16 exists an association between family history of asthma, allergies, and autism. A family history of asthma was reported in children with autism and communication disorder, but no association was found. Other studies found an association between mental disorders and autism.10,12,13,14 These studies found the mental disorders increase the risk of autism. In this study, the analysis found the opposite.
A family history of mental disorders is associated with autism but as a protective factor. Children with autism have 51% fewer possibilities of reporting a family history of mental disorders than children with other NDDs. Besides, children with autism have 3.76 more chances of reporting a family history of diabetes than children with CD. Regarding qualitative analysis, the caregivers expressed their concerns regarding the symptoms and signs presented in the children.
CONCLUSION
In this study, most of the children were in early childhood when they came for diagnosis and treatment. Furthermore, males were the most diagnosed with NDDs. The most diagnosed disorder was autism. NDDs co-occurred. Also, other comorbidities co-occurred with these disorders. Family history of developmental problems and chronic diseases were leading conditions reported by caregivers. The caregivers stated that onset symptoms were the cause of worry; some of the symptoms include developmental milestones delay, communication, and social interaction deficits, aggressive behavior, and deficits in intellectual functions.
STRENGTHS AND LIMITATIONS
This study is the first study carried out in a diagnostic center in the south of Puerto Rico to evaluate NDDs. This study is an exploratory study that can serve as a base study for other epidemiological studies. However, this study has several limitations. The first limitation is the selection of the sample was by a no-probabilistic method. For that reason, our findings and conclusions cannot be extrapolated to the general population. The second limitation identified was the incomplete information for some of the variables under study. The third limitation identified was the information obtained from the secondary database was based on self-reports. And the fourth limitation was the instrument utilized to get the information for the secondary database was not designed for research purposes (mostly qualitative).
PUBLIC HEALTH RELEVANCE
This study is critical because it helps to understand the clinical characteristics, concerns, and needs of children with NDD and their caregivers. This study is a basis for further studies related to these disorders. More studies are required to support the development of better intervention programs for these children and their families.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
CONSENT FOR PUBLICATION
All authors have read and approved the final article. All consent to the publication of this article.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
ACKNOWLEDGMENTS
Research reported in this publication was supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under award number 5U54GM133807 and the Research Centers for Minority Institutions (RCMI-U54MD007579). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health). Special thanks to Dr. Ismarie Soto-Infante and Dr. Suilariam Cepeda for their support in data collection and Dr. Melissa Marzan for her support for the qualitative analysis.
FUNDING
Ponce Health Sciences University, Public Health program (SEED Money).
AUTHOR CONTRIBUTIONS
Accountability
Laura Deliz Bauzá and Luisa Morales had full access to all of the data in the study and assume responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and Study Design
María Pacheco, Iris Martínez and Luisa Morales.
Acquisition of Data
María Pacheco.
Analysis and Interpretation of Data
María Pacheco, Iris Martínez and Luisa Morales.
Drafting of the Manuscript
María Pacheco, Laura Deliz.
Critical Revision of the Manuscript for Important Intellectual
Content
Laura Deliz, Luisa Morales.
Statistical Analysis
María Pacheco, Iris Martínez and Luisa Morales.
Acquisition of Funding
Luisa Morales.
Study Supervision
Laura Deliz and Luisa Morales.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.