BACKGROUND
Cholera is an intestinal infection caused by a bacteria Vibrio cholerae. It remains a global health problem with several hundreds of thousands of reported cases each year. Despite all the major advances in research, the condition still remains a challenge to the modern medical world.
The disease is often contracted from drinking unclean water. Each year, 1.3 million to 4 million people around the world suffer from cholera and 21,000 to 143,000 people die of the disease, the incidence is estimated to be greatest in children less than 5-years of age according to the World Health Organization (WHO).
Cholera is a high-risk in sub-Saharan Africa where clean water and sanitation are often lacking. The disease crops up in other parts of the world when conflict or natural disasters damage water systems and displace families. Though there has been a decrease in the endemicity and intensity of epidemics across the continent, the case fatality rates remain higher in Africa than elsewhere. Some of the risk factors that contribute to these outbreaks include; water contamination, heavy rainfall and flooding and population displacement. It has also been associated with poverty and closely linked to inadequate drinking water and poor sanitation.
In Dadaab Refugee Camp, a cholera outbreak has been common trend annually over the last seven years with the highest caseload reported between November 2015 and March 2016 outbreak, with around 1234 suspected cholera cases and 5 deaths.
On 27th March 2019, The International Rescue Committee (IRC) (health implementing partner) in Dadaab Refugee Camp reported an outbreak of acute watery diarrhea. A 15-years-old had reported to the IRC main hospital with acute onset on watery diarrhea and vomiting, two days later on 29th March, two children aged 5 and 4-years respectively, reported with similar presentation and were admitted at the Cholera Treatment Centre (CTC). Preliminary assessment by the health team and Sub County Surveillance officer showed that these case-patients developed these symptoms a few hours after eating food. The report also highlighted that there were 8 suspected acute watery diarrhea (AWD) developed symptoms after having attended a wedding in the same community initial testing with cholera rapid diagnostic test showed the samples were positive. We conducted this investigation to confirm the causative organism and describe the epidemiology of the outbreak in order to support evidence-based control measures.
METHODS
Study Site
The outbreak occurred in Hagadera Refugee Camp and the surrounding host community within Fafi Sub County, Garissa County in Kenya. Dadaab Refugee Camp is located in the Northeastern part of Kenya in Garissa County, about 500 kilometres from Nairobi Kenya’s Capital and 90 kilometres from the Kenya-Somalia border.
Dadaab is a complex with three Refugee Camps that have a combined population of 208,7331 refugees. Hagadera Refugee Camp is one of the complex with a population of 117,000 of whom 4860 (4%) are children <1-year. (Figure 1) whereas the surrounding Fafi Sub County comprising of a population of approximately 11,700. The two regions reported 585 and 82 cases for Hagadera and the surrounding host community respectively. The population is nomadic and the main economic activity in the area is pastoralism.
Figure 1. Hagadera Camp Snapshot

Case Definition
A suspected case was a resident of Hagadera Refugee Camp or its surrounding environs with sudden onset of acute watery diarrhea and vomiting between March and September 2019. A probable case was a suspected case with a positive rapid test for V. cholerae; a confirmed case was a probable case with a positive stool culture for V. cholerae. In an event of demise of a suspected, probable or confirmed cholera case – this was termed as cholera death.
Case Finding
A systemic case finding was carried out by paying a visit to the health facilities and households affected within the camp. During the outbreak period (27th March-15th September, 2019), the team reviewed the patients’ records to identify suspected cases of cholera among the patients. Thereafter, verification was done by visiting infected households and health facilities. A checklist was administered to obtain demographic and epidemiological information for analysis and those fitting the criteria were referred to CTC for further care and management. The community health workers were instrumental in the referral of cases from the households to the health facility.
Descriptive Epidemiologic Analysis
To examine how the cases were distributed, a descriptive epidemiological study was conducted, the development of an epidemic over the period of time was represented by the use of an epidemic curve. The finding and the data from the analysis were used to compute the attack rate for both age and sex. The case fatality rate was calculated using the prescribed formula as a ratio of the total number of suspected cholera death to the total number of case patient.
Laboratory Analysis
In the health facility, stool specimens were collected before patients received antimicrobial treatment and tested using Onsite rapid diagnostic test kit. The results were read at 10 min and interpreted following the manufacturer’s recommendation. The test was considered positive if the control line and either T2(O1) or T1 (O139) or both (O1 and O139) appeared; negative if the control line only appeared and invalid if the control line did not appear. The reported sensitivity for onsite rapid diagnostic kit (RDT) under field conditions was 96.7 and specificity was 94. All stool specimens meeting criteria proceed to laboratory for bacteriological culture analysis.
Stool Culture and Bacterial Identification
Stool specimens were inoculated in alkaline peptone water, incubated at 35-37 °C for 4 h, plated on thiosulfate citrate bile salts sucrose (TCBS) agar plates and incubated overnight at 35-37 °C. Culture plates were visually examined for medium-sized convex, smooth, yellow colonies and sub-cultured on nutrient agar plates overnight at 35-37 °C. Colonies from the nutrient agar were screened using oxidase discs (Becton, Dickinson and company, USA) and oxidase positive isolates serotyped using polyvalent O1 specific antiserum (Becton, Dickinson and company, USA) and monovalent Inaba and Ogawa antisera (Becton, Dickinson and company, USA).
Case Management
Cholera treatment center were set up to support in the isolation and management of cholera case-patients. Upon confirmation of a cholera case, the patient was referred to the cholera treatment unit for further management including oral and intravenous rehydration.
RESULTS
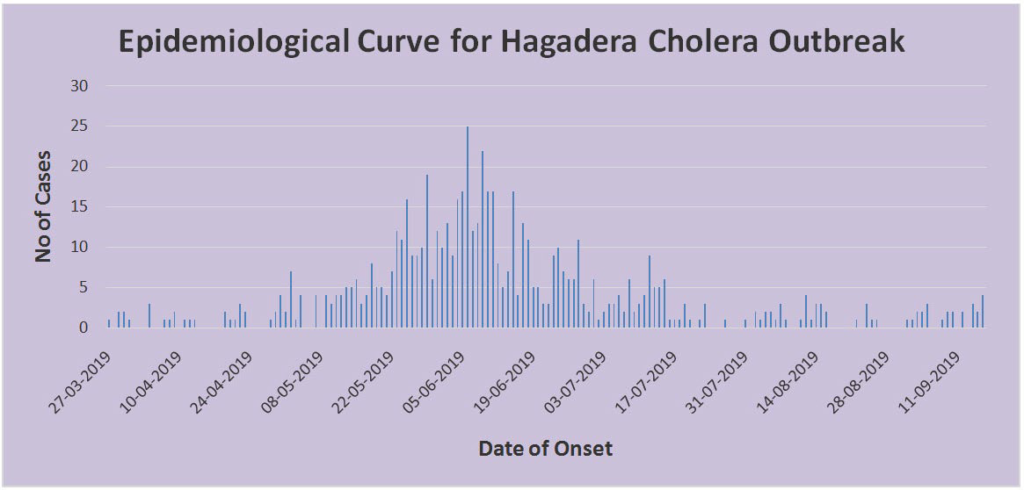
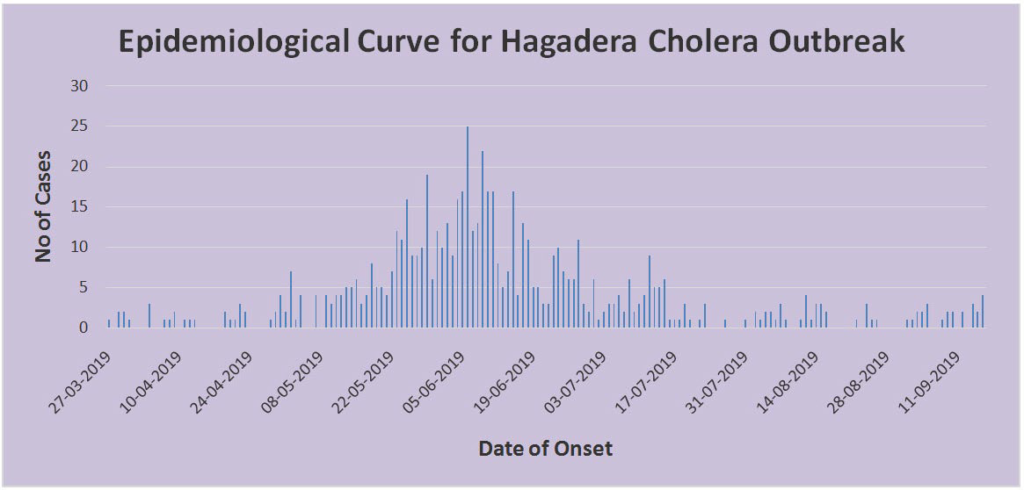
During the outbreak that occurred in Hagadera Refugee Camp and the surrounding host community between March and September 2019, 40% (264/667) of the suspected cholera cases had stool samples collected and tested using RDTs. Of those tested at the different treatment centers, 84% (221/264) were positive with RDT. Out of the 264 stool samples taken to the Laboratory, 30% (78/264) were confirmed to be V. cholerae O1 serotype Inaba. The representation in the epidemic curve displayed that the outbreak was from a common source with several peaks and waves (Table 1).
| Table 1. Demographical Breakdown of the Cholera Cases |
|
Age
|
0-5
|
6-10 |
11-15 |
16-20 |
21-25 |
26-30 |
31-35 |
>35
|
|
Gender
|
M |
F |
M |
F |
M |
F |
M |
F |
M |
F |
M |
F |
M |
F |
M |
F |
| 153 |
136 |
33 |
35 |
25 |
25 |
26 |
32 |
17 |
19 |
26 |
25 |
11 |
12 |
35 |
35
|
|
CFR
|
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0
|
The index case that was admitted on March 27, 2019, showed symptoms of cholera after attending a wedding celebration from block K9 in Hagadera Refugee Camp. The time lag between the index case and notification was due to surveillance challenges. The highest number of cases had onset on 28th May, 2019 in epidemiological week 22, the first case from the surround ing host community was reported in epidemiological week 19. The case fatality rate (CFR) was 0.0% (0/667). The mean age of the case-patients was 15-years (Range: 0.2-75 years) (Figure 2).
Figure 2. Epidemiological Curve for Cholera Outbreak in Hagadera
DISCUSSION
Our investigation findings uncovered a continuous common source outbreak of V. cholerae 01 serotype Inaba occurred in Hagadera Refugee Camp and surrounding host community, in Garissa County of Kenya with a CFR of 0.0%. The highest attack rate was in age≥30 years; there was no difference in gender.
V. cholerae O1, serotype Inaba has been associated with outbreaks of high morbidity and mortality. Epidemics occur mostly in crises situation where water and food supplies become contaminated with V. cholerae in areas with crowded living conditions and poor sanitation. Its ability to cause death within hours of onset especially in undeveloped countries has become a major public health challenge. It is therefore important that awareness about cholera outbreaks is created to stimulate better understanding of the disease and lead to development of practical preventive and therapeutic measures. Death of cholera case-patients usually results from profuse secretory diarrhea which leads to severe dehydration, metabolic acidosis, electrolyte imbalance and circulatory collapse.
The continuous common source outbreak that occurred in Hagadera, between March and September 2019 was attributed by several factors; poor sanitation and inadequate water supply, congestion and overcrowding, inadequate availability of pit latrines and limited knowledge by camp residents on hygiene, whereas for the surrounding host community, inadequate water supply, inadequate surveillance system and insecurity that hampered the movement of the response team in controlling the outbreak topped the list of contributing factors. The incapacity of the team to efficaciously single out the source of the outbreak prolonged the exposure beyond one incubation period. Several studies have demonstrated that cholera outbreaks can persist in the community if not adequately investigated.1,2
The CFR has been known to be a measure of the adequacy of the health care system in cholera outbreak response.3 The health team in Hagadera and larger Garissa County managed to maintain the CFR at 0.0% a figure that is well below t the recommended WHO standard of ≤1%. Such low CFR suggests adequate preparedness, surveillance, case management, community targeted health promotion.4 In the year 2010, a cholera outbreak response in northern Nigeria, recorded a higher CFR (3.75%) which was quite higher compared to our study. Another study done in South Sudan showed a CFR as high as 11% in some counties.5
Our study found the highest attack rate to be among age≥30 years, with no significant difference in gender. This could have been due to the fact that this age group was involved in the care and transportation of the cholera case-patients from the villages to the CTCs with subsequent contamination. This contrasts a study done in Kasese District, Western Uganda which showed the highest attack rate among 5-14 years at 4.2%, though there was also no difference in gender. The WHO position paper highlights that young children living in endemic areas are the most affected by the disease but any age group may suffer.6
Oral cholera vaccines (OCVs) have been recommended in cholera-endemic settings and pre-emptively during outbreaks and complex emergencies.7
This study reveals the challenges and gaps experienced in countries with insecurity regarding, prevention, early detection and effective response to public health threats. However, it also has limitations: Owing to surveillance challenges and insecurity in the area, several cases could have been missed at the beginning of the outbreak, which limits the reliability of our descriptive epidemiology. Also, due to nomadic nature of the pastoralist community surrounding the Hagadera Refugee Camp, there were population movements from one area to another affecting the insurgency to mobile areas within the Refugee Camp.
CONCLUSION
This was a continuous common source cholera outbreak caused by V. cholerae serotype Inaba. We recommended strengthening of surveillance system to improve detection and response.
ACKNOWLEDGEMENTS
We thank the Fafi Sub County and Garissa County Ministries of Health for the good work relationship exhibited during this outbreak investigation. We also wish to express our sincere gratitude to IRC and United Nations High Commissioner for Refugees (UNHCR) who are the implementing partners in the Refugee Camp for the support they gave.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated and/or analyzed during the current study are not publicly available due to ethical issues but are available from the IRC Kenya Program upon reasonable request or from the Director of Preventive and Promotive Health, Ministry of Health, Garissa County, Kenya.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
Verbal informed consent was obtained from the cholera casepatients involved in the study or, caretakers (if the interviewee/ patient was a minor) before the start of the interview. We sought verbal consent because this study was conducted as part of an outbreak investigation whose primary purpose was to inform disease control efforts rather than outright human subjects’ research. Non-etheless, the purpose of the investigation was explained to the patients. Also patients were informed that their involvement was entirely voluntary and their refusal to respond to any or all of the questions would not result into any penalty. Participants’ confidentiality involving personal information were de-identified during data analysis.
CONTRIBUTIONS
KN designed study, analyzed, interpreted data, and drafted the initial manuscript. KN reviewed the initial manuscript for intellectual content. WK, SM conducted a laboratory examination of the samples and wrote the laboratory analysis section. All coauthors read and approved the final manuscript.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.