CASE REPORT
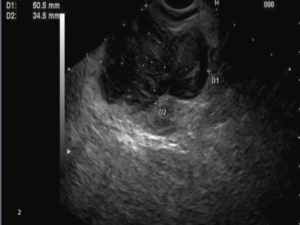
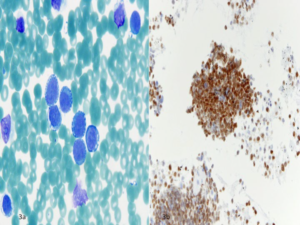
A 27-year-old male with no significant past medical history, presented to the emergency room with symptoms of perianal pain. Additionally, the patient complained of cramps in his legs and buttocks for approximately one month. The cramps were initially minor but progressively worsened and then became constant. His vitals and physical examination were normal except for his digital rectal examination, which was painful and tender. However, no obvious mass was felt in the rectum. His initial blood tests were unremarkable which included hemoglobin-14 g/dl (Nv-13.5-16.5), white cell count-8.9 (Nv-4.5-11), platelets-324 (Nv-150- 400), blood urea nitrogen-12 (Nv-7-25), creatinine 1.2 (Nv-0.4-1.24), sodium-140 (Nv-137- 145) and potassium of 3.7 (Nv-3.5-5.1). Pelvic Computed Tomography (CT) (Figure 1) showed a mass in the perianal region measuring 12 cm with metastasis to the left iliac and obturator lymph nodes. In view of the CT findings, other lab tests like Carcinoembryonic antigen (CEA)- 0.5 (Nv-<3 ng/ml), CA 19-9-10 (Nv-<35 u/ml), Human Immunodeficiency Virus (HIV), Human papillomavirus (HPV) and Chlamydia were checked and were all within normal range. The patient then underwent lower EUS, which showed a 5 cm hypoechoic mass (Figure 2) just outside the anal canal. An FNA was obtained which showed neoplastic cells (Figure 3A). Then cells were largely mononuclear, with a few binucleate and multinucleate cells. These cells had a high nuclear cytoplasmic ratio with a relatively round nucleus. Immunohistochemical stain was positive for muscle (desmin) and more precisely for striated muscle (myogenin, Figure 3B), supporting the diagnosis of Rhabdomyosarcoma. Subsequent Fluorescent in situ hybridization (FISH) performed using DNA probe specific for the FOXO1 (FKHR) gene on 13q14 showed a signal pattern suggestive of rearrangement of FOXO1 gene. Rearrangement of FOXO1 is
associated with a diagnosis of Alveolar Rhabdomyosarcoma. Unfortunately, the patient was a poor candidate for curative treatment due to the presence of distal metastasis. However, he underwent adjuvant chemotherapy and radiation therapy for treatment of his cancer.
Figure 1: Mass in the perianal region.

Figure 2: Hypoechoic perianal mass as seen in lower EUS.
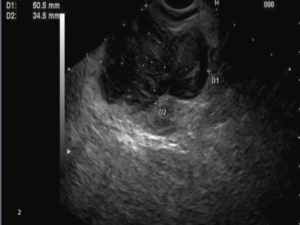
Figures 3: Malignant mononuclear cells with high nuclear cytoplasmic ratios and fairly round nuclei (100X; modified Romanowsky stain)
and the tumor nuclei stain with myogenin (20X; myogenin immunohistochemical stain).
DISCUSSION
Adult perianal Rhabdomyosarcomas are extremely rare and the true incidence is unknown.1 It is estimated to account for less than 1% of all adult solid tumor malignancies.2 The prognosis is poor with a 5-year overall survival rate of only 27% in adults without metastasis after curative treatment. The prognosis can be even more dismal with the presence of distal metastasis.3,4 The most common origin of primary tumors is the head and neck region (35%), followed by the genitourinary and extremities.5 However, primary tumors can also rarely occur at other anatomic sites like the rectum. Differential diagnoses of perianal tumors are neuroendocrine tumors, hematopoietic/ lymphoid malignancies, rectal carcinoma, melanoma, Ewing’s sarcoma and desmoplastic small round cell tumor.6 Tissue diagnosis with immunohistochemical stains is required for a definitive diagnosis. Due to the rarity of the disease, there is no standard way of obtaining the tissue diagnosis. To date, there is only one other case report mentioning EUS as a tool for diagnosing perianal Rhabdomyosarcoma.7 Open biopsy has been done in the past for diagnosis of Rhabdomyosarcoma. However, EUS is minimally invasive, more accurate, less expensive and safe compared to open biopsy.8
CONFLICTS OF INTEREST
None of the authors have conflicts of interest.
CONSENT
No recognizable patient material is used and therefore no patient consent was obtained.
ACKNOWLEDGEMENTS
No financial obligations or acknowledgements to make.