1. Saisho Y. Beta-cell dysfunction: Its critical role in prevention and management of type 2 diabetes. World J Diabetes. 2015; 6(1): 109-124. doi: 10.4239/wjd.v6.i1.109
2. Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes. 2003; 52(1): 102-110. doi: 10.2337/diabetes.52.1.102
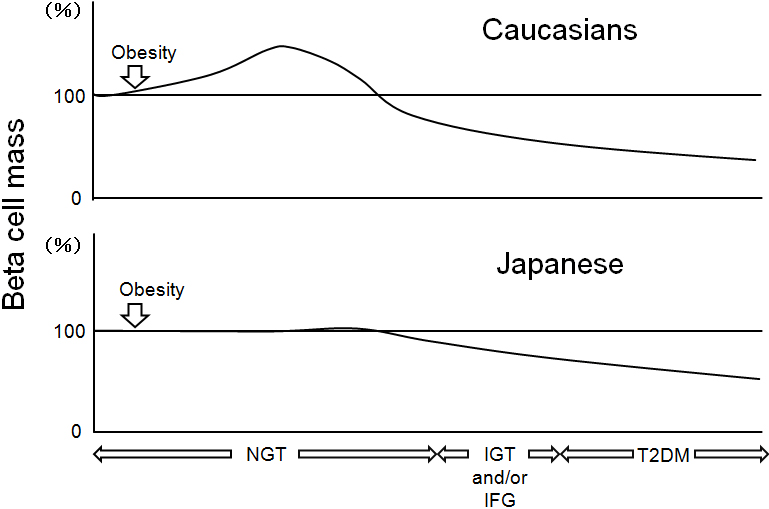
3. Saisho Y, Butler AE, Manesso E, Elashoff D, Rizza RA, Butler PC. Beta-cell mass and turnover in humans: Effects of obesity and aging. Diabetes Care. 2013; 36(1): 111-117. doi: 10.2337/dc12-0421
4. Rahier J, Guiot Y, Goebbels RM, Sempoux C, Henquin JC. Pancreatic beta-cell mass in European subjects with type 2 diabetes. Diabetes Obes Metab. 2008; 10 (Suppl 4): 32-42. doi: 10.1111/j.1463-1326.2008.00969.x
5. Talchai C, Xuan S, Lin HV, Sussel L, Accili D. Pancreatic beta cell dedifferentiation as a mechanism of diabetic beta cell failure. Cell. 2012; 150(6): 1223-1234. doi: 10.1016/j.cell.2012.07.029
6. Mizukami H, Takahashi K, Inaba W, et al. Involvement of oxidative stress-induced DNA damage, endoplasmic reticulum stress, and autophagy deficits in the decline of beta-cell mass in Japanese type 2 diabetic patients. Diabetes Care. 2014; 37(7): 1966-1974. doi: 10.2337/dc13-2018
7. Sato S, Saisho Y, Inaishi J, et al. Effects of glucocorticoid treatment on beta- and alpha-cell mass in Japanese adults with and without diabetes. Diabetes. 2015; 64(8): 2915-2927. doi: 10.2337/db15-0151
8. Kou K, Saisho Y, Satoh S, Yamada T, Itoh H. Change in beta-cell mass in Japanese nondiabetic obese individuals. J Clin Endocrinol Metab. 2013; 98(9): 3724-3730. doi: 10.1210/jc.2013-1373#sthash.hXFoUtgi.dpuf
9. Hsia DS, Larrivee S, Cefalu WT, Johnson WD. Impact of lowering BMI cut points as recommended in the Revised American Diabetes Association’s Standards of Medical Care in Diabetes-2015 on diabetes screening in Asian Americans. Diabetes Care. 2015; 38(11): 2166-2168. doi: 10.2337/dc15-0299
10. Inaishi J, Saisho Y, Sato S, et al. Effects of obesity and diabetes on alpha- and beta-cell mass in surgically resected human pancreas. J Clin Endocrinol Metab. 2016; 101(7): 2874-2882. doi: 10.1210/jc.2016-1374
11. Meier JJ, Breuer TG, Bonadonna RC, et al. Pancreatic diabetes manifests when beta cell area declines by approximately 65% in humans. Diabetologia. 2012; 55(5): 1346-1354. doi: 10.1007/s00125-012-2466-8