INTRODUCTION
Obesity epidemic in Middle East and North Africa region (MENA) is one of the highest worldwide. The prevalence of obesity has been estimated to affect about 19% of the people living in the MENA region.1 Moreover, in the year 2016 the World Health Organization reported a global incidence of more than 1.9 billion adults were overweight and of these over 650 million were obese.2 While in 2015, global burden of disease study group explored the global health data among the 20 most populated countries, they observed highest level of adult obesity in Egypt (35.3%).3
In addition, obesity is considered the fifth leading risk for global mortality. Thus, creating a major burden on the health care in these countries.1 Determination of body mass index (BMI) is the most convenient measure of overweight and obesity.2 Few studies have been conducted in developing countries; with main focus on understanding the epidemiological, socioeconomic, nutritional factors and obesity related health problems.2,3,4
Obesity is a disease characterized by increased accumulation of body fat, the cause is not always attributable to overconsumption of calories or lack of physical activity. Obese subjects often encounter impaired metabolic pathways along with disturbed signaling for hunger and satiety.3 Obesity management includes lifestyle modification in the form of dietary restriction and other behavioral changes that can be maintained indefinitely to promote health.5 Anti-obesity prescriptions counted as lifestyle modification adjunct to enhance initiation and continuance of weight loss in obese subjects with BMI above 30 kg/m2 or for those with a BMI above 27 kg/m2 when comorbidities exist.5 Moreover, anti-obesity prescriptions are recommended when efforts to lose weight are encountered with resistance.6 Many anti-obesity prescriptions assist body weight reduction and promote improvement of metabolic factors.4,6
Various anti-obesity prescriptions have been approved for long-term use to manage obesity; these include sibutramine, a selective noradrenaline/serotonin reuptake inhibitor. It has the potential ability to improve metabolic factors as insulin resistance, and lipid-profiles.6 Orlistat, a potent and reversible gastrointestinal lipase inhibitor prevents dietary fat absorption. It is proven to improve cardiometabolic factors, comprising blood pressure, plasma glucose, and lipid profiles.7 Orlistat is currently the only available drug for the long-term management of obesity.7 Glucagon-like peptide-1 (GLP-1) analogues, gastrointestinal hormones that enhance insulin secretion from pancreatic β-cells. long-term use of GLP-1 analogues reduces HbA1c level and blood pressure.5 Also, Tesofensine is an inhibitor of noradrenaline, dopamine and serotonin reuptake.8
This clinic interview-based study has been conducted to:
1. Describe demographic and clinical characteristics of obese and overweight participants
2. Explore views about effectiveness of obesity management strategies including dietary control, exercise and adjuvant anti-obesity prescriptions.
METHODS AND SUBJECTS
Method and Subjects Recruitment
This is cross-sectional qualitative exploratory interview. Study participants were obese and overweight individuals attending nutrition clinics, during the period from January 2016 till April 2017. The purpose of the study was explained to all participants via plain language statement and written informed consent was taken from those who were willing to participate in the study and data confidentiality was ensured as per national ethical guidelines.
Selected participants included were adults above the age of 18-years who, attended nutrition clinics for more than 4-months and have been following weight reduction regimen. Dietary control surveyed was mainly Mediterranean diet either solely or combined with exercise depending on participants will.
Mediterranean diet followed was a hypocaloric regimen with low-carbohydrate less than 50% and low-fat content 30% mostly obtained from olive oil; limited amounts of dairy products and meat, with a considerable contribution of fruits and vegetables as lentils and beans.9 For each participant, daily consumption was calculated by a nutritionist ranging from 1,200 to 2,000 calories per day.
Physical activity level was assessed using a Physical Activity Questionnaire scores and were categorized into 3 levels: (1) low inactive state “sedentary life”, (2) moderate activity; 3 days of vigorous activity for about 20 minutes per day (3) high activity; daily exercise of more than 5 days of moderate activity as walking for about 30 minutes per day, and or combination with vigorous activities.10 Accordingly, participants who had performed daily physical exercise were assigned level.3
Adjuvant pharmacotherapy; was considered in participants who failed to reduce body weight at least 0.5 kg per week after three months of implementing Mediterranean diet either alone or combined with exercise or subjects who had associated comorbidities such as diabetes.
Prescriptions frequently adopted in nutrition clinics included one of the
subsequent agents:
1. Drugs that diminishes fat absorption as Orlistat (brand name: Xenical).
2. Drugs that potentiate insulin action as Chromax® is a patented salt of trivalent chromium (Cr3+) and tripicolinic acid, also known as chromium picolinate/or Glucophage, a cofactor for insulin, it promotes activation of insulin receptors on cells and thus increases insulin sensitivity.
3. Prescriptions that enhance intestinal motility (Laxatives) thus, decrease net amount of nutrients absorbed as Senna and Plantago. Breakdown products of Senna act directly as irritants on the colonic wall to induce fluid secretion and stimulate colonic motility.
Data Collection
Participants were interviewed by trained interviewers using a pretested questionnaire at nutrition clinics. The interview was conducted in a semi-structured format, consisted of 50 questions allowing participants to contribute their personal experiences in attempting to reduce body weight.
The questionnaires were developed by a committee which included academics (Pharmacology staff members) and nutritionists with expertise in obesity, physical activity, and community department in Alexandria Faculty of Medicine. Questionnaire was created to collect information regarding the following points of interest:
1) Demographic variables of the participant such as age, sex, socioeconomic status and presence of family factors as obesogenic home environment, eating habits, physical activity and presence of comorbidities.
2) Participants’ beliefs about weight control and healthy eating behaviors. Type of weight management strategy followed and individual body response.
Anthropometric Measurements
BMI was determined using height and weight standardized procedure. Weight was measured in Kilogram (kg) using accurate scales checked regularly using known standardized weight, and height was measured using standardized measuring boards with accuracy to 0.1 cm. BMI was calculated by dividing body weight (kg) by squared height (m2 ).
Assessment of obesity concurred withrecommendations of the World Health Organization (WHO) consultation on obesity: normal, BMI <25 kg/m2; overweight, 25-29.9 kg/m2; class I obesity, 30–34.9 kg/m2 ; class II obesity, 35-39.9 kg/m2 ; and class III obesity, ≥40 kg/m2.1
Biochemical Parameters Measured
Blood samples were collected for serum lipid profile tests. The biochemical estimations were carried out in licensed and accredited laboratories.
The following biochemical parameters were determined:
Serumtotal Cholesterol, low density lipoprotein-Cholesterol (LDL-Cholesterol), high density lipoprotein-Cholesterol (HDL-Cholesterol) and triglyceride (TG).
STATISTICAL ANALYSIS
The data was collected and entered into the personal computer. Statistical analysis was done using Statistical Package for Social Sciences (SPSS/version 20) software. Arithmetic mean, standard deviation, for categorized parameters, chi square test was used while for numerical data T-test was used to compare two groups while for more than two groups ANOVA test was used. To find the association between two variables, spearman correlation coefficient test was used the level of significant was 0.05.
RESULTS
The present study included 2,240 participants who were sampled from nutrition clinics in different districts in Alexandria city. Participants were classified according to BMI into: group I obese subjects and included 59.8% of studied participants, the mean age was 38.2±9.85years and group II overweight subjects and included 40.2% of studied participants, with mean age 29.1±11 years.
Table 1 demonstrated the demographic data of enrolled participants. Among participants in both groups; significantly greater number of females compared to males. The highest age group frequency was among age group 30-40 years in group I and 18-20 years in group II.
| Table 1. Demographic Data of the Studied Groups |
|
Group I: Obese (n=1339)
|
Group II: Overweight (n=901) |
p
|
|
No
|
% |
No |
%
|
|
|
Sex
|
|
|
|
|
|
|
Male
|
452 |
33.8 |
382 |
42.4 |
0.008*
|
|
Female
|
887 |
66.2 |
519 |
57.6
|
|
Age (years)
|
|
|
|
|
|
|
18-20
|
147 |
11.0 |
347 |
38.5
|
0.001*
|
|
20-29
|
256 |
19.1 |
279 |
31.0
|
|
30-39
|
549 |
41.0 |
128 |
14.2
|
|
40-50
|
313 |
23.4 |
101 |
11.2
|
|
50+
|
74 |
5.5 |
46 |
5.1
|
|
Mean±S.D
|
38.2±9.85
|
|
|
| Nature of patient’s life style (physical activity) |
|
Sedentary (level 1)
|
568 |
42.4 |
428 |
47.5 |
|
| Moderate (level 2) |
323 |
24.1 |
99 |
11.0
|
|
|
Heavy (level 3)
|
448 |
33.5 |
374 |
41.5
|
|
1Significant at p≤0.05
p was calculated by using Chi square test |
Moreover, 33.5% of group I engaged in daily physical exercise and 41.5% of group II respectively, in which they were assigned level 3 physical activity.
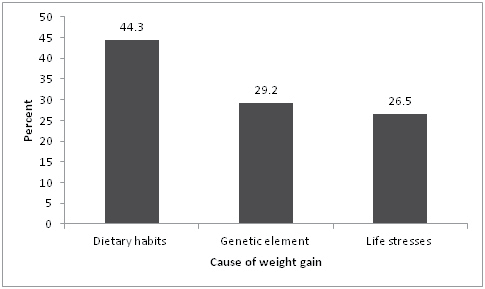
The main cause of weight gain as reported by, 44.3% of participants (992) was due to dietary habits that started early in childhood, while 29.2% claimed presence of a genetic factor (594 participant); they declared a positive family history of obesity. On the other hand, 26.5% of participants (654) reported that the weight gain was due to life-stresses as indicated in (Figure 1).
Figure1. Causes of Weight Gain
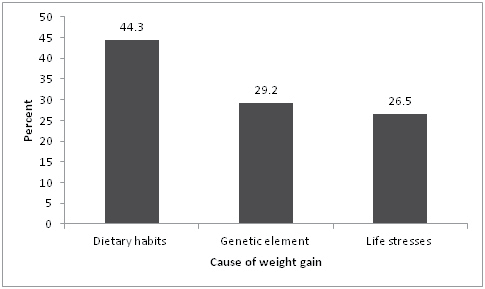
Table 2 showed that dietary control regimen solely was adopted in 55.8% of group I and 59.5% of group II of participants. Also, intake of adjuvant anti-obesity prescriptions was significantly higher among group I participants. Interestingly, a considerable number of participants complained from fluctuating weight regain; the percentage was about 19.4% group I and 23.6% in group II.
| Table 2. Distribution of the Studied Groups Regarding Weight Management Strategy Followed |
|
Group I: Obese (n=1339)
|
Group II: Overweight (n=901) |
X2 |
p
|
|
No
|
% |
No |
%
|
| Dietary control solely |
747
|
55.8 |
536 |
59.5 |
3.016 |
0.082
|
| Dietary control plus exercise |
395
|
29.5 |
351 |
39.0 |
21.686* |
* <0.001*
|
| Dietary control plus adjuvant anti-obesity prescriptions |
143
|
10.7 |
14 |
1.5 |
68.818* |
<0.001*
|
| Dietary control plus both exercise and adjuvant antiobesity prescriptions |
54
|
4.0 |
0 |
0 |
37.234* |
<0.001*
|
*Significant at p≤0.05
p was calculated by using Chi square test
Dietary control followed was mainly mediterranean diet |
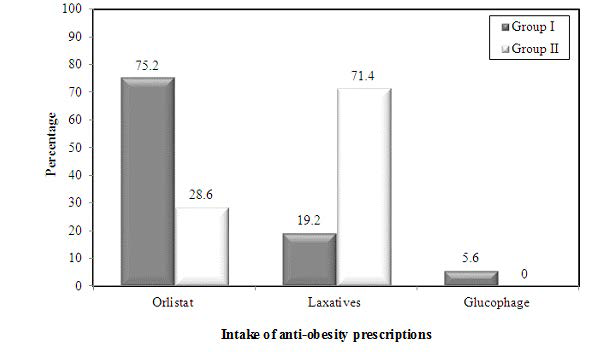
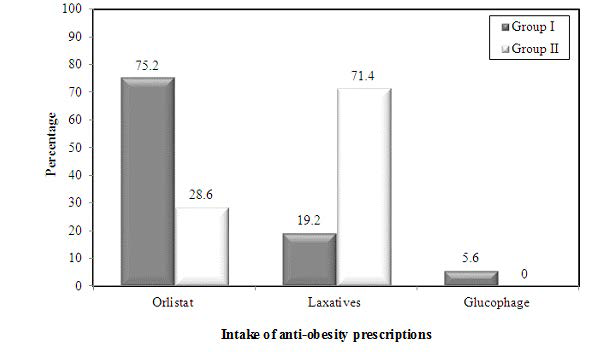
Figure 2 showed that 14.7% of Group I (197participants) received anti-obesity prescriptions, mostly received Orlistat 75.2% (148 participant); followed by laxatives (Senna, Royal Regime tea) were19.2% (38 participant) and least Glucophage were 5.6%(11 participants). while, 1.5% Group II received anti-obesity prescriptions mostly received Laxatives in 71.4% (10 participant). While the remaining 28.6% received Orlistat (4 participants).
Figure 2. Distribution of the Two Groups Regarding Intake of Anti-Obesity Prescriptions
The percentage decrease in body weight as obtained from interview data was significantly highest among participants who followed (Dietary control plus both exercise and anti-obesity prescriptions) strategy compared to other strategies in both groups as shown in (Table 3).
| Table 3. Percentage Decrease in Body Weight in Relation to Weight Management Strategy |
|
Dietary control, exercise, anti-obesity prescriptions (n=1339)
|
Dietary control plus exercise |
Dietary control solely
|
|
Range
Mean
S.D
|
12.0-19.0
16.8
3.98 |
5.0-18.0
12.72
3.65 |
6.0-12.0
8.69
1.03
|
|
F
p
|
115.858
<0.001*
|
|
|
| Sig. bet. grps. P1 = 0.001*, p2 = 0.001* |
* Significant at p≤0.05 p was calculated by using ANOVA-test Sig. bet. grps was done usingPost Hoc Test (LSD)
p1 : p value for comparing between Dietary control, exercise, anti-obesity prescriptions and Dietary control solely
p2 : p value for comparing between Dietary control plus exercise and Dietary control solely |
Blood samples were withdrawn at time of interview after a 12-hour fasting period. Lipid profile results revealed that Total cholesterol (TC), low density lipoprotein -Cholesterol (LDL-C) and Triglycerides (TG) were increased in both groups. However, only TG was significantly higher in group I relative to group II as shown in (Table 4).
| Table 4. Lipid Profile in Studied Groups |
|
Group I: Obese (n=1339)
|
Group I: Overweight (n=901) |
p
|
|
T.C (mg/dl)
|
223.77±24.32 |
210.89±17.89 |
0.065
|
|
HDL-C (mg/dl)
|
4.46±7.65 |
48.34±4.57 |
0.107
|
|
LDL-C (mg/dl)
|
138.28±21.67 |
128.78±19.16 |
0.098
|
|
TG (mg/dl)
|
167.29±34.68 |
149.45±29.89 |
0.032*
|
|
* Significant at p≤0.05
|
p was calculated by using T-test
|
|
In addition, presence of comorbid conditions was more significantly pronounced among group I compared to group II with highest incidence of dyslipidemia and lowest among others as infertility and cardiovascular disorders as shown in (Table 5).
DISCUSSION
Previous studies reported increasing prevalence of obesity and overweight in developing countries.11,12 MENA region study stated that about one fifth of the adult population are considered obese.13 Moreover, systematic reviews suggested that about 31% of ischemic heart disease and 8% of stroke mortality were correlated with obesity, due to associated hypertension and dyslipidemia.14 A chief constraint in the former studies was data collected from different sources using diverse methods and therefore it was difficult for comparison throughout developing countries. Therefore, the present interview-based study used a considerably large sample of the data collected from nutrition clinics to explore the perception and value of dietary control, exercise and use of anti-obesity agents on both weight reduction and conservation.
In this study 59.8% of participants were obese (group I) and 40.2% were overweight (group II). Highest incidence of obesity was among participants in age group 30-39 years (41.0%), this finding was in agreement with previous study by Aitsi-Selmi et al. . In that study they found highest incidence of obesity among age group 25-35 years 42.8%.11 On the other hand, highest incidence of overweight was among adolescence 18-20 years (38.5%). In concordance with Manyanga et al, where it was reported that about 31.4% of school children were overweight in a survey performed in Egypt.15 Aitsi-Selmi et al also concluded that high prevalence of obesity among Egyptian youth may be indicative of nutrition transition due to rapid urbanization.11 Participants in the present study were familiar with obesity comorbidities; the majority of obese subjects suffered from dyslipidemia (47.6%), diabetes mellitus (35.1%) and hypertension (14.7%). On the contrary, Alsheikh-Ali et al reported a high prevalence of dyslipidemia (70%), followed by hypertension (43%) and diabetes mellitus (25%).12 Flegal et al performed a systematic review of hazard ratios (HRs) of all-cause mortality (cardiovascular, renal, neoplastic factors) for overweight and obesity relative to normal weight in the general population. They found grades 2 and 3 obesity (BMI of ≥35) were accompanied with significantly elevated all-cause mortality. The HRs were for obesity 0.95 (95% CI, 0.88-1.01) for grade 1 obesity, and 1.29 (95% CI, 1.18-1.41) for grades 2 and 3 obesity.14 In this interviewbased study, 44.3% of participants agreed that the primary cause of weight gain was nutrition pattern followed early during childhood and persisted into adulthood; plus in addition to, shift towards westernization leading to intake of excess junk food. Another factor, 26.5% of participants complained of life-stresses. Manyanga et al found high obesity incidence among Egyptian youth, they suggested that may be indicative of nutrition transition occurring in the context of rapid urbanization. Furthermore, these youth a were exposed to the proliferation of technology-based entertainments such as computer games at the expense of physical activity.15
In addition, physical inactivity rates (Sedentary life) were as high as 42.4% among group I participants versus 47.5% in group II, mostly in the age groups above 40 years. They complained of lack of time due to responsibilities related to family and social environment.
Consequently, deficiency of exercise could be considered an important factor when examining the correlation to obesity; it is believed that energy intake as opposed to energy expenditure is considered an important factor in obesity.14 Similarly, Yasin et al documented that physical exercise was least favorite among participants in a survey performed in Egypt 1998. They stated in their study that about 2% of participants reported practicing some sports on a daily basis.17
In regards to presence of genetic element, participants in both groups; 29.2% of participants stated a positive family history of obesity as, they believed that genetic factor might be considered as a possible cause of disturbed body metabolism and obesity. There are more than 56 different genes described to be related obesity phenotypes.Those genes mostly are genes that interact with environmental factors related to energy intake and expenditure.18
On the other hand, 26.5% complained of life stresses. They suggested that life-stresses influences food preferences, favoring foods rich in fat and sugar. Aside from overeating, stress can also lead to decreased motivation to exercise.16
Consistent with previous studies obesity management strategies focus on change of individual behavior specifically dietary pattern and exercise.19,20 Results from our interview suggested that a considerable number of participants were dissatisfied with weight management results in both groups (19.4% group I and 23.6% group II). Particularly participants who followed weight reduction strategy either dietary control “Mediterranean diet” solely or combined with exercise. Those participants stated that the cause maybe due to poor compliance, lack of motivation, also sometimes weight loss results were less than expected. On the contrary, Anderson et al performed a long-term observational study utilizing two groups of balanced diet for 5-years; very low carbohydrate diets (VLCDs) versus hypoenergetic balanced diets. They found that the VLCD group attained a significantly more net weight loss than the hypoenergetic balanced diet group (29% compared with 18%).21 The proposed mechanism for dietary control was that reduced intake of fat and carbohydrate rich food may be beneficial in weight loss by increasing satiety and by promoting fat oxidation at the expense of carbohydrate oxidation.22 Moreover, highprotein food as grilled meat, and food rich in fibers such as fresh vegetables and fruits have been shown to increase satiety, preserve fat-free mass.23 Hemmingsson et al also found that a considerable initial weight loss predicts long-term weight reduction.24
Participants from both groups (I and II) who followed daily exercise accompanied with dietary control achieved more satisfactory results. Since exercise plays an equivalent role to dietary restriction in terms of energy balance. Also, exercise improves insulin sensitivity, increasing aerobic capacity and mitochondrial function, with superimposed prevention of weight regain.25 However in another study, Redman et al found that when caloric restriction is precisely controlled, modifications in abdominal fat distribution are attained with no further addition of exercise.23 They reported fat depots, regardless of their location, were reduced by about 30% in men and 25% in women.23 Furthermore, Malis et al suggested that inability of caloric restriction to adjust body fat distribution would indicate that affected individuals are genetically or epigenetically predisposed for fat storage which cannot be easily overcome by dietary restriction.26 Besides, one of the beneficial effects of dietary restriction could be reduction of oxidative stress. Additionally, caloric restriction results in alterations in energy balance, due to reduced energy expenditure, as a consequenceof decreased oxygen consumption or mitochondrial adaptation.27,28
Bray and DeLany conveyed that anti-obesity drugs are less important tool in weight loss than exercise. Though pharmaceutical adjuvant anti-obesity prescriptions are recently gaining popularity; only 211 participants received anti-obesity prescriptions in this interview. Particularly among obese participants along side dietary restriction with or without exercise; mostly consumed Orlistat. Orlistat decreases intestinal fat absorption by about 30%.7 Similarly, Chanoine et al found that Orlistat was administered as adjuvant therapy together with a balanced diet and exercise, it resulted in a decrease in BMI by about 5% within 12-weeks.29 The second in use anti-obesity prescription received was laxatives as Royal regime tea; asit enhances intestinal motility and reduces nutrients absorption, and therefore should be accompanied with vitamin supplements.
The third pharmaceutical agent was anti-diabetic agents which was only consumed by group I; obese participants who received anti-diabetic agents stated that it increased satiety and improved insulin resistance. Anti-diabetic agents do not increase body weight, nevertheless they help to limit weight gain, improve associated hyperglycemia and clinical cardiovascular outcomes.30
Results from, lipid profile samples in this study results revealed significantly high total cholesterol in both groups (I and II), and elevated triglyceride in group I. This may be explained by prevalence of comorbidities as hypertension and diabetes. Another study reported significantly elevated LDL-cholesterol as a potentially important factor hindering obesity management.31 This observation may suggest that dietary pattern have a complex relationship with lipid profile.
CONCLUSION
Finally, this interview-based study revealed that main improvement in weight-reduction was seen in obese subjects following dietary control together with both exercise and adjuvant anti-obesity prescriptions. Although only 9.4 % of participants received anti-obesity prescriptions; The most commonly used anti-obesity prescription was Orlistat.
Furthermore, most common obesity comorbidity observed in obese participants was dyslipidemia; which may impede effective obesity management. Consequently, dietary control supplemented by anti-obesity prescriptions might be beneficial in obesity management in resistant cases.
Moreover, it is necessary to introduce educational programs that aim at promoting healthy dietand physical exercise, particularly commencing early in childhood.
ACKNOWLEDGEMENTS
We kindly appreciate the support of all members of pharmacology and Toxicology department at Faculty of Pharmacy, Pharos University, Alexandria, Egypt.
DISCLOSURE OF CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Equally contributed.
FUNDING
Pharos University in Alexandria.