INTRODUCTION
Cultural beliefs prevalent in the society have a very severe impact on the mind and behavior of the person. Sexuality is a very important but under discussed domain in public as well as in our education system.1,2 So there are many misbeliefs and misconceptions about sexuality prevalent in our society. Many cultures believe semen to be a very precious body fluid and its unnecessary loss to cause severe harm on the health of the person. Cultural myths in relation to semen loss can induce physical and psychological symptoms in a man which together as a syndrome termed as Dhat syndrome.3 “Dhat” is derived from the word “dhatu”. The word “Dhatu” is a Sanskrit word which means “Metal” or “Elixir”.3,4,5 There is description of seven “Dhatus” [Chyle (Rasa), Blood (Rakta), Flesh (Maans), Fat (Meda), Bone (Asthi), Marrow (Majja), Semen (Shukra)], out of which most important considered is “Shukra Dhatu (semen)”.
Dhat syndrome is described in The Diagnostic and Statistical Manual (DSM) IV as a Culture Bound Syndrome (CBS).6 There is an ongoing debate on nosological status of CBS.7 Dhat syndrome has been found to be prevalent in different geographical regions of the world.8 It has been described in literature from China, Europe, Americas, and Russia at different points of time in history.9 Mention of semen as a “soul substance” could be found in the works of Galen and Aristotle who have explained the physical and psychological features associated with its loss.10
The assumption that these cultures bound syndromes affect only specific cultures have resulted in limiting global interest in understanding these conditions and their management. However, these conditions are of serious concern as they have severe detrimental effects on the life of its sufferers. So we in our study tried to find out the most predisposed group for this syndrome, its impact on their life, their surroundings and the whole society and what could be done to relieve them of their sufferings.
MATERIAL AND METHODOLOGY
The study was conducted in Urology Department of S M S Hospital, Jaipur, India. The study was approved by the ethical committee of the institution. The study included 110 patients who presented in the urology clinic with the primary complaint of involuntary discharge of semen. Informed consent was taken from all the patients before including them in the study. Patients were excluded from the study if they didn’t appear for follow-up as advised. The patients were provided comfortable atmosphere and were taken in to confidence that their information will not be disclosed. The patients were enquired about their demographic profile (like age, marital status, educational status, occupation, socio-economic status, family details). They were specifically asked about their personal life like their sexual history, drug abuse, alcohol and smoking. They were enquired about their primary complaint of Dhat, timings of discharge, associated health problems or any sexual problem. They were asked about their beliefs regarding Dhat (questions asked are depicted in Table 1). To find the impact of their suffering of Dhat on their daily living, their health, their surroundings, their professional life and the society, they were asked few questions as listed in Table 2. The response was recorded as never, regular, sometimes.
Urine analysis was done in every patient. Patients were counseled, taught about their condition in detail, were asked to raise their doubts and sexual education was imparted to them. Patients were then called for follow-up after 1 week. Above questions (as in Table 1) were again asked.
| Table 1: Questions asked about their beliefs regarding Dhat |
| What is the substance you think is discharged in Dhat? |
| What do you think is responsible for this condition? |
| What do you think will be the consequences if you continue to have Dhat? |
| Table 2: Questions asked about impact of their suffering of Dhat on their daily living, their health, their surroundings, their professional life and the society. |
| During the past week, did they feel: |
| A vague feeling of fear? |
| Lack of energy? |
| Disturbed sleep? |
| Somatic symptoms like body ache, fainting, dizziness etc.? |
| No interest in work? |
| No interest in surroundings? |
| Easily becomes irritated? |
| They can’t enjoy anything anymore? |
| Easily become emotional? |
| That everything is meaningless? |
| Unnecessarily feeling afraid? |
| Afraid of going to social gatherings? |
| Feel of inferiority complex? |
| Feel life is not worthwhile? |
| Think ‘I wish I was dead”? |
Data was collected and Statistical analyses were performed using the Statistical Package for the Social Science Version (SPSS). Descriptive analysis were analyzed in terms of mean and standard deviation for continuous variables. Frequency with percentage was used for nominal variables.
RESULTS
Assessment of Demographic Profile of Patients
The study included 110 male patients presenting with Dhat syndrome. The mean age of study sample was 23.53 years with an age range of 15-68 years. The most affected age group was of 18-25 years which constituted about 60% of patients, about 25 % were in the age range of 25-35 years, 10% were below 18 years while 5.5% patients were aged above 35 years. More than two-third (70%) of the patients were unmarried, the rest were either married (20%) or widowed/divorcee (10%). The condition had a high prevalence in educated population as well, and about 50% of patients were graduate or above. Majority of the patients were either unemployed or student (49.1 %). About half of patients had monthly family income of less than Indian Rupees 10,000 and 24.5% people had monthly income less than Indian Rupees 5000. The condition was prevalent in both urban and rural community with about two third patients belonging to rural areas. Dhat syndrome was more common in people who were living alone (54.5%) or in nuclear family (30%) as compared to joint family and in people who had no previous history of having sex (60%).
Demographic Profile
|
Age
|
<18(10%) |
18-25(60%) |
25-35(24.5%) |
>35(5.5%)
|
|
|
Educational status
|
Illiterate (22.7%) |
Up to 10th (27.3%) |
Up to graduate (45.5%) |
Above graduate (4.5%)
|
|
|
Occupation
|
Unemployed/Student (49.1%) |
Unskilled worker (20%) |
Skilled worker (17.2%) |
Clerical/farmer (8.2%) |
Professional (5.5%)
|
|
Monthly family income
|
<5000 (24.5%) |
5000-10000 (50%) |
10000-20000 (20%) |
>20000 (5.5%)
|
|
|
Marital status
|
Un-married (70%) |
Married (20%) |
Separated (10%)
|
|
|
|
Previously ever had sex
|
No (60%) |
Yes (40%)
|
|
|
|
|
Type of family
|
Nuclear (30%) |
Joint (15.5%) |
Alone (54.5%)
|
|
|
|
Residence
|
Rural (63.6%) |
Urban (36.4%)
|
|
|
|
|
Smoker
|
Yes (54.5%) |
No (45.5%)
|
|
|
|
|
Alcoholic
|
Regular (20%) |
Occasional (45.5%) |
Never (34.5%)
|
|
|
|
Drug abuse
|
Yes (20%) |
No (80%)
|
|
|
|
Clinical Profile
The mean duration of symptoms at the time of presentation was 22 months, and nearly two-third of patients were passing Dhat every week while one-fourth of patients were passing Dhat at least once in a day. Most of the patients complained of passage of Dhat while urination More than two-third of patients have not consulted anyone while about 20% have consulted quacks or so called sexologists. When asked about associated sexual complaints, about 75% were worried about their habit of masturbation. About one third reported that their semen is thin and about 10% reported erectile dysfunction. Majority of patients reported generalized weakness, about two third patients complained of constipation and about 10% reported burning micturition.
Clinical Profile
|
|
n |
%age
|
| Duration of Suffering |
| <6 months |
12
|
10.9
|
| 6 months-1year |
23
|
20.9
|
| >1 year |
75
|
68.2
|
| Frequency of Passage of Dhat |
| Everyday |
29
|
26.4
|
| Every week |
67
|
60.9
|
| Once a while |
14
|
12.7
|
| When they have Passage of Dhat* |
| While passing urine |
75
|
68.2
|
| While straining for passing stools |
10
|
9.1
|
| During sleep |
50
|
45.4
|
| While sexual excitement |
40
|
36.4
|
| Anytime |
25
|
22.7
|
| What they have Done till now for this |
| Nothing |
74
|
67.3
|
| Consulted quacks |
24
|
21.8
|
| Consulted doctors |
12
|
10.9
|
| Any Associated Sexual Complaint Reported by Patients* |
| Erectile dysfunction |
10
|
9.1
|
| Premature ejaculation |
5
|
4.5
|
| Masturbation |
75
|
68.2
|
| Thin semen |
35
|
31.8
|
| Small penis |
5
|
4.5
|
| No other sex related symptoms |
10
|
9.1
|
| Any Associated Health Problem Reported by Patient* |
| Constipation |
65
|
59.1
|
| Asthenia |
95
|
86.4
|
| Insomnia |
40
|
36.4
|
| Body ache |
45
|
40.9
|
| Anxiety |
60
|
54.5
|
| Burning micturition |
10
|
9.1
|
| No refer to any other associated health problem |
2
|
1.8
|
| *A patient can have more than one response. |
Urinanalysis
Urinanalysis of the patients did not show spermatozoa in any patient. Only about 5% patients showed pus cells, about 5% showed RBC and about 2% showed crystals. Urinanalysis of rest of the patient showed no abnormality.
|
Urinanalysis
|
n |
%
|
| Spermatozoa |
–
|
–
|
| Pus cells |
5
|
4.5
|
| Crystals |
2
|
1.8
|
| RBC |
5
|
4.5
|
| No abnormality |
102
|
92.7
|
Belief of Patients
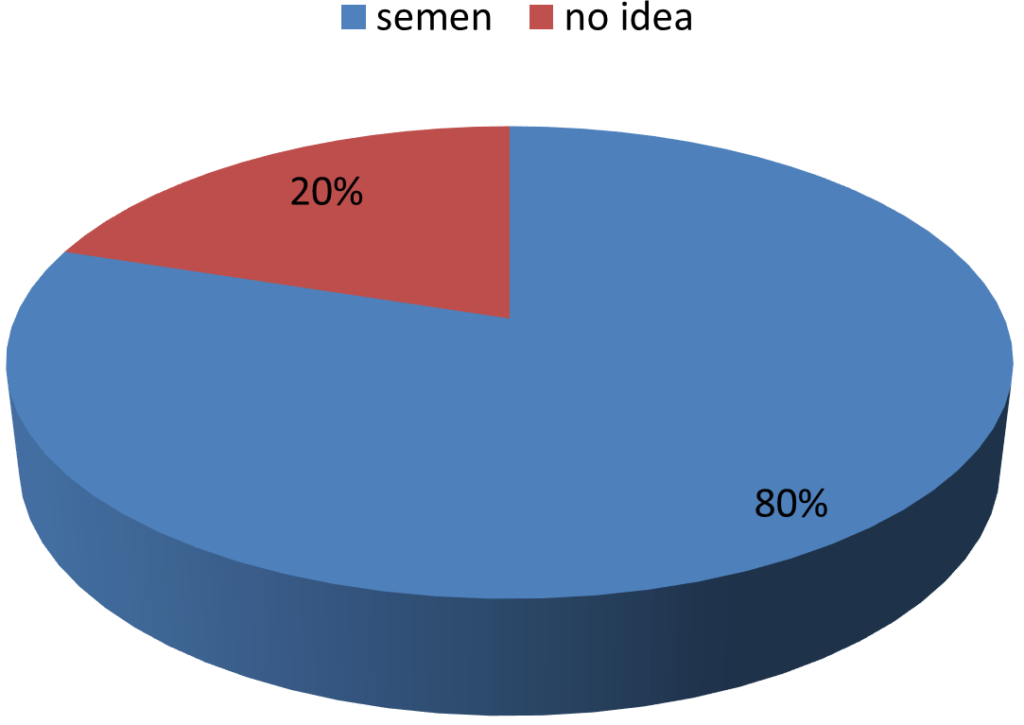
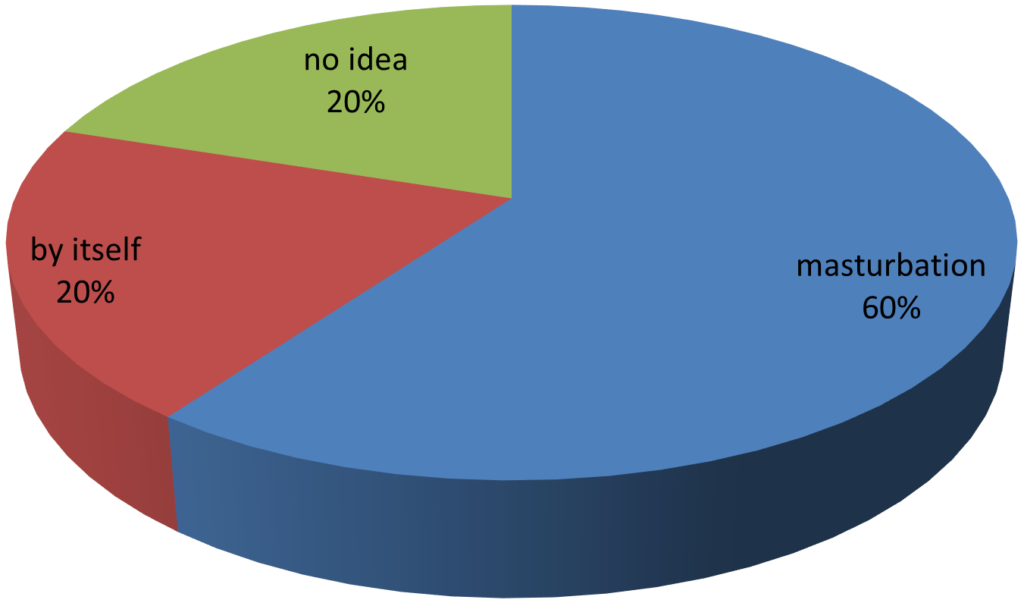
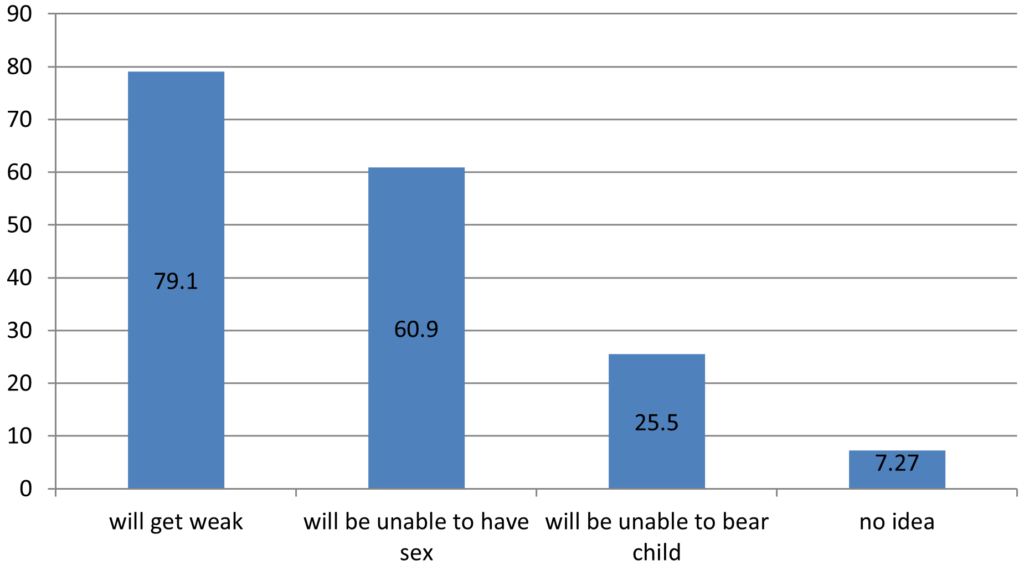
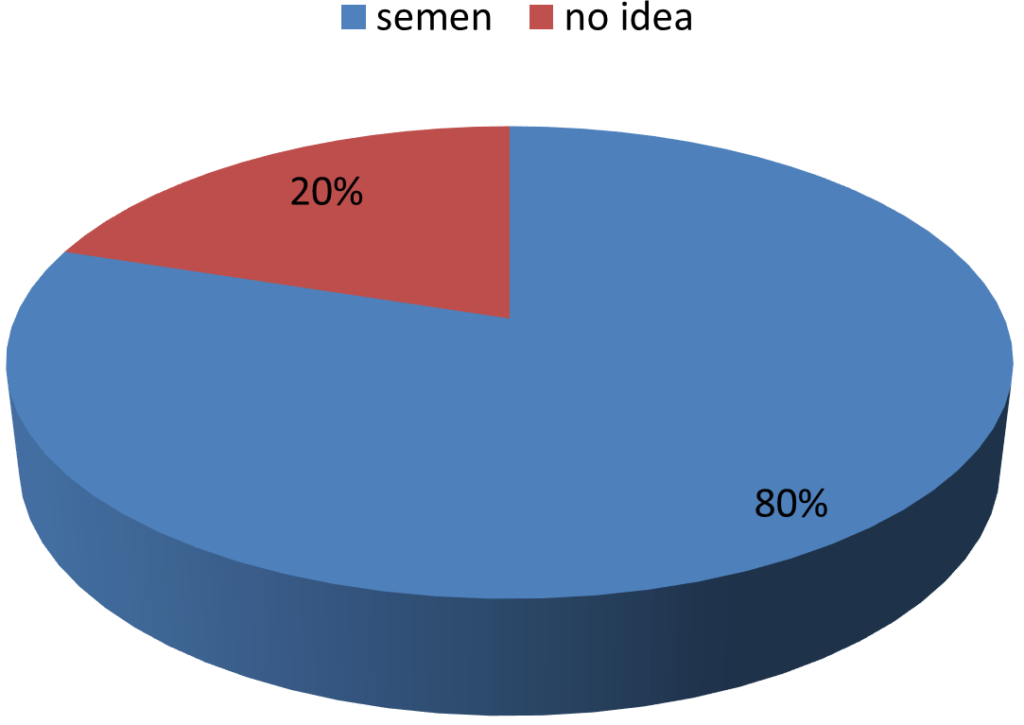
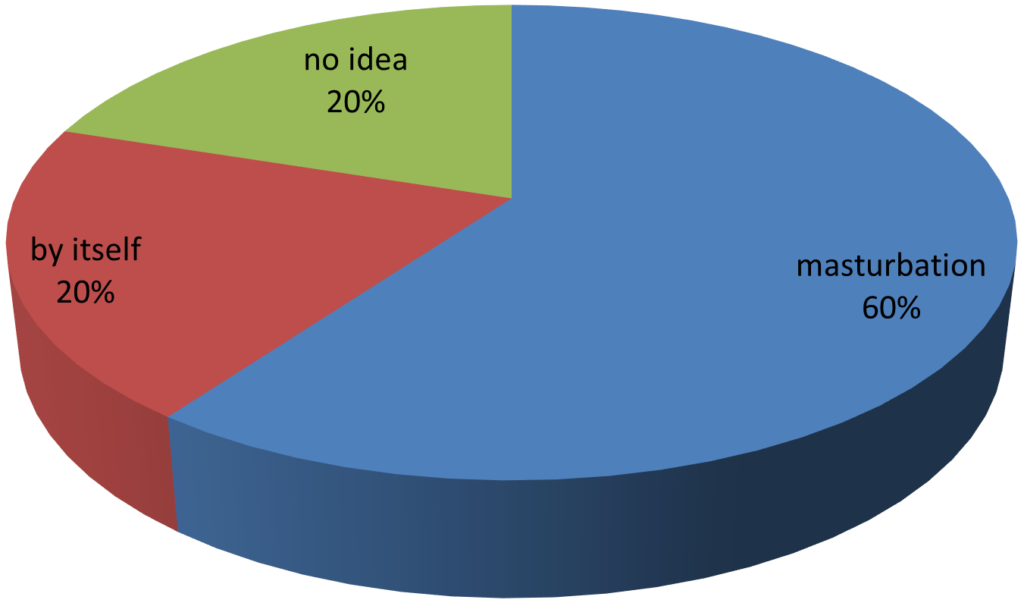
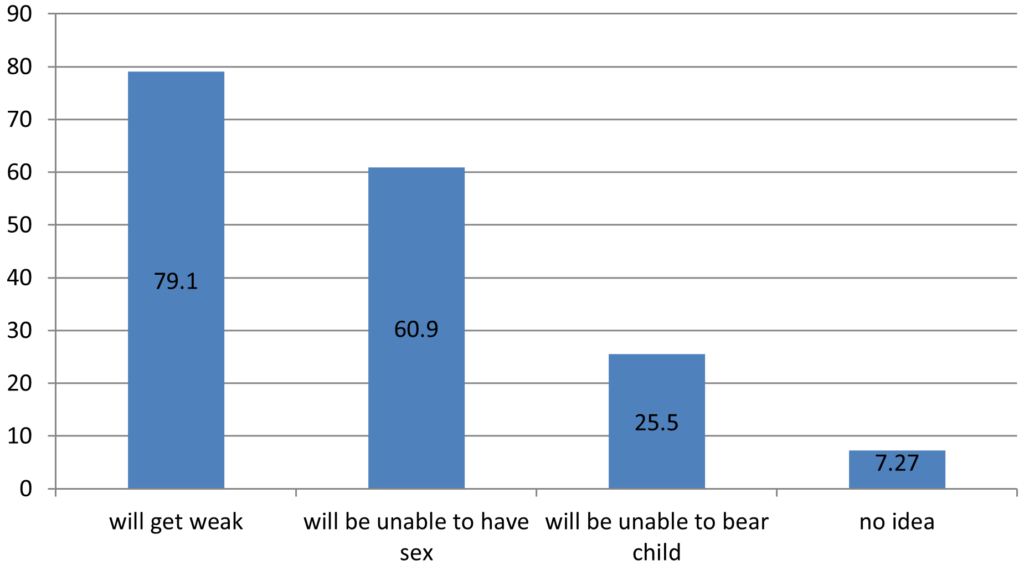
80% patients believed that they are losing semen in Dhat while 20% had no idea. About two third patients believed that they are passing Dhat because of some defect they have created by doing masturbation. Majority of patients thought that if they continue to have Dhat then they will get weak, while about 60% thought that they will be unable to have sex, about one fourth were worried that they will not be able to bear child.
What they think Dhat is?
What they think is responsible for their suffering?
What will be the consequences?
Impact on Society
It is clear from the response of patients to the questions asked (as shown in Table 2), that Dhat syndrome had severe impact on their daily living, their health, their surroundings, their professional life and the society. More than half of patients have regularly no interest in work and in their surroundings. About all the patents feel lack of energy and majority of patients also had disturbed sleep and complain of somatic symptoms like body ache, fainting, dizziness. About half of patients regularly remain irritable. Significant number of patients thought that everything is meaningless, feel life is not worthwhile and even wish to be dead.
Response of the patients to questions asked to find the impact of their suffering of Dhat on their daily living, their health, their family and surroundings, their professional life and the society:
|
During the past week, did they feel:
|
Never n (%) |
Sometimes n(%)
|
Regular n (%)
|
| A vague feeling of fear? |
13(11.8)
|
64(58.2) |
33(30)
|
| Lack of energy? |
0(0)
|
35(31.8) |
75(68.2)
|
| Disturbed sleep? |
18(16.4)
|
54(49.1) |
38(34.5)
|
| Somatic symptoms like body ache, fainting, dizziness etc. |
18(16.4)
|
43(39.1) |
49(44.5)
|
| No interest in work? |
18(16.4)
|
33(30) |
59(53.6)
|
| No interest in surroundings |
16(14.6)
|
37(33.6) |
57(51.8)
|
| Easily becomes irritated |
21(19.1)
|
35(31.8) |
54(49.1)
|
| They can’t enjoy anything anymore |
23(20.9)
|
44(40) |
43(39.1)
|
| Easily become emotional |
18(16.4)
|
38(34.5) |
54(49.1)
|
| That everything is meaningless |
23(20.9)
|
52(47.3) |
35(31.8)
|
| Unnecessarily feeling afraid |
28(25.5)
|
34(30.9) |
48(43.6)
|
| Afraid of going to social gatherings |
38(34.5)
|
44(40) |
28(25.5)
|
| Feel of inferiority complex |
23(20.9)
|
28(25.5) |
59(53.6)
|
| Feel life is not worthwhile |
33(30)
|
46(41.8) |
31(28.2)
|
| Think ‘ I wish I was dead” |
38(34.5)
|
49(44.6) |
23(20.9)
|
At follow-up, after counseling and sex education, correction of misbeliefs and reassurance, response of the patients to similar questions:
|
During the past week, did they feel:
|
Never n(%) |
Sometimes n(%) |
Regular n(%)
|
| A vague feeling of fear? |
84(76.3)
|
19(17.3) |
7(6.4)
|
| Lack of energy? |
78(70.9)
|
24(21.8) |
8(7.3)
|
| Disturbed sleep? |
76(69.1)
|
27(24.5) |
7(6.4)
|
| Somatic symptoms like bodyache, fainting, dizziness etc. |
80(72.7)
|
22(20) |
8(7.3)
|
| No interest in work? |
84(76.3)
|
19(17.3) |
7(6.4)
|
| No interest in surroundings |
82(74.5)
|
20(18.2) |
8(7.3)
|
| Easily becomes irritated |
74(67.3)
|
26(23.6) |
10(9.1)
|
| They can’t enjoy anything anymore |
76(69.1)
|
26(23.6) |
8(7.3)
|
| Easily become emotional |
79(71.8)
|
18(16.4) |
13(11.8)
|
| That everything is meaningless |
82(74.5)
|
17(15.5) |
11(10)
|
| Unnecessarily feeling afraid |
74(67.3)
|
23(20.9) |
13(11.8)
|
| Afraid of going to social gatherings |
79(71.8)
|
21(19.1) |
10(9.1)
|
| Feel of inferiority complex |
76(69.1)
|
23(20.9) |
11(10)
|
| Feel life is not worthwhile |
89(80.9)
|
15(13.6) |
6(5.5)
|
| Think ‘ I wish I was dead” |
92(83.6)
|
14(12.7) |
4(3.7)
|
Impact of Counseling and Reassurance
By comparing the initial response of patients with the response after counseling and reassurance, it is clear that there was a dramatic positive response on the life of patients after counseling and reassurance only. Majority of patients though continued to have Dhat, were able to take interest in their work, their surroundings and in their own life. Majority of patients were able to have a healthy physical, mental and social well-being.
DISCUSSION
Dhat syndrome, although described as culture bound syndrome, has been found to be prevalent in different geographical regions of the world and has been found to be emerging in other countries as well. A significant number of patients with Dhat syndrome come to urologist consultation but there have been very limited reports that describe or analyze this syndrome in urological literature.11 In the case of Dhat syndrome, the nature of underlying belief, i.e., ‘semen is the most vital fluid and has to be conserved at any cost’ is such that there is intense distress in the wake of continued loss of dhat.12 Sumathipala, et al.13 and Balhara, et al.7 have reported that Dhat syndrome was not confined to Oriental countries infact it was prevalent in Europe, USA and Australia in the nineteenth century.
In our study we found that Dhat syndrome is mainly prevalent in particular strata of population: young male, living alone or in nuclear family, with low income, although more common in rural community but is also prevalent in urban areas, common in illiterate as well as well-educated men. Few previous studies conducted by Chaddha, et al.,14 Grover S, et al.15 and Gautam M, et al.16 reported that patients complaining of Dhat Syndrome are typically more likely to be young people, who are recently married or single; of average or low socio-economic status, coming from a rural area and belonging to a family with conservative attitudes towards sex while a study conducted by Verma R, et al.17 reported more prevalence from urban area.
In our study, the mean duration of symptoms at the time of presentation was 22 months, and nearly two-third of patients were passing Dhat every week while one-fourth of patients were passing Dhat at least once in a day . In a recent study conducted in Spain by Menendez et al11 25% of patients complained of daily sperm loss while in 37.5% it was weekly and patients complained of the syndrome lasting from 3 months up to 10 years. In a study conducted by De Silva P, et al.18 complaint of duration of the semen loss lasts up to 20 years.
As reported by Grover S, et al.19 and Rajkumar R, et al.20 our study also showed that patient complaining of passage of Dhat also complains of various somatic symptoms most common being generalized weakness (86.4%) and constipation (59.1%) and also some irrelevant sex related problems like fear of thin semen or small penis.
Most of the patients believed that they are losing semen in Dhat and more than half of patients consider this to be a consequence of their habit of masturbation. Infact their self guilt of masturbation due to the misconceptions prevalent in the society lead to these false attributes.21
They are so much threatened by the misbeliefs in the society that they believe that they will get very weak and will not be able to do sex or bear child. Due to these fears their physical and mental health; and personal and social life get so much disturbed as clearly shown by our study that they lose all their interest in their work, their surroundings and have a feel of fear and tiredness.
In our study, in the urine analysis of the patients we did not found any spermatozoa as supported by studies conducted by Menendez V, et al.11 and Avasthi A, et al.22 Occasionally patient had oxaluria as supported by study conducted by Behere PB, et al.23 while some studies11,22 have reported no oxaluria. Various treatment strategies have been recommended with varying results in the literature. Avasthi A, et al.24 had advised a standardized treatment protocol that mainly includes sex education, biofeedback and relaxation exercises. Bhatia, et al.25 obtained the best result using tranquillizers, Menendez V, et al11 have reported best results using multivitamin, Wigg NN, et al.26 recommended proper counseling along with placebo, anti-anxiety and antidepressant drugs as required while Avasthi A, et al.27 recommend sex education and relaxation exercises.
Our study clearly showed excellent results by the approach of emphatic listening, correction of misconceptions, sex education and reassurance. There is dramatic improvement in the lifestyle of the patients.
CONCLUSION
Dhat syndrome, a culture bound disorder is still prevalent in a large section of our society particularly rural, young, lower economic strata men. The mental conditioning of semen as a very precious fluid and its perceived loss has led to very significant impact on quality of life of such individuals. Reassurance, sex education, counseling supplemented by anti-anxiety/ anti-depressants help majority of men to improve. The study also highlights the necessity of sex education, as evident by its (Dhat syndrome) presence in literate men as well, to be incorporated in the school curriculum to clear various myths and misconceptions still prevalent in some sections of the society.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.