INTRODUTION
Polyarteritis nodosa is a systemic vasculitis that involves small and medium-sized arteries. Cutaneous polyarteritis nodosa (PNC) is a rarer variant of classic polyarteritis nodosa that presents with tender subcutaneous nodules, articular involvement, myalgia and peripheric neurological involvement.1,2
Cutaneous polyarteritis nodosa (CPN) is unknown, however, the involvement of streptococcal infection and hepatitis virus infection has been suggested. The diagnosis is based on the following criteria: vasculitis limited to the skin, histopathological findings of polyarteritis nodosa and absence of systemic involvement.3,4
CASE REPORT
A 41-year-old male patient presented with fever and history of myalgia of the scapular and pelvic girdle, purple reticulated net-like lesions in the upper and lower region, torso and hands compatible with livedo reticularis, major weight bearing joints arthritis (right knee, left shoulder and proximal interphalangeal joints) and paraesthesia. The patient had no significant past medical history, no medication, alcohol or tobacco consumption, no history of high risk sexual behaviours and no common contact with animals.
Laboratory workup, complete blood count, liver and kidney function tests and urinalysis, were within normal ranges, except for elevated acute phase reactants, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Comprehensive infectious work-up was negative. Autoantibodies, including anti-nuclear antibodies (ANA), anti-double-stranded deoxyribonucleic acid (DNA) antibodies (anti-DNAds), and rheumatoid factor, were negative. Complement factors, creatine kinase (CK) and aldolase were normal. Anti-neutrophil cytoplasmic (pANCA and c-ANCA), antimyelperoxidase (anti-MPO) and anti-proteinase 3 antibodies (antiPR3), anti-Saccharomyces cerevisiae antibodies and antiphospholipid antibodies were all negative. Immunoglobulin profile was normal. Hepatitis virus, human immunodeficiency virus (HIV), syphilis, cytomegalovirus (CMV), Borrelia burgdorferi, rickettsia coronii, echovirus, A19 and B coxsackie and B19 parvovirus antibodies were negative. Culture of pharyngeal exudate and urine culture test were normal. Antistreptolysin O (ASO) test was negative, which ruled out infection by Streptococcus. The ultrasonography of the abdomen and the chest X-ray were normal. Pulmonary function tests were normal, despite showing a low diffusing capacity of lung for carbon monoxide. The high resolution computerized axial tomography (HRCT) was also normal which excluded pulmonary involvement. An electromyography test displays sensory axonal polyneuropathy in lower members.
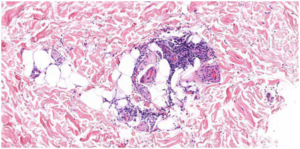
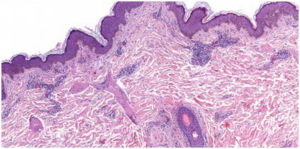
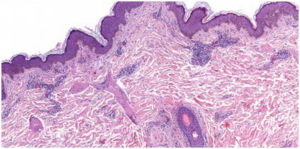
A skin biopsy is conducted, showing fibrinoid necrosis of the medium-sized artery with surrounding neutrophilic infiltrate in the subcutis, as well as in smaller vessels compatible with polyarteritis nodosa (Figures 1 and 2). Direct immune fluorescence (DIF) showed fibrinogen deposits on the walls of the blood vessels throughout the dermis and subcutis.
Figure 1. Nervous Involvement in Skin Biopsy
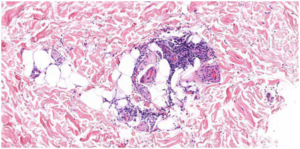
Figure 2. Neutrophilic Infiltrate in Subcutis
Based on the patient’s medical history, biopsy and imaging results and pulmonary function tests, systemic involvement was ruled out and the patient was diagnosed with cutaneous polyarteritis nodosa (CPAN).
The patient was started on prednisolone 40 mg dose with tapering doses, showing visible improvement of skin lesions and arthritis and reduction of raised acute-phase reactants. Tapering beyond 20 mg daily without was not possible which motivated treatment with immunosuppressive therapies, including azathioprine and methotrexate, however, no improvement was noted. Induction treatment with rituximab was administered for 4-weeks, showing rapid and complete resolution of symptoms and skin lesions.
DISCUSSION
Polyarteritis nodosa is a vasculitis of small and medium vessels.2 The cutaneous form does not associate multiorgan involvement and has a favourable prognosis. It is more frequently associated with paediatric patients and may be associated with infections, autoimmune diseases and pharmacological treatment.5
Our patient presented a cutaneous form of polyarteritis nodosa, evidenced by lesions compatible with livedo reticularis, myalgia, arthralgia and peripheral neurological involvement and the absence of systemic involvement. It is important to rule out systemic involvement (gastrointestinal, renal, pneumological, neurological, cardiac and vascular) in order to make a differential diagnosis with polyarteritis nodosa.
While under treatment with corticosteroids, the patient showed a good clinical and analytical response. However, recently he again presented arthralgias and new skin lesions, which is why we decided to start biological agents.
Rituximab is a monoclonal antibody against CD20 used in ANCA-associated vasculitis that compared to other immunosuppressive agents has better remission rates and a lower adverse effect risk.6
The progression of cases of cutaneous nodular polyarteritis to a systemic form of the disease is uncommon; however, there are studies that, after years of evolution, are possible. For this reason, it is essential to monitor patients.2
CONCLUSION
We hereby present a case of cutaneous polyarteritis nodosa in an adult patient. Diagnosis of PNC may be challenging as it may share similarities with polyarteritis nodosa. Most cases respond to treatment with corticosteroids, however, few cases relapse after tapering doses and require immunosuppressive agents and biologic therapy.
RHEUMATOLOGY KEYNOTES
• CPAN is a rare and benign cutaneous vasculitis of unknown ethology with chronic and relapsing course distinct from systemic PAN
• The diagnosis of CPAN is confirmed by histopathologic examination of skin biopsy.
• Treatment with corticosteroids is effective but there are cases of corticosteroid resistant or corticosteroid dependent that require immunosuppressive agents or biologic therapy
ACKNOWLEDGEMENTS
The authors acknowledge the assistance of study participant, radiographers, study nurses and laboratory staff who participated in the study. The study was conducted without any financial support.
CONSENT
Patient consent was given with purposes of writing this article.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.