INTRODUCTION
Tobacco was introduced to India by the Portuguese ~ 400 years ago, rapidly grew as a part of socio cultural milieu in various communities. India currently is the second largest producer and consumer of tobacco in the world, after China.1 Tobacco kills up to half of its users.2 The tobacco epidemic has been one of the biggest public health threats to the world killing more than 7 million people a year. Of the 1.1 billion people who smoke globally about 182 million (16.6%) live in India.3 According to the Global Adult Tobacco Survey (GATS) 48% males and 20% females in India use tobacco.4 It is predicted that tobacco will account for about 13% of all deaths in India by 2020.5
The World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC) is the world’s first public health treaty on tobacco control. India has ratified FCTC in 2004. The WHO FCTC encourages countries to improve and implement action plans to include public policies, such as bans on direct and indirect advertising of tobacco, rise in tobacco tax and its’ rates, promotion of smoke-free public places and workplaces and placing health related warning labels on tobacco packaging. The WHO FCTC also encourages countries to set up surveillance systems in order to explore the distribution of the magnitude, determinants, patterns and consequences of tobacco consumption and exposure to tobacco smoke warning labels on tobacco packaging.6
India is a major stakeholder in global tobacco control activities. The country has taken several initiatives for tobacco control including legislative measures, ratification of the WHO FCTC and implementation of the National Tobacco Control Programme. India enacted various tobacco control measures in response to growing evidence of harmful and hazardous effects of tobacco.7 In order to strengthen the tobacco control activities in India, the Government of India passed the India Cigarettes and Other Tobacco Products Act (COTPA) in 2003. The COTPA included many tobacco control provisions like prohibition of smoking in public places, prohibition of direct or indirect advertising of cigarettes and other tobacco products on billboards and in all media excluding at the point of sale. It also included prohibition of sale of tobacco products to minors and sale within a radius of 100 yards of any educational institution. It also emphasized on mandatory display of pictorial health warnings on tobacco product packages.8
During 2005 a ban on display of tobacco products, restrictions on point-of-sale advertisements and ban on vending machines sale were introduced. During 2008-2009, Cigarettes and other Tobacco Products (Packaging and Labelling) Amendment Rules, were implemented to ensure the display of health message “tobacco causes cancer”, along with one of the specified warning images for all tobacco packages (including cigarettes, cigars, cheroots, bidis, pipe, hookah, chewing tobacco, snuff, and paan masala) with text warning “SMOKING KILLS” for smoked tobacco products and “TOBACCO KILLS’’ for smokeless tobacco products respectively. Bidis taxed at 9% and cigarettes taxed at 38% of price. Ban on smoking in public places and hotels, restaurants and airports can have designated smoking areas introduced. Ban on sale of tobacco products near educational institutions introduced. In December 2010, new pictorial warnings mandated for all tobacco products and amended to the rotation period of two years for the specified health warnings. Ban on foreign direct investment for manufacturing tobacco products introduced. In 2011, round 2 of pictorial warnings was mandated for all tobacco packages four new pictorial warnings were specified for smoked and smokeless tobacco products. Ban on sale of tobacco products in plastic pouches introduced. Round 3 pictorial warnings were mandated for all tobacco packages in 2013. Three new pictorial warnings were specified for smoked and smokeless tobacco products. The word “WARNING” appeared in red font above the text of the health-warning message. A ban on sale, manufacture, and storage of gutka and pan masala introduced. In 2014 specific rates of excise duty increases on cigarettes in the range of 13% to 94%, excluding ‘other’ types of cigarettes which did not change between 2013 and 2014. Two cigarette price tires ‘filter exceeding 75 but not exceeding 85’ and ‘other’ merged into one tier ‘other’. In April, 2015, round 4 of pictorial warnings were mandated for all tobacco packages. Pictorial warnings were required to cover 60% of the package and text warnings to cover 25% of the package. Excise duty increases on cigarettes, cigars, cheroots and cigarillos in the range of 17% to 29% introduced.
The Global Youth Tobacco Survey (GYTS) was developed as a part of the Tobacco Surveillance System (GTSS)9 to monitor tobacco use among school going children aged 13-15 years using standard protocol so that results will be comparable with any geographic part of the country or the world or overtime in the same geographic location.
Adolescents is a vulnerable group, usually get exposed to tobacco and tobacco related habits very early. The age of initiation of tobacco related habit has a direct influence on the survival and related diseases in the individuals.10 The current study to the best of our knowledge is the first attempt which compares GYTS in the state of Maharashtra conducted before (in 2000) and after (in 2015) COTPA implementation of various aspects related to tobacco, such as prevalence, knowledge, attitude, policy compliance in adolescent population. Study Procedures to conduct GYTS 2000 was approved by ethics committee of Tata Memorial Hospital and GYTS 2015 by ethics committee of Healis-Sekhsaria Institute for Public Health.
MATERIALS AND METHODS
GYTS a school-based survey of students in grades 8, 9 and 10 was administered according to the standard GYTS methodology.9 In 2000 the survey was self-administered using questionnaires on paper and responses were recorded on optically readable answer sheets. While in 2015, the survey was self-administered using electronic tablets. All government and government-aided schools (~11,000 in 2000 and 15,940 in 2015) in Maharashtra were included in the sampling frame. The number of students, enrolled in grades 8, 9 and 10 in each school were obtained from the Department of Education, Maharashtra. A two-stage cluster sample design was used. At the first stage, schools (51 in 2000 and 26 in 2015) were selected with probability proportional to enrollment size. At the second stage, from the selected schools classes were selected using pre-selected random numbers. All the students in the selected classes were eligible to participate, allowing for anonymous and voluntary participation of students present on the day of the survey (2256 in 2000 and 1610 in 2015). Both the surveys were selfadministered in the classroom and took around 45 to 60 minutes, including introduction to the survey tools to the participants. All the selected schools received instructions from department of education prior to study field interviewer’s visit to selected schools.
For India the core GYTS questionnaire was suitably adopted to include tobacco use in the forms of bidi smoking and smokeless tobacco use. Same set of questions were use in both surveys and questionnaires translated into Marathi. All questions required answering (i.e. there was no skipping or branching pattern). The questionnaire was self-administered in classrooms with no identification information collected (name of student, class or school), maintaining complete anonymity. For statistical data analysis SPSS version 20.0 was used. Descriptive data by gender of the respondents were presented in tables. However, Odds Ratios (ORs) and 95% confidence intervals (CIs) was calculated for all respondents adjusted for age and gender. For multivariate analysis, survey respondent in year 2000 coded as “0” and in year 2015 as “1” included as dependent variable. While, other variables presented in rows included as independent variables. More details on India questionnaires and methodology is publish elsewhere.10,11
RESULTS
In this study, GYTS 2000 represents data before COTPA implementation and GYTS 2015 represents data after COTPA implementation for the state of Maharashtra. Gender information was missing for 133 records in 2000 survey data and 6 records in 2015, therefore excluded from the data analysis.
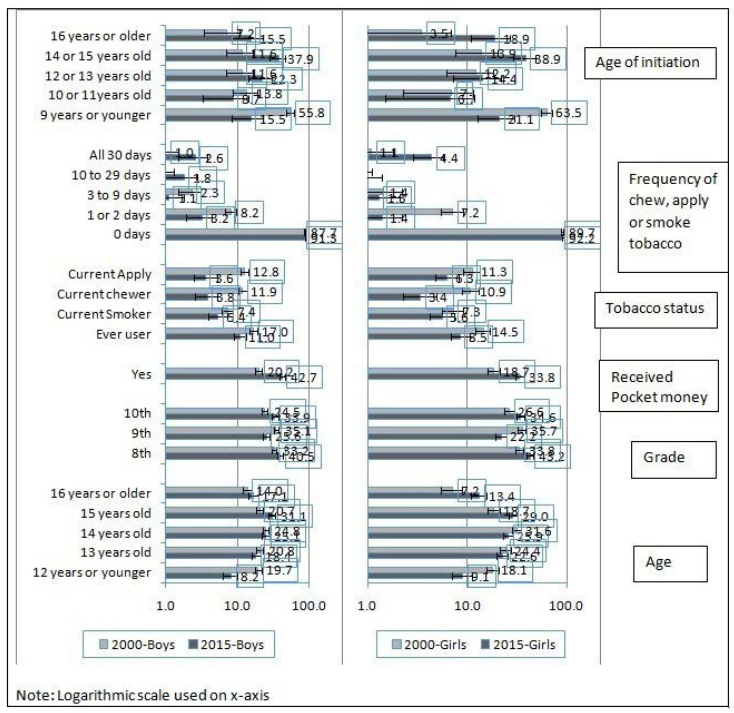
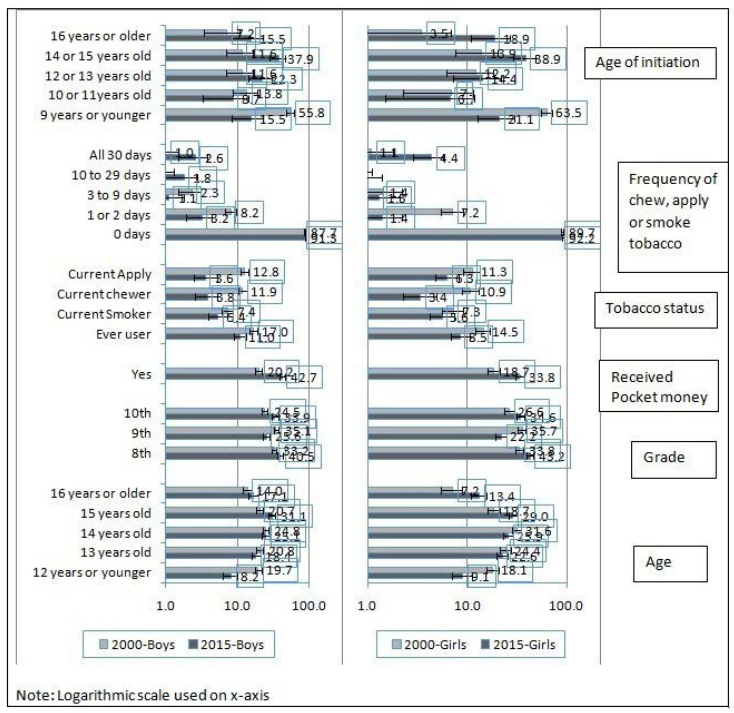
On comparison of GYTS 2000 and 2015 data (Figure 1), the prevalence of ever tobacco use has reduced from 17% (95% CIs; 14.9 to 19) to 11% (95% CIs; 9 to 13.4) among boys and from 14.5% (% CIs; 12.1 to 16.9) to 8.5% (95% CIs; 6.8 to 10.7) among girls. The age of tobacco initiation has also shifted from 11 years or younger (~70%) in 2000 to older than 11 years (~70%) in 2015. In GYTS 2015, 3.8% (95% CIs; 2.6 to 5.3) boys and 3.4% (95% CIs; 2.3 to 4.9) girls reported to have been currently chewing tobacco as compared to 11.9% (95% CIs; 10.2 to 13.7) boys and 10.9% (95% CIs; 8.8 to 13) girls in 2000. Similarly, 3.6% (95% CIs; 2.5 to 5.2) boys and 6.3% (95% CIs; 4.8 to 8.2) girls in 2015 reported of currently applying tobacco as compared to 12.8% (95% CIs; 11 to 14.6) boys and 11.3% (95% CIs; 9.2 to 13.5) girls in 2000. Even though overall current tobacco use in any form during past 30 days shows decline, daily (all 30 days) tobacco use shows an increase from 1% (95% CIs; 0.5 to 1.5) to 2.6% (95% CIs; 1.5 to 3.8) for boys and 1.1% (95% CIs; 0.4 to 1.8) to 4.4% (95% CIs; 2.9 to 5.8) for girls between 2000 and 2015 surveys respectively. Overall proportion of students receiving pocket money increased from 20.2% for boys and 18.7% for girls in 2000 to 42.7% for boys and 33.8% for girls in 2015.
Figure 1. Sample Characteristics of Youth and Their Tobacco Use, Maharashtra GYTS 2000 & 2015
Compared to 2000 survey responses (Table 1), in 2015 survey ~30% lower second hand tobacco smoke exposure at home and ~20% lower at places other than home was reported by students. Between 2000 and 2015 surveys, student reporting their both parents using tobacco (OR=0.36), only mother (OR=0.47) and only father (OR=0.71) using tobacco has decreased. In contrast, between 2000 and 2015 surveys, students reporting some of their closest friends chew or apply tobacco, has increased (OR=1.59). However, in both the surveys around 85% boys and 90% girls said that they would definitely refuse chewing or applying tobacco if offered by their best friends. Compare to 2000 survey responses ~20% lower number of students in 2015 survey thought that smoking was definitely not harmful to their health. Similarly, in 2015 twice (OR=1.97) the number of students than in 2000 survey reported that smoking for a year or two as long as you can stop was definitely not safe.
| Table 1. Harms of Tobacco Use & Exposure from Other Tobacco Use among Youth, Maharashtra GYTS 2000 & 2015 |
| Options |
Year 2000 |
Year 2015 |
Odds Ratios* & 95%CI |
| Boys (1357) |
Girls (866) |
Boys (788) |
Girls (816) |
| n |
% |
95% CI |
n |
% |
95% CI |
n |
% |
95% CI |
n |
% |
95% CI |
| $Do your parents smoke, chew or apply tobacco? |
| None |
726 |
54.2 |
(51.6, 56.9) |
478 |
56.1 |
(52.8, 59.8) |
468 |
59.6 |
(56.2, 63.0) |
543 |
67.4 |
(64.1, 70.5) |
1 |
| Both |
124 |
9.3 |
(7.7, 10.8) |
108 |
12.7 |
(10.4, 14.9) |
35 |
4.5 |
(3.2, 6.1) |
41 |
5.1 |
(3.8, 6.8) |
0.36 (0.27, 0.48) |
| Father only |
405 |
30.2 |
(27.8, 32.7) |
219 |
25.7 |
(22.8, 28.6) |
229 |
29.2 |
(26.1, 32.5) |
163 |
20.2 |
(17.6, 23.1) |
0.71 (0.61, 0.83) |
| Mother only |
43 |
3.2 |
(2.3, 4.2) |
29 |
3.4 |
(2.2, 4.6) |
13 |
1.7 |
(1.0, 2.8) |
18 |
2.2 |
(1.4, 3.5) |
0.47 (0.30, 0.74) |
| My Guardians |
|
|
|
|
|
|
14 |
1.8 |
(1.1, 3.0) |
12 |
1.5 |
(0.9, 2.3) |
– |
| I don’t know |
41 |
3.1 |
(2.1, 4.0) |
18 |
2.1 |
(1.1, 3.1) |
26 |
3.3 |
(2.3, 4.8) |
29 |
3.6 |
(2.5, 5.1) |
– |
| $If one of your best friends offered you a cigarette or a bidi or chewing tobacco, would you take it? |
| Definitely not+ |
1140 |
84.5 |
(82.6, 86.4) |
763 |
89 |
(86.9, 91.1) |
664 |
85.1 |
(82.5, 87.5) |
712 |
87.9 |
(85.5, 90.0) |
0.90 (0.74, 1.09) |
| $Do any of your closest friends chew or apply tobacco? |
| None of them |
908 |
68.6 |
(66.1, 76.1) |
705 |
82.7 |
(78.2, 83.5) |
604 |
77.4 |
(74.4, 80.2) |
741 |
92 |
(90.0, 93.7) |
1 |
| Some of them |
101 |
7.6 |
(6.2, 9.1) |
74 |
8.7 |
(6.8, 10.6) |
153 |
19.6 |
(17.0, 22.6) |
43 |
5.3 |
(4.0, 7.1) |
1.59 (1.26, 2.00) |
| Most of them |
298 |
22.5 |
(20.3, 24.8) |
59 |
6.9 |
(5.2, 8.6) |
15 |
1.9 |
(1.2, 3.1) |
15 |
1.9 |
(1.1, 3.1) |
0.11 (0.07, 0.16) |
| All of them |
16 |
1.2 |
(0.6, 1.8) |
14 |
1.6 |
(0.8, 2.5) |
8 |
1 |
(0.5, 2.0) |
6 |
0.7 |
(0.3, 1.6) |
0.65 (0.34, 1.26) |
| $Do you think smoking is harmful to your health? |
| Definitely not+ |
395 |
29.4 |
(27.0, 31.8) |
212 |
24.7 |
(21.8, 27.6) |
174 |
22.3 |
(19.5, 25.3) |
171 |
21.3 |
(18.6, 24.3) |
0.81 (0.70, 0.95) |
| $Do you think it is safe to smoke for only a year or two as long as you stop after that? |
| Definitely not+ |
649 |
48.8 |
(45.8, 51.1) |
361 |
42.2 |
(38.9, 45.5) |
475 |
61.1 |
(57.6, 64.4) |
486 |
60.4 |
(57.0, 63.8) |
1.97 (1.72, 2.26) |
| $Do you think the smoke from other people’s cigarettes or bidis is harmful to you? |
| Definitely not+ |
267 |
20.3 |
(18.1, 22.4) |
171 |
20.2 |
(17.5, 22.9) |
142 |
18.1 |
(15.6, 21.0) |
129 |
16.1 |
(13.7, 18.8) |
0.94 (0.79, 1.12) |
| $During the past 7 days (one week), on how many days have people smoked in your home, in your presence? |
| 0 days |
891 |
66.7 |
(64.2, 69.3) |
637 |
74.2 |
(71.2, 77.1) |
604 |
77.4 |
(74.4, 80.2) |
633 |
78.8 |
(75.9, 81.5) |
1 |
| 1 to 2 days |
203 |
15.2 |
(13.3, 17.1) |
124 |
14.4 |
(12.1, 16.8) |
85 |
10.9 |
(8.9, 13.3) |
55 |
6.8 |
(5.3, 8.8) |
0.54 (0.43, 0.67) |
| 3 to 6 days |
113 |
8.5 |
(7.0, 10.0) |
41 |
4.8 |
(3.3, 6.2) |
34 |
4.4 |
(3.1, 6.0) |
40 |
5 |
(3.7, 6.7) |
0.64 (0.47, 0.86) |
| 7 days |
128 |
9.6 |
(8.0, 11.2) |
57 |
6.6 |
(5.0, 8.3) |
57 |
7.3 |
(5.7, 9.4) |
75 |
9.3 |
(7.5, 11.6) |
0.85 (0.67, 1.08) |
| $During the past 7 days (one week), on how many days have people smoked in your presence, in places other than home? |
| 0 days |
711 |
53.3 |
(50.6, 56.0) |
562 |
66.1 |
(62.9, 69.3) |
474 |
60.8 |
(57.3, 64.1) |
535 |
66.7 |
63.4, 69.9) |
1 |
| 1 to 2 days |
283 |
21.2 |
(19.0, 23.4) |
161 |
18.9 |
(16.3, 21.6) |
152 |
19.5 |
(16.9, 22.4) |
131 |
16.3 |
(13.9, 19.1) |
0.82 (0.69, 0.98) |
| 3 to 6 days |
169 |
12.7 |
(10.9, 14.5) |
68 |
8 |
(6.2, 9.8) |
80 |
10.3 |
(8.3, 12.6) |
69 |
8.6 |
(6.9, 10.7) |
0.84 (0.67, 1.05) |
| 7 days |
171 |
12.8 |
(11.0, 14.6) |
59 |
6.9 |
(5.2, 8.6) |
74 |
9.5 |
(7.6, 11.8) |
67 |
8.4 |
(6.6, 10.5) |
0.79 (0.63, 1.00) |
| Note: OR= Odds ratios, CI=Confidence interval, NA=not applicable. *year of survey was used as dependent variable with year 2000 coded as 0 & year 2015 was coded as 1 and adjusted for age and sex. +reference category used as sum of probably not, probably yes and definitely yes. $Totals may not add up due to inclusion of only valid cases. |
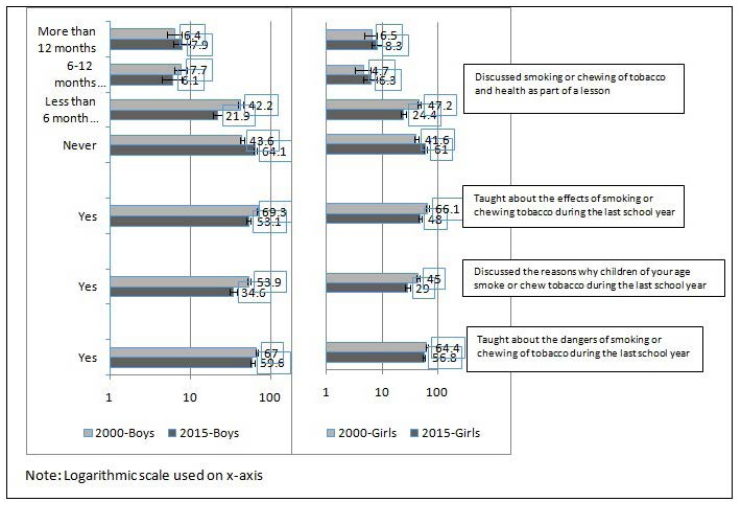
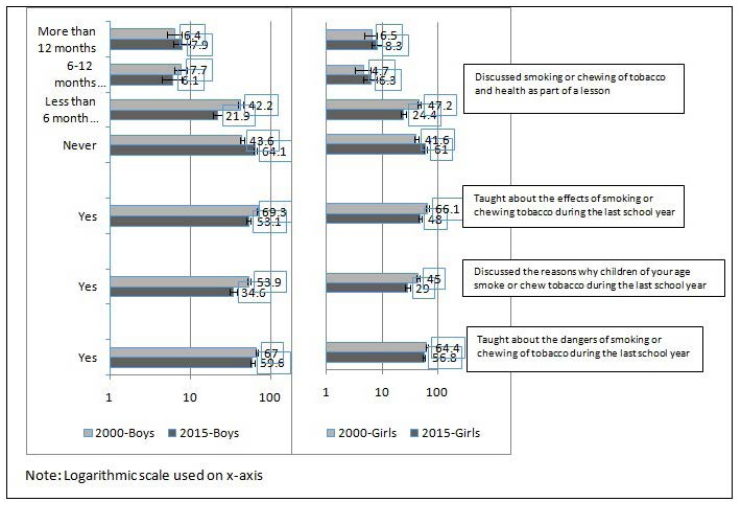
Decrease was observed between 2000 and 2015 surveys (Figure 2), in any teaching about the dangers of smoking/chewing in their school [boys 67% (95% CIs; 64.4 to 69.5) v/s 59.6% (95% CIs; 56.2 to 63) and girls 64.4% (95% CIs; 61.2 to 67.6) v/s 56.8% (95% CIs; 53.3 to 60.1)], any discussions on why children of their age smoke/chew [(boys 53.9% (95% CIs; 51.2 to 56.6) v/s 34.6% (95% CIs; 31.3 to 38) and girls 45% (95% CIs; 41.6 to 48.4) v/s 29% (95% CIs; 26 to 32.3)] and any teaching about effects of smoking/chewing in previous year of school [(boys 69.3% (95% CIs; 66.8 to 71.7) v/s 53.1% (95% CIs; 49.6 to 56.6) and girls 66.1% (95% CIs; 62.9 to 69.3) v/s 48% (95% CIs; 44.6 to 51.4)]. Similarly, between 2000 and 2015 surveys (Table 2), 60% decrease reported by students in families discussing about the harmful effects of tobacco.
Figure 2. Tobacco in school curriculum, Maharashtra GYTS 2000 & 2015
| Table 2. Perception And Attitude Towards Tobacco Use among Youth, Maharashtra GYTS 2000 & 2015 |
| Options |
Year 2000 |
Year 2015 |
Odds Ratios* & 95%CI |
| Boys (1357) |
Girls (866) |
Boys (788) |
Girls (816) |
| n |
% |
95% CI |
n |
% |
95% CI |
n |
% |
95% CI |
n |
% |
95% CI |
| $During the past 30 days, did anyone ever refuse to sell you cigarettes because of your age? |
| Yes |
121 |
76.1 |
(69.5, 82.7) |
72 |
84.7 |
(77.1, 92.4) |
54 |
56.3 |
(46.3, 66.2) |
45 |
55.6 |
(44.7, 66.4) |
1 |
| No |
38 |
23.9 |
(17.3, 30.5) |
13 |
15.3 |
(7.6, 22.9) |
42 |
43.8 |
(33.8, 53.7) |
36 |
44.4 |
(33.6, 55.3) |
2.82 (1.79, 4.44) |
| $During the past 30 days, did anyone ever refuse to sell you bidi /any other smoking tobacco product because of your age? |
| Yes |
97 |
78.9 |
(71.6, 86.1) |
71 |
86.6 |
(79.2, 94.0) |
59 |
61.5 |
(51.7, 71.2) |
51 |
62.2 |
(51.7, 72.7) |
1 |
| No |
26 |
21.1 |
(13.9, 28.4) |
11 |
13.4 |
(6.0, 20.8) |
37 |
38.5 |
(28.8, 48.3) |
31 |
37.8 |
(27.3, 48.3) |
3.03 (1.83, 5.00) |
| $Has anyone in your family discussed the harmful effects of smoking or chewing tobacco with you? |
| Yes |
944 |
71.2 |
(68.8, 73.6) |
563 |
66.6 |
(63.4, 9.8) |
374 |
47.7 |
(44.2, 51.2) |
385 |
47.8 |
(44.4, 51.3) |
0.39 (0.34, 0.45) |
| $At any time during the next 12 months (one year), do you think you will smoke a cigarette or a bidi or chew a tobacco product? |
| Definitely not+ |
1128 |
84.6 |
(82.7, 86.6) |
761 |
89.3 |
(87.2, 91.4) |
650 |
83.1 |
(80.3, 85.6) |
711 |
88 |
(85.6, 90.1) |
0.81 (0.67, 0.98) |
| $When you watch TV, videos, or movies, how often do you see actors smoking? |
| Never |
92 |
6.9 |
(5.6, 8.3) |
58 |
6.9 |
(5.2, 8.6) |
75 |
9.5 |
(7.7, 11.8) |
115 |
14.3 |
(12.1, 16.9) |
1 |
| A lot |
552 |
41.6 |
(38.9, 44.2) |
372 |
44.3 |
(41.0, 47.7) |
258 |
32.8 |
(29.6, 36.2) |
245 |
30.5 |
(27.4, 33.8) |
0.42 (0.33, 0.54) |
| Sometimes |
404 |
30.4 |
(27.9, 32.9) |
255 |
30.4 |
(27.3, 33.5) |
278 |
35.4 |
(32.1, 38.8) |
299 |
37.2 |
(34.0, 40.6) |
0.68 (0.53, 0.88) |
| I never watch TV, videos, or movies |
280 |
21.1 |
(18.9, 23.3) |
154 |
18.4 |
(15.7, 21.0) |
175 |
22.3 |
(19.5, 25.3) |
144 |
17.9 |
(15.4, 20.7) |
– |
| $When you watch TV, videos, or movies, how often do you see actors chewing tobacco? |
| Never |
155 |
11.6 |
(9.9, 13.3) |
103 |
12.1 |
(9.9, 14.3) |
126 |
16.1 |
(13.7, 18.9) |
154 |
19.1 |
(16.5, 22.0) |
1 |
| A lot |
398 |
29.9 |
(27.4, 32.3) |
306 |
35.9 |
(32.7, 39.1) |
199 |
25.5 |
(22.6, 28.7) |
190 |
23.6 |
(20.8, 26.6) |
0.51 (0.41, 0.63) |
| Sometimes |
480 |
36 |
(33.4, 38.6) |
286 |
33.6 |
(30.4, 36.7) |
294 |
37.6 |
(34.3, 41.1) |
316 |
39.2 |
(35.9, 42.6) |
0.72 (0.58, 0.88) |
| I never watch TV, videos, or movies |
300 |
22.5 |
(20.3, 24.7) |
157 |
18.4 |
(15.8, 21.0) |
162 |
20.7 |
(18.0, 23.7) |
146 |
18.1 |
(15.6, 20.9) |
– |
| $Has a cigarette company person or cigarette vendor ever offered you a free cigarette? |
| Yes |
214 |
16.6 |
(14.6, 18.6) |
83 |
10 |
(8.0, 12.0) |
57 |
7.3 |
(5.7, 9.3) |
37 |
4.6 |
(3.4, 6.3) |
0.54 (0.42, 0.70) |
| $Has a bidi company person or bidi vendor ever offered you a free bidi? |
| Yes |
203 |
16 |
(14.0, 18.0) |
91 |
11 |
(8.9, 13.2) |
56 |
7.1 |
(5.5, 9.2) |
30 |
3.7 |
(2.6, 5.3) |
0.47 (0.36, 0.61) |
| $Has a gutka or pan masala company person or vendor ever offered you a free sample? |
| Yes |
225 |
17.3 |
(15.2, 19.3) |
106 |
12.6 |
(10.4, 14.9) |
55 |
7 |
(5.4, 9.0) |
25 |
3.1 |
(2.1, 4.6) |
0.39 (0.30, 0.52) |
| Note: OR= Odds ratios, CI=Confidence interval, NA=not applicable. *year of survey was used as dependent variable with year 2000 coded as 0 & year 2015 was coded as 1 and adjusted for age and sex. +reference category used as sum of probably not, probably yes and definitely yes. $Totals may not add up due to inclusion of only valid cases. |
Between 2000 and 2015 surveys (Table 2), decrease was also observed in the distribution of free cigarettes (OR=0.54) or bidis (OR=0.47) or gutka/pan masala (OR=0.39) by company persons/vendors. Among the students who watched TV or videos or movies, less students reported seeing actors smoking (OR=0.42) or chewing (OR=0.51) a lot on screen, in 2015 than in 2000. In contrast, students who attempted to buy cigarettes (OR=2.82), bidis or other smoking products (OR=3.03) who were not refused tobacco products because of their age has increased threefold between 2000 and 2015 surveys.
In 2015 (Supplementary Table 1), more boys than girls were aware about the ban on sale of gutka, ban on sale of flavored tobacco and ban on sale of pan masala or flavored areca nut. About 51% boys and 41% girls reported seeing shops selling tobacco products near their schools. Even though 41% boys and 32% girls observed boards prohibiting the sale of tobacco products to minors at tobacco shops, 49% boys and 35% girls have observed people of their age not only buying tobacco but 41% boys and 26% girls even selling tobacco products. About 36% boys and 27% girls observed pictorial health warnings only on cigarettes packets, 4.7% boys and 3% girls observed only on bidis packets, 6.9% boys and 7.2% girls only on chewing packets and 24.1% boys and 18.8% girls have observed pictorial warnings on both smoke and chewing tobacco packets. Interestingly, 10% boys and 13% girls who use tobacco reported never observing pictorial health warnings on tobacco products.
| Supplementary Table 1. COTPA Compliance among Youth, Maharashtra GYTS 2015 |
| Questions |
Options |
Year 2015 |
| Boys (N=788) |
Girls (N=816) |
| n |
% |
95% CI |
n |
% |
95% CI |
| $Do you want to stop tobacco use now?
|
I do not use any tobacco now |
25 |
16.7 |
(10.7, 22.6) |
27 |
13.8 |
(9.0, 18.7) |
| Yes |
109 |
72.7 |
(65.5, 79.8) |
160 |
82.1 |
(76.7, 87.4) |
| No |
16 |
10.7 |
(5.7, 15.6) |
8 |
4.1 |
(1.3, 6.9) |
| Do you think the sale of gutka is banned in Maharashtra? |
Yes |
323 |
41.2 |
(37.8, 44.7) |
250 |
30.9 |
(27.8, 34.1) |
| Do you think the sale of flavoured tobacco is banned in Maharashtra? |
Yes |
287 |
36.6 |
(33.3, 40.0) |
230 |
28.4 |
(25.4, 31.6) |
| Do you think the sale of pan masala or flavoured areca nut (Supari) is banned in Maharashtra? |
Yes |
432 |
55.2 |
(51.7, 58.6) |
382 |
47.3 |
(43.9, 50.7) |
| Have you seen any shop selling tobacco products near to your school? |
Yes |
405 |
51.7 |
(48.2, 55.2) |
332 |
41.2 |
(37.8, 44.6) |
| $During the past 30 days (one month), did anyone ever refuse to sell you gutka/pan masala or any other smokeless product because of your age? |
Yes, because of age |
14 |
17.3 |
(9.0, 25.5) |
25 |
27.8 |
(18.5, 37.0) |
| Yes, because of smokeless tobacco is banned |
24 |
29.6 |
(19.7, 39.6) |
31 |
34.4 |
(24.6, 44.3) |
| No |
43 |
53.1 |
(42.2, 64.0) |
34 |
37.8 |
(27.8, 47.8) |
| Have you seen any sign boards prohibiting the sale of tobacco products to minors at the tobacco selling shops? |
Yes |
319 |
40.7 |
(37.4, 44.2) |
260 |
32.1 |
(29.0, 35.4) |
| Have you observed any one of your age selling tobacco products? |
Yes |
324 |
41.2 |
(37.8, 44.7) |
206 |
25.5 |
(22.6, 28.6) |
| Have you observed any one of your age buying tobacco products? |
Yes |
381 |
48.5 |
(45.1, 52.0) |
282 |
34.9 |
(31.7, 38.3) |
| $Do you think smoking is banned in public places like restaurants, buses, train stations, bus stations, schools, gyms and sports stadiums, etc.? |
Yes, all places |
464 |
59.2 |
(55.7, 62.6) |
390 |
48.6 |
(45.1, 52.0) |
| Yes, some of these places |
183 |
23.3 |
(20.5, 26.4) |
258 |
32.1 |
(29.0, 35.4) |
| No |
137 |
17.5 |
(14.9, 20.3) |
155 |
19.3 |
(16.7, 22.2) |
| $Have you ever objected to anyone smoking in your presence in any public places? |
Yes, always |
293 |
37.4 |
(34.1, 40.9) |
250 |
31.3 |
(28.2, 34.6) |
| Yes, sometimes |
273 |
34.9 |
(31.6, 38.3) |
273 |
34.2 |
(31.0, 37.5) |
| No, never |
162 |
20.7 |
(0.18, 23.7) |
170 |
21.3 |
(18.6, 24.3) |
| $Have you observed pictorial health warnings on tobacco products? |
Yes, only on cigarettes packets |
281 |
35.8 |
(32.6, 39.3) |
216 |
26.9 |
(23.9, 23.0) |
| Yes, only on bidi packets |
37 |
4.7 |
(3.4, 6.4) |
24 |
3.0 |
(2.0, 4.4) |
| Yes, only on chewing tobacco packets |
54 |
6.9 |
(5.3, 8.9) |
58 |
7.2 |
(5.6, 9.2) |
| Yes, both smoke and chewing tobacco packets |
189 |
24.1 |
(21.3, 27.2) |
151 |
18.8 |
(16.2, 21.6) |
| No, I never observed as I do not use any form of tobacco |
142 |
18.1 |
(15.6, 21.0) |
253 |
31.5 |
(28.4, 34.8) |
| No, even if I am a tobacco user |
81 |
10.3 |
(8.4, 12.7) |
102 |
12.7 |
(10.6, 15.2) |
| Note: CI=Confidence interval. $Totals may not add up due to inclusion of only valid cases. |
DISCUSSION
Smoking and chewing tobacco has severe influence on social,11,13,14,15,16,17,18,19,20,21,22,23,24 economic13,14,18,21,22,23,24 and health11,12,13,14,15,16,17,19,20,21,22,23,24 components of individuals. Use of tobacco exposes, both the first hand users and second hand smokers, to many harmful carcinogenic chemicals and diseases.12 Current study clearly shows, decline in overall tobacco use among boys and girls in survey conducted in 2000 (before COTPA implementation) and in 2015 (after COTPA implementation). However, as demonstrated in other states of India,13 this study also observes narrowing of the prevalence differences of tobacco use among boys (11%) and girls (8.5%) but continues to remained high among boys than girls. Smoking by girls is culturally not accepted in Indian society,10,14 and therefore; higher cigarette smoking gender differences were observed among students in most states, mainly in the northeastern states of India.10 In this study, the proportion of girls reporting smoking was almost identical to that reported by boys in both the surveys. Findings from the GYTS from 132 WHO member states shows that around half of all the students surveyed worldwide were exposed to tobacco smoke at home (36.4% in India) and outside their home (48.7% in India).15 In this study, between 2000 and 2015, decreased in the exposure to SHS 7 days prior to the survey was observed in their homes as well as outside their homes. One such study was conducted in Mumbai in 2010, found that students own tobacco use, their age, their parents tobacco use, their close friends tobacco use were associated with their exposure to second hand smoke at home and outside home.16
The family members and friends tobacco use was associated with adults17 and children’s10,14,15,18,19 tobacco use. A population base survey of high school students in Mumbai19 further delineated that both parents using tobacco increased the odds four times while any one parent using tobacco increased the odds two times that their children will also use tobacco. Even though the current study reported a decline in tobacco use by both parents but tobacco use by any one parent (father only) remained high between 2000 and 2015 surveys. Similarly, smoking acts like as a catalyst to make new friends and develop relationships.20 In this study post COTPA implementation, boys and girls reporting any of their closest friends smoke, chew or apply tobacco decreased in 2015 than it was reported in 2000.
Pocket money increases the purchasing power among the youth and is therefore, an influential factor for initiation of tobacco products.14,18 Pocket money was also associated with student’s intention to use tobacco and ease to access tobacco products.19 In this study, around two-fold increase observed in the proportion of students who receive pocket money between 2000 and 2015 surveys.
Tobacco control policies compliance decreased smoking prevalence.19,21,22,23,26,28 A policy on tobacco sale to minor was associated with lowering youth smoking.22 Although the laws clearly prohibit the sale of tobacco products to young people<18 of age in India,8 the current study shows initiation of tobacco use continues to starts as early as 9 years or younger.
However, the current study observed shift in the distribution of age of initiation of tobacco use among both boys and girls from 11 years or younger (~70%) in 2000 survey to older than 11 years (~70%) in 2015 survey. Section 6 of COTPA prohibits the sale of tobacco products to minors and near educational institutions; however, students have reported seeing people of their age not only buying but selling tobacco products as well. Sale of tobacco and related products was also observed by students near their schools. Another study conducted in Mumbai in 201223 also found that tobacco vendors were present within 100 m of nearly all sampled schools and student’s tobacco use was associated with the presence of tobacco vendors and advertisements within 100 to 500 m of schools.
Among all tobacco products, smokeless tobacco is the predominant form used by men (29.6%), women (12.8%), and youth of age 15-24 (10.8%); it exceed the prevalence of cigarette smoking and that of other smoked products (e.g., bidis).24 Section 8 of COTPA emphasizes on specific health warnings through pictorial messages on all tobacco products, tobacco industry influence led to years of delays and dilutions.25,26 The pictorial health warnings introduced in 2009 were weak, with one symbolic image that of a scorpion (which was unrelated to cancer) on 40% of the fount of the package. In December 2011, four graphic images of cancer of the mouth, jaw, or neck were replaced the scorpion image. While in 2013 three new graphics health warnings were implemented. All smokeless tobacco warnings since 2011 were accompanied by the text “Tobacco Kills”; however, size, location, the lack of rotation and freedom to tobacco industry to choose any one of the available warnings continues to dilute the impact. This study confirms low level of noticing and effectiveness reported in other Indian studies.27,28 Additionally, change from the symbolic warnings (before COTPA) to graphics health warnings (after COTPA) did not lead to increase in noticing as well as effectiveness.
Students in this study have reported around 40% decrease in the distribution of free cigarettes, bidi’s and gutka or pan masala by vendors or company persons between 2000 and 2015. Distribution of free cigarettes to minors was prohibited under COTPA but now making it a punishable offense under section 77 of the Juvenile Justice Act (Care and Protection of Children), 2015,29 will further restrict the free sample distribution in future.
Even though sale of gutka is banned in Maharashtra under the Food Safety and Standards Act (FSSA), 2012,30 similar to other studies,31,32,33 the current study highlights continuation of poor knowledge among students in relation to existing laws. The lack of knowledge about existing laws and harmful effects of tobacco was correlated well in our study with reduction in discussion about harmful effects of tobacco at home as well as in schools. As observed in other studies,15,34 academic teaching on harmful effects of tobacco, during the last school year had reduced in 2015 (59% boys v/s 56% girls) to that reported in 2000 (67% boys v/s 64% girls) Maharashtra GYTS. School tobacco control policies have shown success in delayed initiation of smoking and in reduction of smoking rates in the Western settings35 and in India.36 Thus health education and awareness with a comprehensive, evidencebased curriculum could be helpful to protect the youth from the risk of tobacco use.
STRENGTHS AND LIMITATIONS
There are several notable strengths and limitations to this study. First strength, data for this paper came from the GYTS surveillance system, which was followed globally with a standard study protocol and hence comparable within country and between countries. However, the results are generalizable mainly to school going children might be a potential limitation. This was cross-sectional survey; hence causality between exposure and outcome may not be established, might be another limitation. Also, the responses were self-reported without any biological validation of their tobacco use status and might subject to recall biases. However, such measures have been widely used and shown good validity and reliability when administered anonymously within classroom.37 Additionally, we did not asked about number of other variables that might have contributed to the low knowledge and low awareness of COTPA, such as, while responding weather they were thinking of tobacco products that were available in a packages or container, illicit products, or homemade products.
CONCLUSION
Tobacco use has decreased after implementation of COTPA in school going children of Maharashtra. Shift in the distribution of age of initiation of tobacco use needs attention of researcher and policy makers. Established factors that influence children’s tobacco use such as parents, close friends tobacco use, exposure to second hand smoke at home and outside home, pocket money received by students requires continuous monitoring. Increasing the awareness and knowledge at home and at school will further support the tobacco control efforts. Overall compliance with tobacco control laws in India needs further enforcement in order to decrease availability, accessibility, and affordability of tobacco products.
ACKNOWLEDGEMENTS
This study was funded by the Tobacco Free Initiative, WHO, Geneva and the technical assistance was provided by the Office on Smoking and Health, CDC, Atlanta, USA. The views expressed in the article, however, are those of the authors.
This manuscript work was partialy supported from NCI/ NIH grant (1R01CA201415-01A1).
We wish to thank the Government of India, Government of Maharashtra and the Ministry of Education, for their permission and administrative help for carrying out the survey. The Unit of the National Informatics Centre, India provided enrolment information. We are grateful to the students and school personnel who helped enthusiastically with this research.
We would like to thank Dr P.C Gupta for providing feedback on final version of the manuscript. We also thank Mrs. Neha Mathur, Mr. Naveen Agarwal and all the field interviewers for their valuable contribution to the study.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.