INTRODUCTION
Currently, liver cirrhosis (LC) with portal hypertension (PH) is one of the leading causes of morbidity and mortality worldwide. Due to the high incidence of viral hepatitis, as well as the steady growth of factors such as alcohol, drugs or toxic liver injury, its social importance is steadily increasing in many countries.1,2,3 Although the average age of patients with LC in Europe and the USA is 55±10 years, in Central Asian region tendency to “rejuvenation” of the disease, up to 25 years old and younger.1
Often determined by the fatal prognosis, the two main complications of LC are: bleed-ing of esophageal and gastric varices (EGV) and progression of liver failure with encephalopathy. A group at risk for potential EGV bleeding includes 20-50% of patients with PH. According to different authors, mortality associated with hemorrhagic syndrome ranges from 30% and above, and with the development of a hepatic coma, that rate rises to 80-90%.4,6
The only radical method of treatment for these patients is liver transplantation. However, liver transplantation is not only a potential possibility for radical treatment, but it is always interfaced with needs to resolve a number of difficult questions; among which are medical, social and organizational issues, both from the government point of view (juristic and legislative based), as well as from the practical health care point of view (hospital equipment, human resources, etc.).7,8 Thus, even in countries with an advanced transplantation program, liver transplantation requirements are only, on average, 25-50% met.9-11 Among the patients in the waiting list, 10-24% die before transplantation. More than a quarter of these deaths are due to esophageal and gastric varices bleeding. For this reason, prevention of complications from cirrhosis in patients with sufficient functional liver reserve is relevant.10 Such high mortality rates necessitate the implementation of interventions aimed at preventing hemorrhagic syndrome. Among these, endovascular and surgical decompression of the portal system are considered the most optimal methods.12,13
It should be noted that, currently, interest in the traditional portosystemic shunt (PSSh) method has decreased slightly. On one hand, this decrease is caused by the widespread introduction of minimally invasive techniques, among which priority is given to endovascular interventions (TIPS) and endoscopic techniques (ligation and sclerotherapy), and on the other hand, by a influence on the demand of bypass surgery, which has exerted a vast introduction of radical treatment for LC.14
Numerous studies show that for patients of Child-Pugh functional class “A” and “B”, PSSh must still be considered as an optional method for portal decompression, especially in patients with inefficient pharmacological and endoscopic treatment, and who lack the indication or possibility for liver transplantation. During indication observance, PSSh was proved to be an effective alternative to other methods, both in terms of preventing EGV bleeding as well as in the survival rate of patients with liver cirrhosis.15,16 Therefore, different variations of traditional decompressive surgery still remain as a method of choice in the leading hepatology centers worldwide.17
Thus, the development of vascular surgery for PH, both as a stage of preparation for liver transplantation, as well as a part of a possible method for preventing EGV bleeding, remains as an urgent problem to solve in modern hepatology.
MATERIALS AND METHODS
During the period from 1976 to 2015, PSSh using the traditional technique was performed on 925 patients with PH in Republican Specialized Center of Surgery (RSCS) named after academician V.Vakhidov (Tashkent, Uzbekistan). The etiological factor of PH in 867(94.3%) patients was LC, whereas in the remaining 58(5.7%) patients it was an extrahepatic form of PH. The results of 689 PSSh performed in RSCS named after academician V.Vakhidov (Tashkent. Uzbekistan) from 2001 to 2015 in patients suffering LC were analyzed.
Statistic analysis was held using MS Excel with Systat Software (USA) program software. Quantitative data was submitted as mean (M)± standard deviation (m). The significance of differences was defined according to Student criteria. Difference were defined as statistically veracious in р<0.05. Mortality analysis was measured according to Kaplan-Meier.
The average age of all patients was 28.5±0.42 years EGV bleeding occurred in 483(70.1%) patients in other cases, PSSh was performed as a prophylactic measure due to the high risk of it being developed. Different types of PSSh were performed on all patients (Table 1). Among the types of bypasses performed, distal splenorenal shunts (DSRSh or Warren shunts) were performed on the majority of cases (350). In the other 339 cases, the following central type PSSh were performed: proximal splenorenal shunt with splenectomy (PSRSh), latero-lateral splenorenal shunt (LLSRSh), splenosuprarenal shunt (SSRSh), and H-shaped splenorenal shunt (H-SRSh).
Table 1: Type of portosystemic shunt performed in patients with PH
|
Type of operation
|
LC
|
|
Number
|
%
|
|
Distal splenorenal shunt (Warren)
|
350 |
50,8% |
| Different types of central bypass |
339 |
49,2%
|
|
Total
|
689 |
100%
|
RESULTS
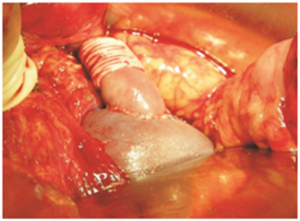
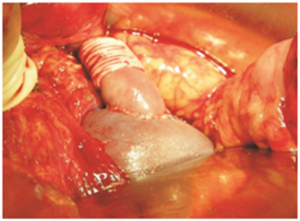
The current status of surgery for PH in Uzbekistan is characterized by an individualized approach, which aims to choose the most optimized method of preventing complications, depending on factors such as: age of patient, risk level of developing hemorrhagic syndrome, portal pool angioarchitectonics features; By putting to use the technique of portocaval decompression limiting, when forming the central type of decompression. This technique was developed in 1998 (patent №IAP03265). The essence of the developed technique is the application of a calibrated restrictive cuff (vascular prosthesis), passed on top of the anastomotic vessel, when performing termino-lateral and latero-lateral
shunting types, or on top of the insertion from the internal jugular vein (IJV), when forming H-SRSh. (Figures 1 and 2)
Figure 1: Scheme of PSSh with restrictive cuff.
Postoperative Complications
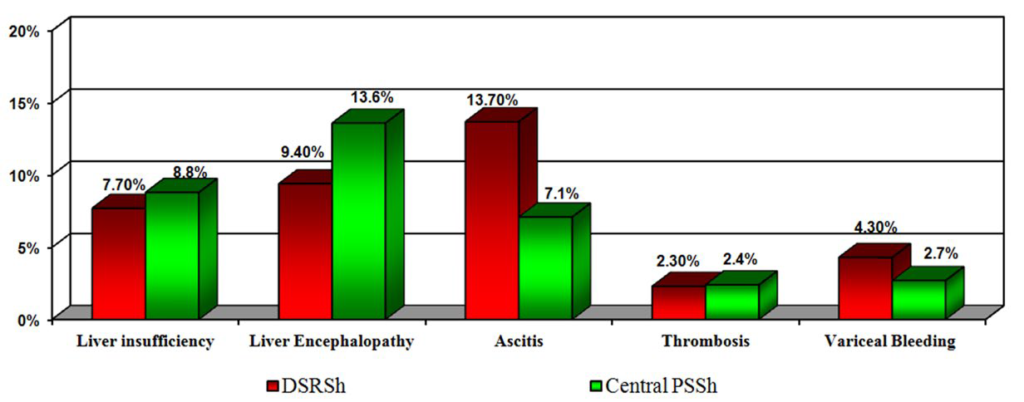
Acute liver failure (ALF) development was one of the severe post-operative complications found in patients after central PSSh was performed. If considered in chronological order, over the last 5 years of monitoring, ALF frequency decreased to 8.8% in patients with central bypass and to 7.7% in patients with Warren procedure. Before the year 2000, however, frequency of ALF ranged between 25-30%. Similar data was obtained for other post-operative complications.
Figure 2: PSSh with restrictive cuff
Hepatic encephalopathy (HE) frequency in the central anastomosis group decreased from 40% (before the year 2000) to 13.6% and in Warren procedure group (DSRSh group) from 33 down to 9.4% (Figure 3).
Figure 3: Frequency of specific complications after central and selective PSSh.
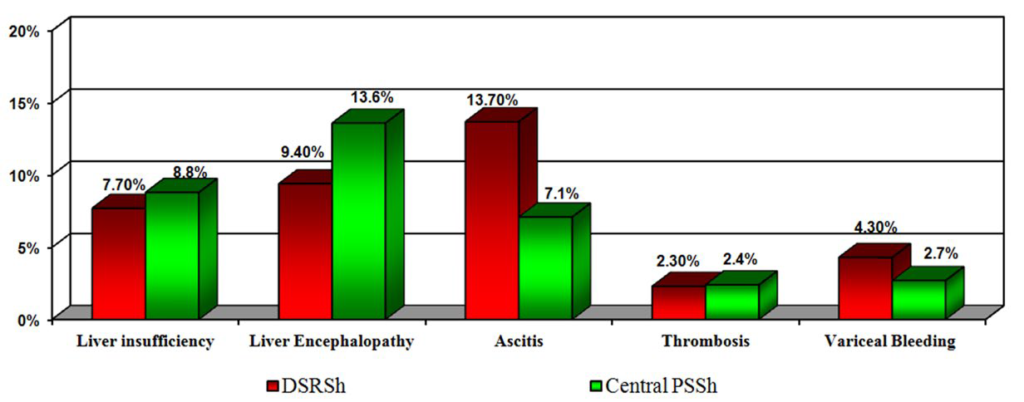
Of course, in the distant period of observation (3-5 years) mentioned complications were of fundamental importance. However, it is possible to ascertain a significant improvement in the quality of the surgical correction of PH by individual approach for bypass type and if necessary, formation of the partial discharge, which allows to preserve residual hepatofetal blood flow at an acceptable volume level. This explains the low incidence of ALF in 5 years follow-up. Also, thrombosis minemalization became possible because of the formation of a full
size anastomosis chamber and limiting of vessel diameter.
Bleeding
Endoscopy was performed on 2nd-3rd month after operation in order to evaluate the effectiveness of decompression. Regression of varicose veins was found in the majority of cases. However, within the central bypass group there was no significant difference in the decompressive effect and regression was less pronounced in patients who had undergone the Warren procedure. A good decompressive effect (varices of 1st grade and less) was observed in 75.0% of patients in the total central bypass group, and in 72.5% of patients in the partial central bypass group. Such data reveals an adequate decompression for both options. However, after the Warren procedure the rate of decompression was observed in 46.8% of patients with up to 3 months monitoring. The forementioned is possibly due to the selective decompression of the slow restructuring of portal circulation.
Mortality
With regards to mortality, acute liver failure was a major fatal complication, presenting in more than 70% of cases. In the last period of follow-up on the background of preventive bypass with preservation of hepatofetal flow, mortality rate in the immediate post-operative period decreased to 2.7% for central bypass patients and to 3.9% for selective decompression (14.8% until year 2000).
Among the factors that most significantly influenced the decline of mortality rates in cirrhotic patients with PSSh were: 1) indications and contraindications for PSSh were fundamentally reviewed, 2) partial central18 and selective19 types of anastomoses were widely introduced, 3) the original procedures of portocaval discharge limitation were introduced, 4) the number of total central anastomoses was decreased to a minimum, 5) precision surgical technology with optical amplification during vascular anastomosis formation was used, and 6) range of liver drug therapy support during the post-operative period was substantially expanded.
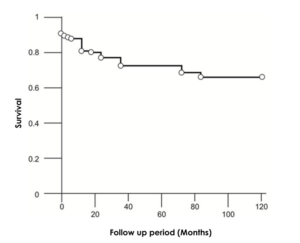
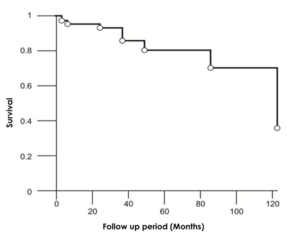
Figure 4: Survival rate after Warren procedure
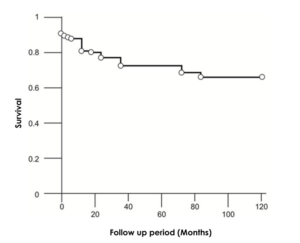
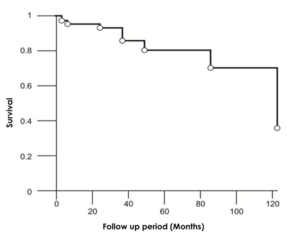
The survival analysis held in each of the stratified groups revealed general and specific (unique to a certain type of PSSh) trends in mortality. Overall survival rate of patients after Warren procedure was as follows: 87.5% for up to 1 year, 74.4% for 3 to 5 years, and 71.3% for more than 5 years (Figure4). Thus, the highest mortality rate was observed during the first three years of follow-up. Survival rates of patients after central PSSh were characterized by the absence of immediate postoperative mortality as well as the largest percentage (69%) of patients with a 10-year survival rate (Figure 5).
Figure 5: Survival rate in patients after central. PSSH.
The main cause of general postoperative mortality in the 5-years follow-up, regardless of the PSSh procedure performed, was cirrhosis activation with expansion of hepatocellular insufficiency and further decomposition of the patient? And development of the expanded hepatocellular insufficiency.
Quality of Life
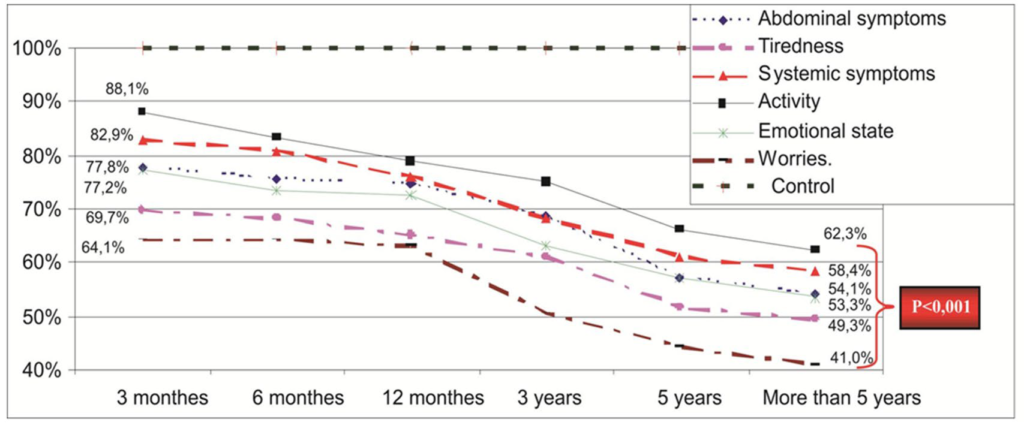
To assess “quality of life (QoL)” the chronic liver disease questionnaire (CLDQ), designed by Younossi et al20 for patients with chronic liver disease, was used. The CLDQ is the first specific document for assessing quality of life. It includes 28 items distributed by the following six domains: 1) abdominal symptoms, 2) tiredness, 3) systemic symptoms, 4) activity, 5) emotional state, and 6) worries. Answers from respondents included seven possible options ranging from “all the time” to “never”. Patients answer all questions and the middle amount of points are determined with a maximum of 196 points possible. In some domains points are defined by various questions (from 1 to 7 points). In summary, the higher the score obtained, the better the “quality of life” of the patient.
This “quality of life” analysis was performed in 248 patients with LC after PSSh. To compare the “quality of life” indicator, 50 people were included in the control group and were surveyed by the mentioned principle. It should be noted that for the purity? Of the study, the control group included healthy individuals matched for age (27.9±0.9 years), gender and location of living.
The “quality of life” analysis before and after PSSh is of particular interest. The group of 32 patients with liver cirrhosis was analyzed and their quality of life was analyzed beforeand after PSSh. Besides, all patients before PSSh, during the previous month, had a bleeding from EGV episode, which was stopped conservatively.
Results of the “quality of life” questionnaires showed that, before PSSh, indicators were significantly worse than in the periods immediately following the operation. The mean total pre-operative score was 114.1±1.4 and in the term of three months after PSSh, it increased to 127.5±1.7. The latter score significantly differed from the baseline indicator (p<0.001). The increased score observed pre- and post-PSSh was caused not only by the decompressive effect resulting from the procedure, but also by the positive emotional and psychological state of post-operational patients. Patients also paid special importance to the objective indicators of their status improvement. Regression of PH and
its complications causes not only the decrease of EGV bleeding risk, which, by itself, has a subjectively positive reflection in the neurological state of patients, but it also changes other objective criteria for assessing their own health.
In particular, the reduction or disappearance of the edematous- ascitic syndrome, which an etiologic factor was not only a protein synthetic failure of hepatocytes, but also an elevated PH. In addition, the reduction of portal pressure has a positive effect on the discomfort associated with splenomegaly syndrome, since PSSh facilitates the reduction of spleen size. Further, mean scores were examined by main domains. Within the period of up to 3 months following the procedure, the lowest scores were obtained by the following domains: “tiredness”: 4.0±0.03, “activity”: 4.4±0.03; “emotional state”: 4.2±0.03, and “nervousness”: 4.1±0.07. With all these indicators, values differed from those of the control with a high degree of accuracy (p<0.001). Subsequently, gradual, progressive deterioration of the quality of life indicators was observed in all the domains. The most pronounced deterioration was for the domains of “activity” and “emotional state”, by which, during practically all periods, the mean score worsened reliably (p<0.05- 0.001), unlike other domains, where there had been periods without considerable reduction.
Comparison with the control was more pronounced and within more than five year follow-up, accounted just for 41.0% in comparison to the control by the domain «nervousness», and maximum 62.3% – to the control by domain «activity» (Figure 6).
Figure 6: Quality of life dynamics relatively to the control group by the main domains of CLDQ.
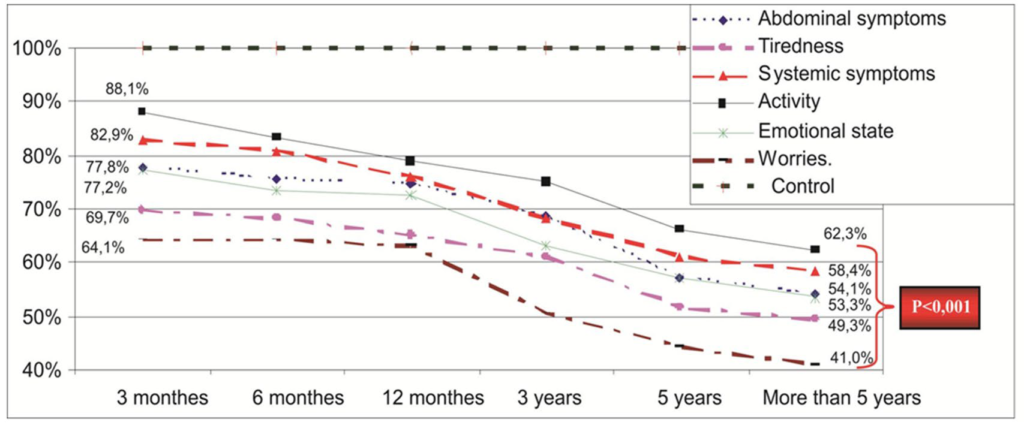
In up to 5 years follow-up after PSSh, progression of the pathological process in the liver causes deterioration of the “quality of life” indicators. Using the physical state scale of the CLDQ questionnaire, it is from 78.6%, relative to the control value of 100%, to 55.3% (p<0,001) within the 3 months period after surgery. With the psychological state scale, these values go from 72.4% to 48.8% (p<0,001) within more than five years of surveillance.
Model for End-Stage Liver Disease (MELD)
Not less interesting is the study of the dynamics of the Model for End-Stage Liver Disease (MELD) score after PSSh. This scale is widely used in many countries to assess the optimal timing for liver transplantation. Unfavorable life prognosis is associated with a MELD>15-18.
The pre-surgery mean score was 10.19±0.24 points on the MELD scale and 7.13±0.17 points by the Child-Pugh classification. This score was reliably less than in the liver transplantation group. Thus, reevaluation to readdress the need for liver transplantation in the dynamics had to be carried out at least 1 time per year (MELD score less than 10) in 62.5% of patients, at least 1 time in 3 months (MELD 11-18 points) 37.5% of patients.
In the immediate period after traditional PSSh there was no significant deterioration in the MELD scale (10.19±0.24 versus 10.94±0.23 points). The progression of liver failure with a high degree of activity was found in 6.3% of patients within one year after surgery. In another 6.3% of patients, EGV bleeding accrued: in one case due to shunt thrombosis and in the other case from gastric erosions due to portal gastropathy. Six months after PSSh, 3.1% of patients died due to progressing liver failure.
One year after operation, the MELD value changed from 10.86±0.22 points to 11.79±0.32 points (p<0.05). In addition, the MELD value higher than 15 points was found only in 10.3% of patients, they formed a group of patients that needed liver transplantation 15.6%
DISCUSSION
At present, interest for traditional PSSh has markedly fallen. On one hand, this is due to the widespread use of minimally invasive techniques, including endovascular interventions, like TIPS, as well as endoscopic techniques such as ligation and sclerotherapy. On the other hand, introduction of radical treatment in many countries made a certain influence on the demand of PSSh producing.16
Furthermore, Rosemurgy et al17 found that widespread use of TIPS continues although there is a certain lack of direct evidence of its effectiveness prior to surgical bypass.
Authors presented results of an 18-year follow-up of a prospective randomized study. Patient survival was significantly greater after traditional PSSh, as it was also for patients with a Child-Pugh class “A” (91 vs. 19 months) and Class “B” (63 vs. 21 months). Adequate shunt patency after PSSh was 45 months, whereas it was only 22 months after TIPS. The authors state that patients with Child-Pugh functional class “A” and “B” should have traditional bypass surgery rather than TIPS, leaving TIPS only for patients who present an initially severe (grade “C”) condition.17
Interesting results were obtained in a randomized clinical trial that evaluated the efficacy of emergency TIPS vs. PSSh. The study compared efficiency of TIPS vs. PSSh as a way to stop acute bleeding in emergency situations and was conducted in 154 patients with liver cirrhosis of all Child-Pugh severity groups.21
PSSh showed the best results with 97.4% hemostasis and less frequent encephalopathy. Additionally, life expectancy was three times greater for patients with PSSh than with TIPS (uncovered). And, despite the recommendation of many surgeons who suggest that PSSh is a surgery that should be arried out in planned fashion in order to prevent bleeding, authors recommend the use of this intervention as a means of treatment for acute bleeding. It should be noted that in another study by Orloff et al22 the advantages of PSSh compared to endoscopic procedures for bleeding control and recurrence prevention were also demonstrated. Puhl et al23 believe that PSSh should be considered as an optional method in portal pressure decompression, especially in patients with insufficient endoscopic or drug therapy, as well as in patients with the absence of transplantation indications. This also applies to the secondary prevention of rebleeding in patients with good liver function.
According to the interstate archive data analysis made in the United States the following reasons for TIPS were identified: First of all, during 4 years of observation (2000-2003) in the second most populous state (Florida, USA), only 165 PSSh where performed (an average of about 41 shunts in a year). On the contrary, TIPS where performed in 1486 patients among 1321 patients that were nearly 10 times greater. Secondly, number of centers offering the TIPS procedure was almost 10 times higher (more than 100). In general, mortality after these procedures was almost identical (11.0% TIPS versus 12.7% PSSh). Thus, the cost of TIPS was significantly lower ($62,000 vs. $107,000). However, conducting analysis, authors claim that if the mortality after TIPS procedure was due to the severity of patients and did not depended on the level of the surgical hospital, the mortality rate after the traditional PSSh depended both on the level of the medical center and the surgeon’s experience. Also, in spite of the advantages of the TIPS procedure, the authors summarized that, in long-term observation, traditional PSSh gave more superior survival rate prospects.24
Finally, a retrospective analysis by Elwood et al16 broth that the Warren procedure should be considered as the first line approach for patients with high risk of bleeding in Child-Pugh classes “A” and “B”, especially when endoscopic sclerotherapy is ineffective or in those cases where liver transplantation will not be needed within 5 years.
The effectiveness of the Warren procedure made under recommended readings is higher than that of TIPS. This option avoids the need of multiple stent patency monitoring and thus resenting.16 According to several clinical trials, this TIPS technique can be complicated, in 75-82% of patients, with endovascular graft dysfunction or thrombosis in a period from 6 months to 1 year after surgery.16,22
It should be noted that the accumulated experience of different hepatology schools determines the selection of a particular method, thereby giving continuity to the centers’ own results. For example, in some studies only the initial state of compensated liver function is considered as an indication for PSSh. In contrast, other authors only recommend alternative therapies. Thus, according to Semenova,25 endoscopic bleeding prevention is of minimal risk, although it does not allow sustainable longterm results to be achieved. In turn, the Warren procedure has a clear advantage with respect to long-term effects, but has a higher risk of bleeding. In this connection, the Warren procedure is preferable for patients with compensated liver cirrhosis without a history of surgery for PH. When liver cirrhosis is in subcompensation and patient has a history of surgical treatment for PH, or suffers from severe comorbidity, endoscopic sclerotherapy should be carried out as first choice of treatment.26
In another study, complications after PSSh were observed in 27.3% of cases, with a postoperative mortality of 4.5%. The author recommends H-type splenorenal bypass with a vascular graft insertion for patients with Child-Pugh Class A and a blood flow of 1000 ml/min through the portal vein. In patients with Child-Pugh class “B”, an inactive or low activity phase, and portal vein blood flow less than 1000 ml/min, the
Paciora procedure is recommended. In decompensated (ChildPugh class “C”) patients, the recommendation is to refrain from active surgery.26,27
In a study by held I.I. Dzidzava,28 the survival rate of patients after endoscopic ligation in the one year follow-up was 57.3%; in three years, 38%; in five years, 33.1%. In turn, longterm results in PSSh patients are characterized by the absence of rebleeding, thrombosis, and satisfying survival rates: one year, 84.8%; 3 years, 68.6%; 5 years, 51.3%; 10 years, 25.8%. The authors conclude that the performance of selective and partial PSSh is indicated in patients with liver volume more than 1200 sm3 and positive values of the liver dysfunction index.
Given the above, it can be concluded that, over the past decade, the development of minimally invasive methods, in order to prevent bleeding, has led to a decrease in the number of traditional PSSh performed. However, the conducted literary analysis shows that, even in centers which perform all kinds of operative treatments, including radical ones, traditional decompression of the portal system remains the method of choice. Furthermore, using adequate approach to indications, the results obtained with the mentioned procedure of choice are greatly superior in comparison with those of alternative endoscopic methods.
CONCLUSION
At the present time, leading Hepatology Schools have different views regarding which is the best choice for bleeding prevention. In most cases, surgeons prefer minimally invasive techniques, among which endoscopic procedures and TIPS are the most popular.
Now-a-days liver transplantation is the only radical treatment for liver cirrhosis, though for countries without transplantation service portosystemic shunts remain as an actual method of rebleeding prevention. In terms of highly developed transplantological service, minimally invasive techniques are optimal because bleeding itself can be viewed as an indication for liver transplantation. Additionally, performing TIPS or an endoscopic procedure provides the necessary time interval to find an organ donor and prepare the patient for radical surgery. Also in favor of minimally invasive technologies is the fact that these procedures are available to patients who are in serious, critical condition and abdominal surgery is associated with an unnecessary risk. On the other hand, when TIPS vs. PSSh results are compared, it can be seen that endovascular techniques have their negative side as well.
Obtained own findings objectively prove the effectiveness of PSSh in terms of hemorrhagic syndrome prevention with a high survival rate, as well as its important role in decreasing the need for liver transplantation. In the absence of bleeding risk, the possibility for dynamic patient monitoring, drug therapy and thus lengthening of the time period becomes opened before the transplantation what should be carried out in decompensated functional state of hepatocytes.
In portal hypertension surgery, PSSh remains one of the optimal ways to prevent bleedings from EGV. The conceptual importance of this type of intervention is determined not only by limited ability to perform liver transplantation, but also by a competitive perspective to reduce the demand for radical interventions in patients with functionally compensated LC. Thus, for patients with Child-Pugh functional class A and B, and in the absence of prospects of liver transplantation, traditional surgical methods, such as central partial or selective PSSh, should be considered as an actual competitive alternative.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.