INTRODUCTION
Food safety is a term that generally refers to ways and approaches to ensure that the production, preservation, distribution and consumption of food happen in a safe manner. Consumption of contaminated food could increase the risk of consumer acquiring an illness, caused a foodborne illness or disease. Every year, foodborne and waterborne diarrhoeal diseases kill about 2.2 million people, including 1.9 million children.1 The health care cost of foodborne diseases has become a heavy economic burden for countries. In Australia, 5.4 million cases of food poisoning per year were estimated to generate economic cost a AU$1.2 billion, while the estimated total costs of foodborne disease in New Zealand were NZ$ 1.6 billion in 2009. 2,3 In order to decrease or eliminate foodborne diseases effectively, the WHO developed a global strategy named “the Global Environment Monitoring System – Food Contamination Monitoring and Assessment Programme (GEMS/food)” to monitor and supervise foodborne diseases from different countries, including New Zealand and Australia.4
Foodborne disease is normally associated with microbiological, chemical or physical hazards. Among these three major health hazards, foodborne diseases, caused by pathogenic microorganisms, have become a big health issue. One of the key reasons is that microbial contamination is hard to predict and track back to its origin.5 A better understanding of the characteristics acteristics and epidemiologist of foodborne pathogens may lead to a decrease in the occurrence of microbiological foodborne outbreaks. Preventive and management approaches such as Microbiological Risk Assessment (MRA) and Hazard Analysis and Critical Control Point (HACCP) have been successful in lowering the risks of foodborne diseases. 6 The Australian New Zealand Food Standards (ANZFS) also direct food safety agencies to supervise and monitor foodborne pathogens in each country.
A foodborne outbreak refers to an incident where two or more people present a similar illness after consuming a common food or meal. In New Zealand, foodborne outbreak surveillance was commenced in 1997 by the Institute of Environmental Science and Research Ltd (ESR) on behalf of the Ministry of Health. In this surveillance programme the real-time data are collated, analysed and recorded on EpiSurv, a national notifiable disease surveillance system. 7 The OzFoodNet, foodborne diseases surveillance systems was established by Australia governments in 2000 to collect and analyse foodborne data from the National Notifiable Disease Surveillance System (NNDSS) and enhanced surveillance data from OzFoodNet sites.8 Data on foodborne outbreaks in quarterly annual reports published by ESR and OzFoodNet are a sound and reliable source of information about microbiological food safety issues in Australia and New Zealand. Data analysis of foodborne outbreaks is recognised as one of the effective approaches in estimating how many human cases of specific enteric diseases are associated with a specific food item.9 However, some mild foodborne illnesses may be ignored by patients or medical institutions so that the numbers of national foodborne illness attributing to overall foodborne diseases would consequently be underestimated.
The purpose of this review was to gather information on foodborne outbreaks reported during 2007 to 2011 in Australia and New Zealand.
A comprehensive comparison of the microbiological food safety issues and factors associated with foodborne outbreaks i.e. different foodborne pathogens, food types and preparation methods, was made. The outcome from our data analysis produced detailed information about the similarities and differences in the food safety challenges faced by each country. Finally, some recommendations and suggestions to decrease foodborne outbreaks were listed.
Information Collection and Data Processing
In order to compare microbial food safety issues in Australia and New Zealand between 2007 and 2011, information on foodborne outbreaks were collected and collated by searching online quarterly and annual reports published by OzFoodNet10-17 (Australia) and ESR18-22 (New Zealand). Foodborne pathogens, food vehicles and food preparation methods were the key factors in gathering data. The useful data on foodborne outbreak were classified into four groups, which included the total numbers of outbreaks in both countries, foodborne pathogens involved in the outbreaks, food vehicles associated with outbreaks, and food preparation methods. The data were converted into tabulated sheets using Microsoft Excel 2007TM and processed to generate into a presentable output. This allowed us to use recorded data to illustrate the microbial food safety issues in both countries through figures and graphics. However, it is important to notice the limitations of the data in the outbreak reports by ESR or OzFoodNet as, for example there may have been further changes and updates of information on foodborne outbreaks that occurred after outbreak reports were completed.
Following data collection and analysis, three electronic databases (Web of Knowledge, Google Scholar and Science Direct) were searched to explore information on microbiological foodborne pathogens, food vehicles and preparations methods associated with the highest numbers of outbreaks.
The numbers of overall identified foodborne outbreaks from the national surveillance systems in each country assisted to recognize and rank the microorganisms responsible for the top five foodborne outbreaks as reported by ESR and OzFoodNet. In other words, the electronic databases were used to study the characteristics of these microorganisms as well as to understand possible the sources and pathways for them to infect human population through food vehicles and food preparation places. Finally, the impact of changes in food policies and standards as well as implementation of different food safety strategies in Australia and New Zealand to prevent outbreaks from occurring was discussed.
Comparison of Food Safety Issues Between Australia and New Zealand
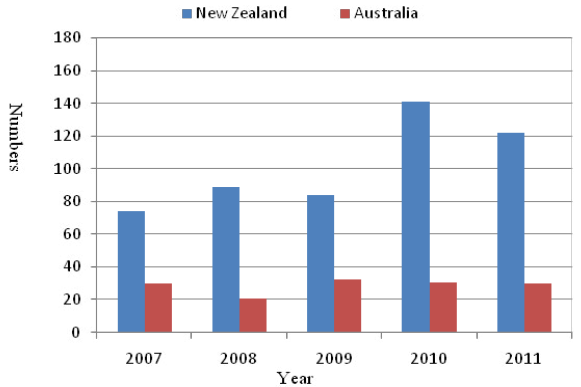
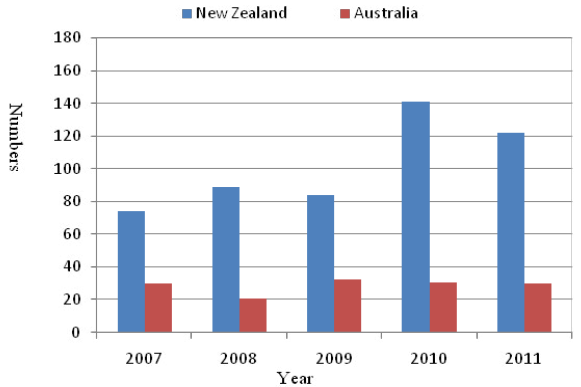
A total of 13 published quarterly and/or annual reports on foodborne outbreaks by ESR and OzFoodNet from 2007 to 2011 were chosen for the study of microbiological food safety issues in Australia and New Zealand. Figure 1 shows number of total outbreaks recorded in Australia and New Zealand from 2007 to 2011. There were 122 foodborne outbreaks reported in New Zealand in 2011, a 39.3% increase from five years ago (2007). When looking at the situation in Australia during the same period (2007 to 2011) the numbers of reported outbreaks remained fairly consistent at around 150 in each year. Comparison of total numbers of foodborne outbreaks showed that overall outbreak numbers in both countries were similar in 2008, 2010 and 2011; however, Australia had slightly higher numbers of foodborne outbreaks than New Zealand. The Australian population was approximately five times more than New Zealand, therefore population adjusted outbreak numbers in Australia were more appropriate to be used for comparing with outbreak numbers in New Zealand in 2007 (Australia, 30 and New Zealand, 74), 2008 (Australia, 21 and New Zealand, 89), 2009 (Australia, 33 and New Zealand, 84), 2010 (Australia, 31 and New Zealand, 141), and 2011 (Australia, 30 and New Zealand, 122) (Figure 2). Therefore, these data indicated that the New Zealand population was at a higher risk of facing a foodborne outbreak than our Australian counterparts.
Figure 1: Foodborne outbreaks in Australia and New Zealand, 2007 through 2011.

Figure 2: Population adjusted outbreaks in Australia and New Zealand, 2007 through 2011.
Association between Specific Food Service Sector and Outbreaks
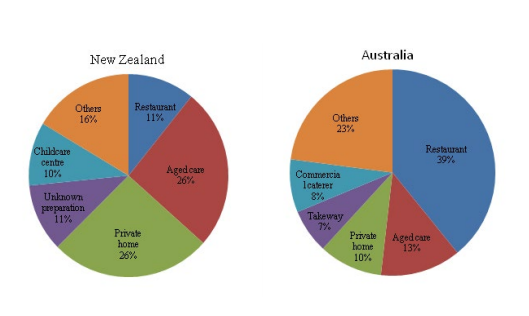
Improvement in food safety practices could prevent foodborne disease23 and this is one of the most important elements of strategies to reduce outbreaks. The lack of food safety knowledge among food handlers has been widely recognised as problematic area in food safety.23-25 Figure. 3 shows an association between food preparation places and foodborne outbreaks in both countries. In New Zealand, the most common food preparation places associated with foodborne outbreaks were private homes (26%), aged care facilities (26%), restaurants (11%), childcare centres (10%) and unknown preparation sites (11%). On other hand, in Australia, the high risk food preparation places were restaurants (39%), aged care facilities (11.8%), private homes (10%), commercial caterers (8%) and takeaway businesses (7%).
Figure 3: Percentage of food preparation places associated with foodborne outbreaks in Australia and New Zealand, 2007 through 2011.
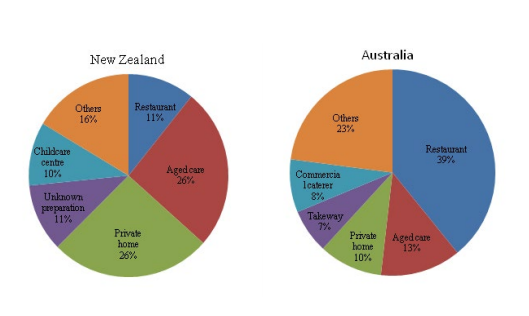
It was noticed that the three main food preparation places linked to the highest number of outbreaks were the same in both countries i.e. restaurants, aged care facilities and private homes. Restaurants were responsible the highest number (39%) of outbreaks in Australia, while in New Zealand, private homes (26%) and aged care facilities (26%) were leading places for the outbreaks. Restaurants associated with 11% outbreaks were the third major reason in New Zealand. The Top foodborne outbreak place (private homes) in New Zealand was the third major outbreak place in Australia. This clearly showed that both nations face different types of food safety challenges. The most important contributing factors in restaurant-associated foodborne disease outbreaks were food worker’s health and hygiene (responsible for the largest number of foodborne outbreaks occurring in the restaurants), food preparation practices within establishments and contamination outside the restaurant premises.26
Aged care facilities were at a high risk of foodborne outbreaks due to the low-immunity status of the residents. Aged population are particularly vulnerable to food infections by foodborne pathogens, thus these places are required to take extra care to avoid incidents happening. In order to prevent foodborne outbreaks, Kirk et al.27 suggested the facilities needed to enhance handling processes of puree foods and not to provide raw or undercooked eggs to the elderly. In addition to the home being a risky place, poor food-handling and food safety knowledge still resulted in a high risk of foodborne outbreaks.28 A right attitude by the individuals towards food-handling practices and hygiene conditions is important to reduce outbreaks in private homes.
It was found that the pattern of the top five high-risk food preparation places in Australia was different from that in New Zealand except cooking at home. The high numbers of foodborne outbreaks occurred in Australian food service businesses probably suggested more tourists or visitors came to this country than to New Zealand. It also suggested that more numbers of Australian dined outside than New Zealanders did. One way to improve this situation in Australia is to implement food safety programmes in food service industry (restaurants, cafes and bars) and to monitor them more closely. Standard operating procedures (SOP) should also need to be developed for entire food service sector. In order to improve food safety at private homes, one of the highest risk food preparation places in New Zealand, the efforts are needed on educating the general population on safe food handling practices.
Overall, in order to protect consumers from food poisoning episodes and to decrease the potential risks of foodborne outbreaks in both countries, the government agencies have worked together to develop joint food standards for more than fifteen years. Now there are documented regulations (Australia New Zealand Food Standards Code) developed by Food Standards Australia and New Zealand (FSANZ). 29 Furthermore, food service sector (including restaurants, takeaways and aged care facilities) in New Zealand need to comply with the new Food Act 2014 and the operator must have in place a system i.e., Food Hygiene Regulations 1974 or Food Safety Programmes (FSP) to ensure consumer’s safety. Although, these regulations are aimed to decrease risks of food poisoning incidents, the business operators in high-risk food preparation places play a crucial role to determine the food safety status of the final food products. Therefore, the external audit of these premises by the food regulatory authorities and food workers’ training and awareness of harmfulness microbiological hazards need to be improved through establishing an effective FSP in the food service sector.
Foodborne Outbreaks and Vehicle Foods
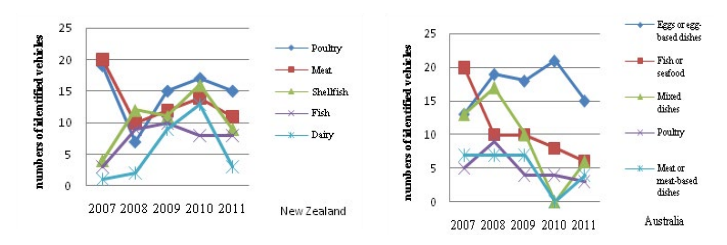
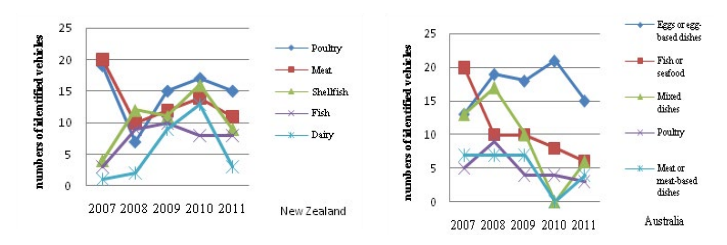
Food, as an ideal growth medium for microorganisms, is recognised as a transmission vehicle. Considering the vehicle or source implicated in foodborne outbreaks during the period from 2007 to 2011, there were 720 and 510 foodborne outbreaks associated with an identified vehicle or source in Australia and New Zealand, respectively (Figure 4). The top five foods or sources associated with foodborne outbreaks in New Zealand were shellfish, meat, poultry, fish and dairy, while consumption of contaminated eggs or egg-based dishes, fish/seafood, mixed dishes, poultry and meat or meat-based dishes were the top five food vehicles in Australia. Poultry and eggs, as major transmissions of foodborne pathogens Campylobacter and Salmonella were also noted in our analysis of the data. It has been suggested that the primary processing stage was the most cost-effective intervention site to decrease the risks of campylobacter contamination on poultry meat.30 Poultry, fish and meat were the common food vehicles identified in different outbreaks in both countries. Australia has specific problems with egg and egg-based foods whereas contamination of dairy foods was a particular issue in New Zealand. Most of the reported foodborne outbreaks in this article were noticed to be mainly associated with poor handling practices during food preparations and unsatisfactory hygiene in the private or commercial kitchens. So any improvement in food processing, storage and distribution will have a positive impact and contribute in lowering the potential risks of foodborne outbreaks.
Figure 4: Identified food vehicles associated with foodborne outbreaks in Australia and New Zealand, 2007 through 2011.
Major Foodborne Pathogens Associated with Foodborne Outbreaks
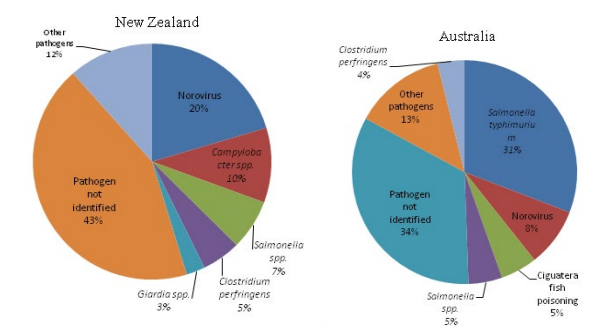
Data analysis of foodborne outbreaks in Australia and New Zealand during a five-year period (2007-2011) revealed the responsible biological agents. (Figure 5) presents an overall picture of biological contamination, including the top five foodborne pathogens in both countries. Norovirus (20%), Campylobacter spp. (10%), Salmonella spp. (7%), Clostridium perfringens (5%) and Giardia spp. (3%) were top five foodborne pathogens in New Zealand; in Australia, the top five pathogens or agents were Salmonella typhimurium (31%), Norovirus (8%), Ciguatera fish poisoning and Salmonella spp. (5% for each), C. perfringens (4%). In majority of the cases casual agent was unidentified (43% and 34% of total number of foodborne outbreaks in New Zealand and Australia, respectively). This indicated that both nations have a common challenge to improve outbreaks monitoring and investigation system for identifying the causal agent.
Figure 5: Top five foodborne pathogens frequently linked to outbreaks in New Australia and New Zealand, 2007 through 2011.
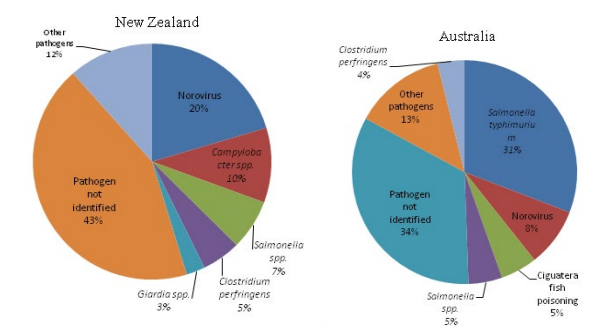
Foodborne pathogen data also showed that both countries had different food safety risks to handle i.e. norovirus in New Zealand and S. typhimurium, in Australia, were recognised as the major foodborne pathogens during 2007 and 2011. Norovirus and Salmonella were also responsible for nearly 75% of foodborne outbreaks reported in the Unite State. 26 The risk of Salmonella associated with eggs was investigated in South Australia and the authors found that was highly linked to egg shell instead egg contents. 31 They accordingly suggested a good hygiene in food preparation and prevention of cross contamination especially after handling broken, cracked or dirty eggs and expected such practices could contribute to reduce risks caused by this pathogen. Looking at the high outbreak numbers associated with norovirus in New Zealand, consumption of raw shellfish specifically raw oysters (contaminated by polluted pipe water or sea water) was the major attributing factor. 32 Nevertheless, serving raw or undercooked oysters is a well-accepted eating habit in New Zealand. Monitoring oyster growing water quality and educating people to eat thoroughly cooked oysters can be effective approaches for decreasing the norovirus outbreak numbers.
Norovirus: This is the most common contributor to acute nonFigure 4: bacterial gastroenteritis outbreaks in New Zealand. From 2002 to 2009, more than 38% of shellfish-associated outbreaks were caused by norovirius; a total of 1206 norovirus outbreaks were identified by genotyping and 825 (68.4%) outbreaks was related to norovirus GII.4.31 A study showed food handlers would be potential transmission mode of norovirus GII.e/GII.4 if a person had recovered from gastroenteritis prior to handling foods. 32 Waste water was also found to be linked to two norovirus outbreaks occurred in commercially farmed oysters.33 Greening et al. 31 suggested that tracking the variants of novovirus by country could give information about the various transmission modes and, thus would be useful in deceasing rate of international spread.
Salmonella: This microorganism causes salmonellosis, a major foodborne disease worldwide. The most common route of transmission of Salmonella was faecal-oral, which meant humans could be infected by consuming contaminated food or water by direct or indirect contact with faeces of an infected human or animal. In Australia and New Zealand, Salmonella typhimurium was the most common serovar followed by Salmonella enteritidis. 34 S. typhimurium was the causative serotype in 78% of 172 outbreaks in New Zealand; S. infantis and S. typhimurium phage type 135 were most commonly identified.35 Non-typhoid salmonellosis was identified as a foodborne disease in New Zealand. However, it was not clear how this pathogen infected consumers.36 Moreover, changes in the Salmonella serovar spectrum and distribution were found from year-to-year, thus leading to the complexity of the global epidemiology of Salmonella. 34 In Australia, Salmonella species were responsible for 36% of foodborne diseases from the consumption of unsafe eggs and eggbased dishes However, Salmonella associated with eggs was not endemic in New Zealand.19
Campylobacter: New Zealand has one of the highest risks of campylobacteriosis in the world. High population of Campylobacter was commonly found in the environment and on some raw plant or animal origin foods, in particular, raw poultry meat. 37 Identified routes of transmission were food (47%), direct animal contact (28%), overseas travel (7%), person-to-person transmission (4%) and water-related (3%).38 The reports also suggested that in summer there was a higher risk of campylobacteriosis than other seasons, however, the reasons for these observed seasonal trends were poorly understood. 39 Additionally, the implicated food vehicles associated with campylobacteriosis may vary from country to country.
Clostridium perfringens: This microorganism is one of the most common causes of foodborne outbreaks in New Zealand and Australia. High occurrences of Clostridium perfringens were related to the gut of food animals and humans, and the production of an enterotoxin was encoded by the C. perfringens enterotoxin gene (cpe).40
Ciguatera fish poisoning: This is a global disease caused by the consumption of certain marine fish that have accumulated orally-effective levels of ciguatoxins from complex environmental origins, thus resulting in diverse and long-term human health effects. 41 In Australia, the total number of foodborne outbreaks due to ciguatera fish poisoning were 43 and this placed in the third position in a total of 685 foodborne outbreaks from 2006 to 2010. There were only three outbreaks of ciguatera fish poisoning that occurred in New Zealand between 2008 and 2012 (data not included in this review).
Listeria: Listeriosis does not cause large numbers foodborne outbreaks, however, high mortality rates in immune-compromised individuals put it on the priority list of food safety authorities in New Zealand and Australia, so an enhanced listeriosis surveillance system was consequently established. In Australia, listeriosis cases were sporadic and limited to contaminated mussels, processed meats, sandwiches and fruit salads, in light of high protein, moderate water activity and low numbers of microflora in those foods.42
Changes of Food Policy and Standards
Foodborne pathogens are able to adapt and grow under adverse conditions, therefore, food policy and standards need to be updated in order to ensure their effectiveness in food safety plans. There have been significant changes in regulation and policies for Listeria control that have been changed from having no policy at all to zero tolerance for all foods in Australia, New Zealand, Italy and the Unite State.43 In New Zealand, the latest standard code states that L. monocytogenes must not be detected in 25 g sample of a food, particularly in ready-to-eat foods. In Australia, zero tolerance on a selected range of products (meat paste and pâté, smoked fish products, marinated smoked mussels and cheeses with a moisture content equal to or greater than 40% and a pH<5.0) at the end of processing or at wholesale has been implemented.43 Crerar et al.44 found that L. monocytogenes control in food supply chain was unsuccessful of mainly due to the inconsistent requirements and legislation for the control of this pathogen. These authors also noticed that in the dairy and seafood industries L. monocytogenes could be controlled effectively by legislation and by the food safety programme of the business. Some specific control measures have been mandated through legislation in the food retail and service sectors.
Poultry meat has been scientifically established to be a significant exposure pathway in New Zealand. 38,39 In order to prevent and decrease Campylobacter contamination, the policy changed from zero to low levels of contamination because researchers found that the current interventions (such as biosecurity measurements) were not able to eliminate Campylobacter in the poultry production chain completely. 45 On the other hand, broiler chicken carcasses at the end of primary process was recognized as an important pathway for Campylobacter to infect human population in New Zealand; the Ministry for Primary Industries (MPI) consequently commenced and conducted “Campylobacter Risk Management Strategy” from 2006. This policy change helped to drop the estimated foodborne cases of campylobacteriosis in New Zealand i.e., from 4500 cases per quarter in 2006 to 2000 cases per quarter in 2013.46
CONCLUSION
This paper reviewed foodborne outbreaks reported by ESR (New Zealand) and OzFoodNet, (Australia) between 2007 and 2011. The total numbers of these outbreaks during these five years were also summarised and compared, according to foodborne outbreaks associated with pathogens, transmission vehicles and preparation setting in each country. The most frequently implicated vehicles were seafood, meat and poultry, but the implicated foods relating to high risks of the outbreaks varied from each country. For example, a high risk of Salmonella infection associated with eggs and egg-based foods in Australia and dairy products in New Zealand. Private homes, restaurants and aged care facilities were associated with the highest number of outbreaks in both countries. Data analysis in this review suggested that the surveillance of foodborne outbreaks needed to be increased to develop food safety policies in the future.42 A research survey on trust in the Australian food supply indicated that participants had little knowledge, or interest, in understanding of food regulations even while they expressed high trust in the food system.47 Therefore, common control measures such as food safety education and good practices (cleaning and disinfection) would help to effectively reduce risks of microbiological foodborne illness in Australia and New Zealand.