INTRODUCTION
Urinary and bowel dysfunction is a condition that encompasses loss of bladder and bowel control which is characterized by partial or complete loss of urination and defecation or urine incontinence. The most common cause of constipation requiring surgical intervention is a prostatic disease and its sequela, and perineal hernia.1 Urinary and bowel dysfunction is multifactorial that is mainly caused by spinal cord injury cranial or at the lumbosacral level. Spinal cord damage is mainly caused by traumatic injury due to different accidents. Traumatic injury of the sacrococcygeal area occurs frequently in young cats of either sex. This injury may lead to temporary or permanent urinary incontinence.2 Lumbo-sacral epidural injections in cats have a rare but serious potential risk of causing damage to the spinal cord. Development of chronic urinary retention and constipation due to decreased perineal reflex was reported in a cat after single epidural administration of morphine.3 Nerve injury at this point could eliminate voluntary and supraspinal control of voiding which initially leads to an are flexic bladder and complete urinary retention, followed by the slow development of automatic micturition and bladder overactivity mediated by spinal reflex pathways.3,4 Urinary incontinence in cats was also associated with a variety of congenital and acquired disorders. Incontinent cats with spinal cord disorders warrant a more guarded prognosis than do cats with other bladder or urethral disorders.5 Constipation resulting from pelvic nerve damage causes increased resting tone of the colon and rectum and decreased ability to evacuate feces. Fecal incontinence is rarely a management problem for the owners.2
In this condition, voiding is commonly inefficient because of simultaneous contractions of the bladder and urethral sphincter. Therefore, spinal cord injury can affect both urine storage and voiding.4,6 Following traumatic injuries to the spinal cord, affection of other structures like the hind leg and tail were also recorded in 84.3% of the cats.2 Occasionally there is a development of megacolon due to prolonged obstruction from intractable impaction to the rectum and colon.7 Patients that had an anal tone and perineal sensation at the time of initial examination following injury have a higher chance of returning to normal urinary function after treatment intervention.2 In companion animals, the characteristic clinical signs of severe and lower motor neuron spinal cord injury include detrusor hyporeflexia or areflexia and sphincter hypotonia or atonia, which can lead to increased bladder compliance and constant urine leakage.6 The diagnosis of the present case was based on history, clinical and physical examination of the abdominal area. The present report was aimed to show techniques and outcomes of colotomy to resolve constipation secondary to bowel dysfunction in the cat.
CASE DESCRIPTION
History and Clinical Findings
A one-year-old female cat weighing 1.3 kg was presented to the Veterinary Teaching Hospital of Addis Ababa University with a history of anorexia, dullness, and absence of defecation for the last 8-days. As the owner reported, when they first noted the abdominal distention it was recognized as she was getting pregnant. However, since her abdomen distention was increasing with the unexpected speed they started to follow other conditions and found that she could not defecate, lost appetite, and lost her hind leg control. As a result, she started suddenly falling when she was in an attempt of walking as usual. Additionally, the owner informed us that the cat has not been walking normally since her birth and she was using her metatarsal bone as her footpad with flexed hock joint. Clinical examination revealed stunted growth, poor body condition, a very weak anal and pedal reflex, and she was in lateral recumbency due to highly distended abdomen that could not allow her to stand. Abdominal palpation revealed an elongated hard mass in the abdominal cavity. Other findings include a slightly pale and dry mucous membrane, weak and rapid pulse (140 beats/minute), moderate dehydration (8%), RT 36.8 °C. Based on history and clinical findings the case was diagnosed as constipation and exploratory laparotomy was indicated to resolve the problem.
Patient Stabilization and Pre-Operative Preparation
Pre-operatively the animal has received IV 10 ml of 40% glucose and lactated ringer solution that was fixed at 5 ml/kg/hour for 1 hour before surgical intervention to stabilize the patient. At the same time procaine penicillin G at dose rate of 20,000 IU/kg, IM was administered. Since the cat was weak and easily manageable, the caudal ventral midline was shaved and scrubbed before anesthetizing the animal to reduce prolonged exposure to the anesthetic agent.
Anesthesia and Animal Control
The cat was premedicated with intramuscular tramadol, atropine sulfate, and xylazine hydrochloride @ 2 mg/kg, 0.02 mg/kg, and 1.1 mg/kg, respectively. Then she was controlled in dorsal recumbency with her legs tied to the surgical table. For induction anesthesia, ketamine hydrochloride was given with slow IV administration at 5 mg/kg. Finally, the surgical site was disinfected aseptically and draped with a fenestrated sterile drape.
Surgical Procedure and Techniques
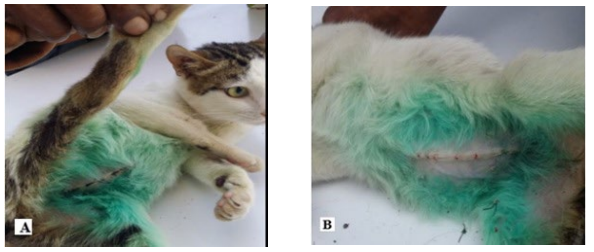
About 6 cm long ventral midline incision was made onto the caudal abdomen. The abdominal cavity was entered after incising a very thin linea alba. The abdominal cavity was investigated and distended urinary bladder and impacted colon were identified. Then accumulated urine was voided by direct gentle compression of the bladder before undergoing colotomy (Figure 1A). Then the impacted intestine was exteriorized from the abdominal cavity and the laparotomy incision was packed off with sterile gauze to prevent accidental spillage of intestinal contents (Figure 1B). About a 5 cm long enterotomy incision was made on the anti-mesenteric border of the colon and fecal mass at the incision site was first removed by holding with gauze while gentle outward pushing is maintained from the mesenteric side of the colon (Figure 1C). The mass located proximal to the incision and in the rectum was removed by gentle milking to the incision site. After removing all hard fecal mass, the edge of the colotomy incision was cleaned with different gauze soaked in normal saline. The intestine was closed with a lambert suture pattern using 3-0 chromic catgut taking care of stricture formation. Pair of surgical gloves worn during colotomy was changed and laparotomy packs were removed to replace the intestine into its normal position and the abdominal cavity was flushed with 10 ml normal saline. The abdominal incision was closed with a single layer of simple interlocking suture pattern using the same suture material. The skin was closed with a simple interrupted suture using 2-0 suture silk (Figure 2A). The surgical procedure was completed without adding a maintenance dose.
Figure 1. Colotomy in Progress Following Urinary and Bowel Dysfunction

(A) Distended urinary bladder (B) Exteriorized impacted colon
(C) Removal of fecal mass after anti- mesenteric incision of the colon
Figure 2. Skin Suture and its Removal
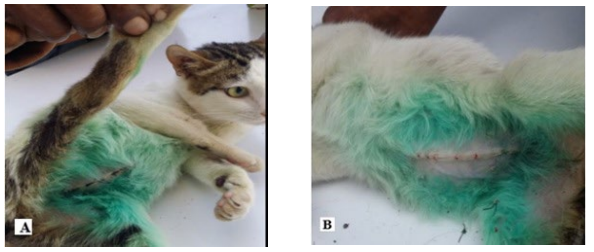
(A) Simple interrupted skin closure (B) On 18-days of operation and skin suture removal
Post-Operative Care and Outcome
Post-operatively the topical wound spray was applied on the surgical site and tramadol injection was prescribed 2 mg/kg, IM for the next 2-days. Intravenous fluid therapy was continued until she has received a total calculated fluid deficit and discontinued on the 3rd day since she was started drinking boiled milk. Antibiotic given pre-operatively was continued for 7-days. The owner was advised to provide liquid/soft feed for 10-days and to gradually return to a regular diet. Additionally, oral laxative bisacodyl 1 mg/day was administered after 2-days of operation and was given occasionally until the defecation difficulty was resolved. The patient was so alert and started feeding normally on 3rd day of surgery. However, she was unable to use her hind legs due to previous damage to the spinal nerve at the lumbosacral level. Therefore, neurobion forte tablet was administered for consecutive 20-days as supportive treatment. The skin suture was removed on 18-days of operation, after complete healing of the surgical wound (Figure 2B). The cat was able to pass her feces completely though she can not decide where she has to defecate. She faced urination incontinence and was unable to empty her bladder. Therefore the owner was advised how to manually compress the bladder to assist urination. Her hind leg was showed excellent improvement and she was able to run, play, and hide on 52-days follow-up. Though, the problem of passing feces was resolved after surgical intervention, fecal and urine incontinence were remain as the main problem during the follow-up period.
DISCUSSION
Urinary and bowel dysfunction is a common condition characterized by partial or complete loss of urination and defecation or urine incontinence.3 This condition is multi-etiological that could be congenital and acquired disorders.5 The acquired disorders are mainly caused by spinal cord injury at the lumbosacral level.4,8 A radiographic examination can be conducted to identify the presence of impacted fecal material and other abdominal abnormalities.7 Unfortunately in the current case, physical diagnosis and exploratory laparotomy were used to identify intra-abdominal abnormalities. The present surgical procedure was performed to remove fecal mass from the colon following constipation secondary to the unknown cause of spinal cord injury. In recent procedures directly treating the primary cause of intestinal obstruction-like1 was found difficult due to equipment unavailability. To resolve this primary cause (spinal cord injury) sacral anterior root stimulation in combination with sacral deafferentation was developed. By using this method human patients with refractory voiding and bowel dysfunction were revealed good improvement.9 As reported by Saha et al,7 the cats with intestinal obstruction and found refractory to medical therapy were finally selected to undergo surgical intervention. In the present case, medical treatment was not tried before surgical intervention. Because the patient cannot wait or receive medical treatment as her abdomen was highly distended and in a recumbent position.
In the current case report, the animal was pre-medicated using xylazine, tramadol, and atropine sulfate while ketamine was used as induction anesthesia and the surgical procedure was completed without any problem. This is almost in agreement with Saha et al7 work that used xylazine along with ketamine and diazepam. In contrary to this Song et al3 used dexmedetomidine for sedation while ultra-short acting non-barbiturate propofol and midazolam were used for induction anesthesia and lumbosacral morphine epidural was used to provide peri-operative analgesia. In the present case, spinal cord injury was confirmed following hind limb paresis manifested by incoordination and urinary and fecal incontinence that was observed after the surgical procedure.
In the present case, the abdominal incision was closed with a single layer of simple interlocking suture pattern since the cat has poor body condition and a skinny abdominal wall. Skin closure was made with simple interrupted suture without burying knot since the skin and subcutaneous tissue was very thin and does not allow subcuticular suture. The management of persistent lower urinary tract dysfunction resulted from severe thoracolumbar spinal cord injury can be challenging. The management of this condition consists of regular manual bladder compression that can result in better outcomes if the primary cause is corrected.6 Currently, the site of nerve injury was not identified and management of urine incontinence was found difficult. Nonetheless, the owner was advised to manage it manually by applying gentle bladder compression.
Sacral nerve stimulation has proven to be an effective treatment modality for voiding dysfunctions that are refractory to conservative treatment, particularly for patients with urinary and fecal incontinence.9,11 However, if clinical signs of constipation persisted for more than 6-months it is unlikely to function normally because of irreversible neuromuscular damage to the colon due to persistent pathologic dilation.7 In the present case, the problem of constipation was completely resolved after surgical correction while fecal and urinary incontinence were continued as the main problem. Though skin sutures removal was possible on the 8th day operation as conducted by Osuna,1 currently skin suture was removed after complete healing on the 18th day with no surgical complication. Suture removal was delayed to prevent wound dehiscence associated with increased intra-abdominal pressure during manual compression of the bladder.
CONCLUSION
Surgical removal of impacted fecal mass has enabled the cat to void feces without any support and played a major role in the survival of the patient. She also gradually returned to her previous gait after 20-days of operation following supportive treatment. Urine and fecal incontinence were continued as the main challenging condition despite the survival of the animal.
ACKNOWLEDGMENTS
The authors are thankful to Dr. Mahari Teklu for his help through provision of all necessary materials to perform surgical procedure and Haimanot Girma for his assistance with the post-operative management of this case.
AUTHOR CONTRIBUTIONS
All authors contributed to the manuscript preparation and final submission. The main surgical procedure and original manuscript writing were performed by Cheru Telila Feyisa, the manuscript structure modification and editing by Jiregna Dugassa Kitessa, while Zerihun Mulatu Tuji was participated as assistant surgeon and reviewing process. Finally, all authors read and approved the final manuscript submission.
ETHICAL CONSIDERATION
The approval of ethical committee was taken for conducting this study and followed all the animal ethics and welfare guidelines.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.