1. Bedford Russell AR, Breathnach A, Sender P. Confirmed group B streptococcus infection: tip of the iceberg. Arch Dis Child Fetal Neonatal. 2001; 84: F140. doi: 10.1136/fn.84.2.F140b
2. Patterson MJ. Streptococcus. In: Baron S, ed. Medical Microbiology. 4th ed. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. 13.
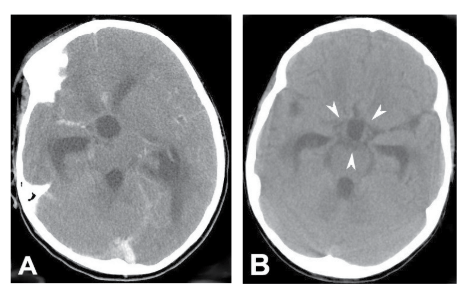
3. Srinivasan L. Ramanan R. Hydrocephalus secondary to group B streptococcal meningitis. Journal of Maternal-Fetal & Neonatal Medicine. 2004; 16(1): 67-68. doi: 10.1080/14767050412331283148
4. Robbins SL, Cotran RS. Pathological Basis of Disease. 7th ed. Copyright©2005, Saunders, An Imprint of Elsevier. 373.
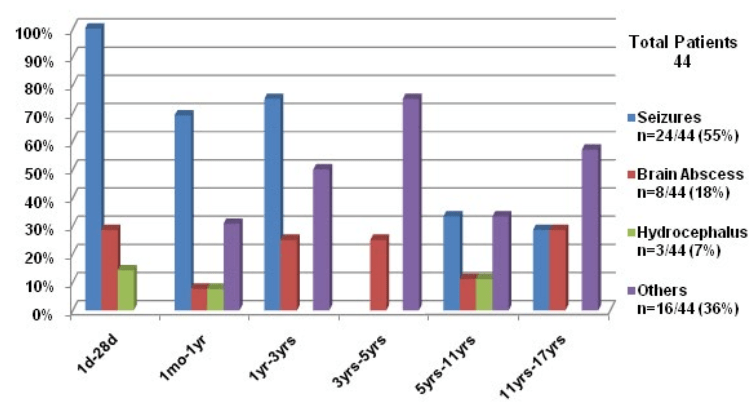
5. Torres RS, Fedalto LE, Torres RF, Steer AC, Smeesters PR. Group Astreptococcus meningitis in Children. Pediatr Infect Dis J. 2013; 32(2): 110-114. doi: 10.1097/INF.0b013e31826fd4af
6. Dillon HC Jr. Group A type 12 streptococcal infection in a newborn nursery. Successfully treated neonatal meningitis. Am J Dis Child. 1966; 112(3): 177-184. doi: 10.1001/archpedi.1966.02090120045002
7. Ramanathan K, Grossman A. Neonatal Streptococcal meningitis. Ill Med J. 1967; 132: 705-707.
8. Coulter JB, Buchannon CR, Vellodi A, Hart CA, Sills JA. Group-A streptococcal infection in the newborn. Lancet. 1984; 2(8398): 355-356.
9. Murphy DJ Jr. Group A streptococcal meningitis. Pediatrics. 1983; 71(1): 1-5.
10. Verboon-Maciolek MA, Krediet TG, Ertbruggen IV, Gerards LG, Fleer A. Severe neonatal group A streptococcal disease. Eur J Pediatr. 2000; 159(6): 450-452. doi: 10.1007/s004310051305
11. Lardhi A. Neonatal group A streptococcal meningitis: a case report and review of the literature. Cases J. 2008; 1(1): 108. doi: 10.1186/1757-1626-1-108
12. Wong VK, Wright HT. Group A beta-hemolytic streptococci as a cause of bacteremia in children. Am J Dis Child. 1988; 142: 831-833. doi: 10.1001/archpedi.1988.02150080037016
13. McMahon BJ, Barrett DH, Bender TR, Brenneman GR, Hurwitz RM, Cannon W. Group A streptococcal meningitis in an infant: report of a case associated with a community outbreak due to M-type 4 organisms. Alaska Med. 1979; 21(4): 57-59.
14. Congeni BL, Bradely J, Hammerschlag MR. Safety and efficacy of once daily ceftriaxone for the treatment of bacterial meningitis. Paediatr Infect Dis J. 1986; 5(3): 293-297. doi: 10.1097/00006454-198605000-00004
15. Moses AE, Beeri M, Engelhard D. Group A streptococcal meningitis: reports of two cases. J Infect. 1998; 36(1): 116-118. doi: 10.1016/S0163-4453(98)93558-7
16. Rezvani M, Jerome Y. Yager AE, Hartfield DS. Group A streptococcal meningitis as a complication of an infected capillary haemangioma. Eur J Pediatr. 2004; 163(1): 19-21. doi: 10.1007/s00431-003-1334-4
17. Yagupsky P, Giladi Y. Group A beta-hemolytic streptococcal bacteremia in children. Pediatr Infect Dis J. 1987; 6(11): 1036-1039.
18. Harden A, Lennin D. Serious supportive group A streptococcal infections in previously healthy children. Pediatr Infect Dis J. 1988; 7(10): 714-718.
19. Melzer M, Joashi U, Murdoch I, Gransden W. Group a streptococcal meningitis with an infected BCG scar. JR Soc Med. 2000; 93(12): 641. doi: 10.1177%2F014107680009301211
20. Brandt C, Kitz R, Lutticken R, Brade V. Streptococcus pyogenes Meningitis Complicating Varicella in a 3-month-old Child. Scand J Infect Dis. 2003; 34: 876-878. doi: 10.1080/00365540310016844
21. Gertner M, Rodriguez L, Barnett SH, Shah K. Group A beta-hemolytic Streptococcus and Waterhouse-Friderichsen syndrome. Pediatr Infect Dis J. 1992; 11(7): 595-596.
22. Burech DL, Koranyi KI, Haynes RE. Serious group A streptococcal diseases in children. J Paediatr. 1976; 88(6): 972-974. doi: 10.1016/S0022-3476(76)81052-9
23. Dehority W, Uchiyama S, Khosravi A, Nizet V. Brain abscess caused by Streptococcus pyogenes in a previously healthy child. J Clin Microbiol. 2006; 44(12): 4613-4615. doi: 10.1128/JCM.01724-06 h
24. Shadravan I, Fishbein J, Hebert LJ. Streptococcal meningitis with an unusual port of entry. Am J Dis Child. 1976; 130(2): 214-215. doi: 10.1001/archpedi.1976.02120030104021
25. Shetty AK, Frankel LR, Maldonado Y, Flaco DA, Lewis DB. Group A streptococcal meningitis: report of case and review of literature since 1976. Paediatr Emerg Care. 2001; 17(6): 430-434. doi: 10.1097/00006565-200112000-00007
26. Rotimi VO, Grange AO, Lawal SF, Eke PI. Childhood meningitis caused by group A streptococci belonging to a new serotype: a case report. East Afr Med J. 1984; 61(8): 648-651.
27. Paul SP, Jerwood S. Group A streptococcal septicemia, meningitis and cerebral abscess: case report and literature review. Turk J Pediatr. 2012; 54(2): 180-183.
28. Pettersen G, Ovetchkine P, Tapiero B. Group A streptococcal meningitis in a pediatric patient following cochlear implantation: report of the first case and review of the literature. J Clin Microbial. 2005; 43: 5816-5818. doi: 10.1128/JCM.43.11.5816-5818.2005
29. Arnoni M, Berezin E, Safadi M, Almeida F, Lopes C. Streptococcus pyogenes Meningitis in Children: Report of Two Cases and Literature Review. The Brazilian Journal of Infectious Diseases. 2007; 11(3): 375-377. doi: http://dx.doi.org/10.1590/S1413-86702007000300015
30. Brown CC, Pickering LK, Baker CJ. Group A streptococcal meningitis without predisposing factors. South Med J. 1981; 74(8): 1029-1030. doi: 10.1097/00007611-198108000-00049
31. Jevon GP, Dunne WM Jr, Hawkins HK, Armstrong DL, Musser JM. Fatal group A streptococcal meningitis and toxic shock-like syndrome: case report. Clin Infect Dis. 1994; 18(1): 91-93. doi: 10.1093/clinids/18.1.91
32. Bruun T, Kittang BR, Mylvaganam H, Lund-Johansen M, Skrede S. Clinical, microbiological and molecular characteristics of six cases of group A streptococcal meningitis in western Norway. Scand J Infect Dis. 2010; 42(9): 665-671. doi: 10.3109/00365548.2010.483477
33. Khan MA, Viagappan GM, Andrews J. Group A streptococcal brain abscess. Scand J Infect Dis. 2001; 33(2): 159.
34. Steppberger K, Adams I, Deutscher J, Müller H, Kiess W. Meningitis in a girl with recurrent otitis media caused by Streptococcus pyogenes–otitis media has to be treated appropriately. Infection. 2001; 29(5): 286-288. doi: 10.1007/s15010-001-1065-2
35. Jagdis F. Group A streptococcal meningitis and brain abscess. Paediatr Infect Dis J. 1988; 7(12): 885-886.
36. Levy EN, Griffith JA, Carvajal HF. Localized meningoencephalitis and group A streptococcal bacteremia. Clin Pediatr (Phila). 1992; 31(7): 438-441. doi: 10.1177/000992289203100712
37. Wilson NW, Copeland B, Bastian JF. Posttraumatic meningitis in adolescents and children. Pediatr Neurosurg. 1990-1991; 16(1): 17-20. doi: 10.1159/000120497
38. Sommer R, Rohner P, Garbino J, Auckenthaler R, Malinverni R, Lew D, Kaiser L. Group A beta-hemolytic streptococcus meningitis: clinical and microbiological features of nine cases. Clin Infect Dis. 1999; 29(4): 929-931. doi: 10.1086/520461
39. Mandell, Bennett, Dollin. Principles and Practice of Infectious Diseases. 5th ed. Copy right 2005 Churchill Livingston. 287-288.
40. Ronald EH, Hill A. Intraventricular Hemorrhage and Post Hemorrhagic Hydrocephalus. Current and potential Future Intervention. Clin perinatal. 1997; 24(3): 589-605.