INTRODUCTION
Chylous ascites or chyloperitoneum are defined as a milky fluid collection in triglycerides in the abdominal cavity.1 It is responsible for 0.001-0.005% of hospital admissions.2 Chylous ascites can be associated with many conditions such as malignancy, trauma, lymphatic injury, radiation, cirrhosis, and fibrosis but are rarely associated with bowel obstruction.3 We discuss the course and management of a 31-year-old male patient who presents with chylous ascites due to small bowel obstruction post-Roux-en-Y gastric bypass.
CASE REPORT
A 31-year-old gentleman admitted via accident and emergency complaining of 8-months history of intermittent abdominal pain, which became severe in the past three-days, with 10-year background history of laparoscopic Roux-en-Y gastric bypass. The pain was severe colicky, associated with nausea and vomiting. He was vitally stable upon admission (Pulse 88 bpm, BP 130/88 mmHg and Temperature 37 °C). Abdominal examination, mild tenderness at the epigastric region, and distention. Laboratory investigation sent, the result was unremarkable, except for an increase in C-reactive protein (CRP) which was 9.9 mg/L ( normal 0-8).
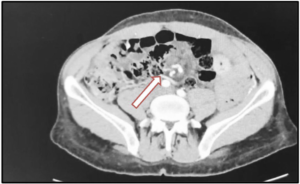
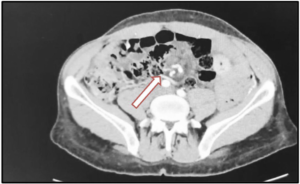
A computer tomography scan (CT-scan) urgently done, showing dilated and thickened small bowel loops, and swirling of the it to vessels and fat at the centre of the abdomen, mild pelvic fluids and enlarged mesenteric lymph node consisted of internal hernia (Figure 1). The surgical team discussed the result with the patient, and he agreed to go for surgery.
Figure 1. CT-Scan Showing Central Abdominal Swirl Sign
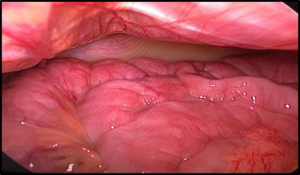
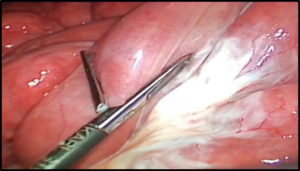
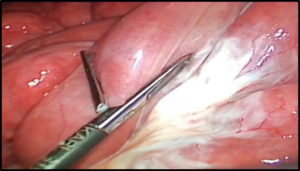
Intra-operatively we found a moderate amount of milky fluid at the pelvis and between bowel loops (Figure 2), no signs of perforation nor ischemia. As we reached Peterson’s space, the mesentery and the small bowel loops engorged at the minor defect created from the previous laparoscopic Roux-en-Y gastric bypass (LRYGB) covered with thick white fluid (Figure 3). The bowel loops released were viable, with no ischemia or perforation.
Figure 2. Intra-Abdominal Chylous Ascites
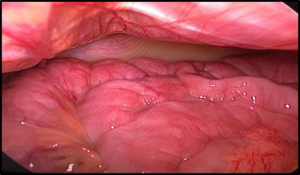
Figure 3. Engorged Mesentery with Chyle Leaking at the Peterson’s Space
The defect was sutured continuously with a non-absorbable thread, and the fluids were aspirated and sent for culture and analysis.
POST-OPERATIVELY
Patient recovery was uneventful, and he received four days of broad-spectrum antibiotics (Tazocin 4.5 gm IV and metronidazole 500 mg IV). We discharged him after resuming a regular diet and opened his bowel.
First 2-weeks visit, uneventful recovery at home, with regular bowel habit and diet. Abdominal examination was unremarkable, and the wound was clean and healing well. Laboratory of abdominal fluid consist of diverse organisms, and fluid analysis was high for triglycerides 300 d/L consistent with chyle.
DISCUSSION
The disruption of abdominal cavity lymphatics causes chylous ascites. Lymphatic drainage starts from the intestinal trunk and further to the chyle cistern and then upwards to the thoracic trunk.4 Interference to this pathway leads to chylous ascites. There is three mechanism of disruption which are: (1) Exudation of the lymphatics directly to the peritoneal cavity (2) obstruction of the lymphatic system due to neoplastic lesion (3) direct damage to the lymphatics due to trauma of surgery.5 Clinical presentation of chylous ascites as described by Browse et al6: (1) painless abdominal distension (75%), (2) malnutrition/hypoproteinemia (60%), (3) dyspnea (46%), and (4) steatorrhea (46%). Diagnosed chylous ascites can be with CT-scans imaging by identifying the density of the intra-peritoneal fluid or directly via paracentesis, which appears as a turbid milky fluid, with a triglyceride level of >110 d/L.1
Chyloperitoneum due to small bowel obstruction because of Roux-en-Y gastric bypass is rare; just a few case reports mentioned in the literature.6 Reconstruction of bowel limbs creates novel spaces, namely Peterson’s space between the Roux limb and the transverse colon and jejuno-jejunostomy space. The incidence of internal hernia post laparoscopic Roux-en-Y gastric bypass is 0.2-11%.7
Chyloperitoneum due to small bowel obstruction is due to mesenteric engorgement with chyle, resulting in the white staining seen in the case report.8 Akrama et al3 described the presence of chyle as due to obstruction of the lymphatic, only with no disruption of the arteriovenous system. Hence, in internal hernia due to volvulus obstruction of the small bowel, the low-pressure systems are initially obstructed example, the lymphatics and venous and the high-pressure system are patent, such as the arterial. Thus, the presence of chylous ascites bowel indicated bowel viability, as we can confirm from the case report. Nevertheless, delay intervention in such cases may lead to sequential compromise of the arterial system leading to ischemia and perforation. Thus, prompt intervention is required.
CONCLUSION
Chylous ascites or chyloperitoneum is a rare presentation in patients with internal hernia. Only a few cases report mentioned in the literature, and it is a good sign of bowel obstruction and indicator of bowel viability.
INSTITUTIONAL BOARD PERMISSION
Yes.
CONSENT
The authors have received written informed consent from the patient.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.