INTRODUCTION
Fracture-dislocations of the proximal humerus (PH) with fragmentation and destruction of the tubercle zone are rare among all fractures of the PH, but they account for up to 58.3% of fracture-dislocations of all localizations.1,2 Fracture-dislocations result from excessive force of the traumatizing agent and overstrain of muscles counteracting trauma that lead together to the fracture of the proximal metaepiphysis of the humerus and to the dislocation of its head from the articular cavity.3 This type of damage is the severest with regard not only to the bone tissue of the humerus and scapula, but also to periarticular tissues, joint capsule, tendons and muscles of the rotator cuff, the tendon of the long head of the biceps, and it often causes adverse consequences for the function of the joint and the limb as a whole.4-7 All patients with fracture-dislocations are a priori considered a high-risk group for the development of aseptic (ischemic) necrosis of the humeral head. Radiological criteria for ischemia were formulated by Hertel et al,8 and, according to him all patients with fracture-dislocations of the PH have radiological signs of the rupture of the respective arc that predicts ischemia.
There are no unified approaches to the treatment of fracture-dislocations of the PH in the scientific literature, and the data obtained by different researchers are contradictory. Along with the growing relevance of shoulder joint replacement in the treatment of fracture-dislocations of the PH, it is believed that ischemia of the humeral head is associated with worse results after surgical treatment of this particular type of injury.9,10 In a randomized trial, Olerud P et al11 did not find any statistically significant differences in the results of endoprosthetics and conservative treatment observed one year after the injury. The relative rarity and the severity of the course of fracture-dislocations of the PH explain the difficulties related to perception and implementation of the proposed in the literature treatment algorithms, which could hardly be used in the routine work of trauma centers.
The study was aimed to assess the results of treatment for fracture-dislocations of the PH within different time frames for optimizing treatment tactics.
Objectives of the study are: 1. To analyze currently used treatment options for fracture-dislocations of the PH and time from injury to surgery in the context of short- and medium-term results and complications; 2. To investigate anatomical factors affecting functional outcomes of treatment; 3. To assess long-term functional outcomes of treatment for fracture-dislocations of the PH; 4. To develop a practical algorithm facilitating decision-making in treatment of fracture-dislocations of the PH on the basis of the obtained data.
PATIENTS AND METHODS
This retrospective cohort study evaluated clinical outcomes of 25 patients with fracture-dislocations of the PH (15 patients were analyzed for short- and medium-term results, and 10 – for longterm results).
At the first stage of this retrospective study, we formed a clinical group consisting of 15 patients with fracture-dislocations of the PH who were treated at the Russian Scientific Research Institute of Traumatology and Orthopedics and at general hospitals in St. Petersburg, Russia during the period from 2005 to 2016 (the patients received specialized care between 6-hours and 14-days after the injury). This group (with B3, C3.2 and C3.3 fractures according to the Arbeitsgemeinschaft für Osteosynthesefragen/ Association of the Study of Internal Fixation (AO/ASIF) fracture classification) included 11 women aged 66.0±8.5-years and 4 men aged 52.2±12.5-years. When recruiting patients to this group, we deliberately did not include those with the simplest and the most prevalent combination of fracture and dislocation of the shoulder, namely dislocation of the shoulder with the fracture of the greater tuberosity (type 11-A1.3 fractures according to the AO classification), since this type is not of interest in terms of justifying the rational choice of treatment tactics.
At the second stage, conducted at the same hospitals in St. Petersburg, Russia. Ten cases were analyzed for long-term results of treatment for fracture-dislocations of the PH. All patients were treated during the period from 2005 to 2014, and the follow-up period ranged from 1 to 9-years.
All patients underwent: clinical examination, questionnaire survey (100-points Constant score), and shoulder X-ray in 2 views. Cortical index indicating the relative thickness of the cortex in relation to the total shaft diameter was calculated. Twelve copies of inpatient medical records (discharge summaries) and outpatient records were analyzed.
The studied groups were comparable with respect to diagnosis, cortical index, types and initial magnitude of bone fragments displacement and other studied parameters.
Data were analyzed using free software: past and instat. non-parametric wilcoxon test was used to compare the pre-operative and post-operative values within each group. Mann-Whitney u test for independent samples was used to compare patient characteristics, follow-up, clinical scores, and radiographic data. All statistical tests were performed 2-sided. Statistical significance was set at p<0.05.
All patients gave written informed consent for the use of their data for research purposes at the beginning of the data collection process. Ethical approval was granted for utilizing the dataset for research purposes by the Ethic Committee of Russian Scientific Research Institute of Traumatology and Orthopedics named after R. R. Vreden.
RESULTS AND DISCUSSION
Analysis of Short- and Medium-Term Results of Treatment for Fracture-Dislocations of the PH
According to the types of treatment the clinical group was divided into the following subgroups: conservative therapy without surgery − 5 patients, surgical treatment − 10 patients, including 4 cases of extra-cortical osteosynthesis and 1 case of open reduction followed by osteosynthesis of the PH with the use of two spokes and cerclage wiring (according to Weber’s method). This particular case of osteosynthesis was included in the group of patients treated with the use of extra-cortical osteosynthesis. Two patients underwent closed reduction and blocking intramedullary osteosynthesis, and 3 patients underwent unipolar shoulder replacement (USR). The composition of the group of patients with fracture-dislocations of the PH who underwent surgery is presented in the table, which shows the types and shapes of the implants used, as well as their quantitative characteristics (Table 1). The standard deltoideopectoral approach was used to perform plate osteosynthesis and arthroplasty. In patients who underwent blocking intramedullary osteosynthesis, the anterolateral mini-open surgical approach was used. In this case, the closed reposition of the fragments and the closed reduction of the dislocation were performed under X-ray control (C-arm) and achieved by manual “pushing” the head of the humerus out of the armpit, followed by the manipulations with the spokes (Steinmann pin), until the restoration of the correct relationships in the shoulder joint. When fragmentation of the tubercle zone (the area of tuberosity) was detected, the tendons of the rotator cuff were fixed (sutured) to the bone fragments. Other technical details of these standard manipulations have been described in many recent publications and manuals.
| Table 1. Data on the Surgical Hardware Used in the Course of Surgical Treatment of Patients with Fracture-Dislocations of the PH |
|
Type
|
Number of Patients
|
| Plates with angular stability of screws (LCP type) |
2
|
| Plates without angular stability screws (DCP type): T- and L-shaped |
2
|
| Spokes and wire cerclage |
1
|
| Intramedullary locking nails |
2
|
| Unipolar prostheses |
3
|
| Total |
10
|
The average blood loss during the surgical treatment of fracture-dislocations of the PH amounted to 240.0±65.8 ml. Comparison of the amount of blood loss during different surgical operations revealed similar values for both types of osteosynthesis and higher values for shoulder replacement. The difference between the values varied up to 100 ml. Low levels of blood loss in case of fracture-dislocations of the PH could be explained by the absence of traumatic injuries of the major vessels due to the dislocation of the bone fragments or to the iatrogenic damage during the process of reduction.
The average duration of the surgical operation of the discussed type amounted to 84.5±30.0-minutes (Me=80). The “fastest” surgical method of restoring normal anatomy of the PH, as a matter of course, was open reduction of bone fragments with extra-cortical osteosynthesis (61.0±15.5-minutes (Me=55)), and the “slowest” one was blocking intramedullary osteosynthesis, which required twice as much time on average (125±7-minutes (Me=125)). The average duration of USR in case of fracture-dislocations of the PH amounted to 96.7±17.5-minutes (Me=95).
Among the patients of the studied group, there were no vascular disorders related to the compression of the neurovascular bundle, but in 3 cases (20%) we observed neurological disorders (brachial plexopathy). According to descriptive statistics, the average length of pre-operative hospital stay in case of patients with the studied traumatic pathology who underwent surgery amounted to 3.75±2.90-days (Me=3), and the values varied from 1 to 11- days. Only 3 patients underwent surgical treatment within the first 24-hours, and 3 patients more between 24 and 48-hours. Within the first week after the injury, 5 more patients were operated. Analysis of the results obtained with the use of the constant scale revealed that among the patients operated within the first 48-hours the average score was 69.0±22.3 points (Me=71), while in patients operated later, during the interval between 3 and 7-days, the average score was 50.4±9.0 points (Me=50). It is noteworthy that better results of restoration of the shoulder function were observed in patients who underwent osteosynthesis within the first 24-hours after the injury (Figure 1).
Figure 1. Distribution of the Average Values of the Constant Outcome Score in Patients with Fracture-dislocations of the PH Operated within Different Periods of Time after the Injury. Group 1 – within the First 48-hours, Group 2 – During the Interval between 3 and 7-days

The subgroup of patients who were treated conservatively included 4 women aged 69.0±7.5-years and 1 man-aged 76-years. All these individuals had absolute indications for a surgical intervention from the orthopedist’s point of view, but they did not undergo it due to the absolute contraindications (severe somatic illnesses). Surgical interventions were not performed on the basis of internists’ and/or anesthesiologists’ consultative medical reports indicating extremely high-risks of death during the surgery or anesthesia. In the presence of absolute contraindications, the reposition of the fragments and the reduction of the dislocation were not performed. The injured limb was immobilized with a soft bandage (sling) until the pain was relieved, and then rehabilitation was initiated. The average score for conservatively treated patients amounted to 34.0±8.0, and these unsatisfactory functional results were predictable.
Among the anatomical factors affecting the outcome of treatment, in our opinion, the most important types of fragment displacement were as follows: displacement of tubercles and the distance of their displacement from their physiological localization, damage and displacement of fragments at the level of the anatomical neck, fracture of the fragment involving the articular surface, the value of cortical index. Displacement at the level of the surgical neck in combination with the angular deviation of the fragments or without it, in the presence of a non-reduced dislocation of the fragment involving the articular surface, was not significant for predicting unfavorable outcomes of treatment.
Assessment of the degree of initial displacement of tubercles and its impact on the results of treatment showed that significantly better results were obtained in case of displacement no more than 10 mm (p=0.041). Patients with displacement no more than 10 mm had an average score of 68.0±16.1 points (Me=69.5), while those with displacement of the tubercle(s) exceeding 10 mm had an average score of 49.5±19.5 points (Me=44).
Among the patients of the studied group, in 6 (40%) cases the fracture line did not pass through the articular surface of the humeral head, and in the remaining 9 (60%) cases the damage affected the fragment involving the articular surface. The results of treatment were dependent on this factor with a difference in the median values of the score up to 10 points in favor of the subgroup with an intact articular surface. Similar data were obtained when comparing the scores of patients who had fracture-dislocations with the fracture line passing at the level of the anatomical neck of the humerus.
As a next step, the impact of the value of the cortical index was considered. Its values were not significantly different in the compared groups (p=0.1). However, the values of the cortical index were linked to the score values. In patients with low cortical index values (less than 5 mm), the average score was unexpectedly higher than in those with high index values – 68.8±19.1 points (Me=70) and 47.3±19.9 points (Me=47), respectively. When explaining these findings, it is necessary to take into account that lower scores in patients with cortical index values exceeding 5 mm resulted from the fact that 4 out of 6 patients did not underwent any reduction, and, consequently, the dislocation of the shoulder persisted. The remaining two patients obtained satisfactory scores of 67 and 72 points.
Analysis of the results of treatment for fracture-dislocations of the PH allows us to conclude that the delay in restoring normal anatomy of the PH or avoiding surgical interventions at all lead to functional disorders of the shoulder joint.
Unipolar shoulder replacement, as a method of treating fracture-dislocations of the PH, should not be a unified way of solving the problem, since the results obtained in case of physically active patients do not always meet their needs. Comparison of the function scores in the medium and long-term revealed that patients who underwent osteosynthesis had similar satisfactory score values, while those after USR had low values.
Analysis of Long-Term Results of Treatment for Fracture-Dislocations of the PH
In the group analyzed for long-term results of treatment, all 10 patients underwent shoulder hemiarthroplasty.
The analysis of the results showed that the average score in this group was high and amounted to 75.9±13.6, with the median value equal to 76 points.
Relatively high score values in our study could be explained mainly by the low-level of pain intensity in the setting of a relatively small amplitude of movement, which had been also reported in other studies.13
Analysis of Treatment-Related Complications in Patients with
Fresh Closed Fracture-Dislocations of the PH
In 1970, one of the founders of the shoulder surgery, Neer,14 wrote that a patient with a comminuted fracture-dislocation of the PH should be considered a potential candidate for shoulder replacement. This postulate had a strong underlying evidence base, stemming from investigating a large sample of patients and in-depth analysis of the outcomes and complications of treatment with the use of other methods. For this reason, in our study we did not aim to prove the benefits of one or another method for treatment of comminuted fracture-dislocations of the PH.
As mentioned above, osteosynthesis was performed in 7 clinical cases, and USR – in 3 cases. Patients, who underwent osteosynthesis, despite a relatively high rate of complications (71.4%), had better score values: 69.3±17.5 points (Mean=72) vs. 52.3±11.7 points (Mean=50).
Such a high rate of complications following osteosynthesis resulted not only from the complex architectonics of tissue damage, the high-risk of neurovascular bundle damage and corresponding difficulties in performing an accurate reduction of fragments, but also from post-operative problems. These may include heterotopic ossification of the tendons of the rotator cuff of the shoulder. This complication was not found in any of the observed clinical groups of patients, and it is rare, according to the modern literature.15
The most serious and irreversible complication following treatment of fracture-dislocations, posttraumatic avascular necrosis, was detected in 3 out of 15 patients (20% of cases). Among them, there were 2 cases of necrosis after conservative treatment without reduction of the deformity and reposition of bone fragments.
Algorithm for Choosing the Optimal Treatment Tactics for
Patients with Fresh Closed Fracture-Dislocations of the PH
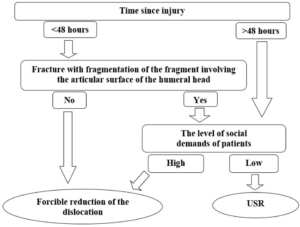
Based on the results of the study, we propose the following algorithm for determining the tactics of surgical treatment in cases when a fracture-dislocation of the PH with complete dislocation of the fragment involving the articular surface of the humeral head from the articular cavity of the scapula is diagnosed (Figure 2).
Figure 2. Schematic Diagram Representing the Algorithm for Choosing Therapeutic Tactics for Patients with Fracture-Dislocations of the PH
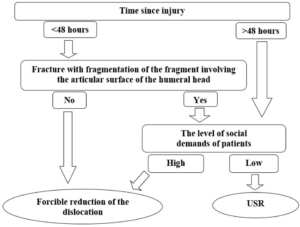
It should be taken into account that the tactics of conservative treatment in such cases is bound to a pronounced deficit in shoulder function and patients’ dissatisfaction with the results of treatment.
The algorithm of choice of the therapeutic tactics in case of the considered severe injuries lies in a phased and sequential evaluation of clinical and X-ray indicators. The time elapsed since the injury should be the key clinical indicator for the choice of treatment. If it exceeds two days, it is advisable to choose shoulder joint replacement as the optimal method of surgical treatment, since irreversible ischemic changes in the humeral head can lead to unsatisfactory results and require delayed arthroplasty of the injured joint in the future.
At the second stage, it is necessary to make a radiographic assessment of the presence of damage to the fragment involving the articular surface of the humeral head. Radiography of the shoulder joint in two standard views does not always allow to obtain reliable information. Therefore, a computerized tomography (CT) scan may be required in some cases. If the fracture of the fragment involving the articular surface of the humerus (with its fragmentation or without it) is confirmed, the most predictable and favorable result of treatment can be obtained by shoulder joint replacement.
The issue of shoulder joint replacement surgery in treatment of patients with fracture-dislocations of the PH remains debatable. The results of our study showed that neither patients, nor doctors were satisfied with the outcomes of USR. Thus, in our opinion, the USR technique does not provide good functional results in most cases, due to the complexity of intra-operative restoration of anatomy of the tubercle zone of the PH and tendons of the rotator cuff of the shoulder joint. However, this type of surgical treatment allows reducing the level of pain in patients with low functional demands for the operated limb and is the most preferable for the elderly. For patients with high physical demands to the function of the shoulder joint and a professional need to perform hard physical labor, shoulder replacement can be chosen only in cases of terminal destruction of the PH. Also, in our opinion, USR in this situation should be reconsidered in favor of the reverse total shoulder replacement. In cases when the time from injury does not exceed 48-hours and there is no fragmentation of the fragment involving the articular surface of the humerus, it is advisable to perform an organ-preserving operation of forcible reduction of the dislocation and osteosynthesis of the fracture by any of the available modern methods.
As for young and middle-aged patients with high functional demands, in cases of terminal and irreparable damage of the PH, the choice of this type of endoprosthesiсs, in our opinion, should be reconsidered in favor of the use of modern reversible endoprostheses.
One of the limitations of our study is the small number of observations. The retrospective nature of the study and the rarity of the discussed type of injury did not allow us to exclude or control confounding variables. Non-consistent treatment and follow-up could also affect the results of the study. However, we believe that our data described above contribute to the understanding of the problems associated with treatment for fracture-dislocations of the PH.
CONCLUSION
Analysis of treatment outcomes of 15 patients with multifragmental fracture-dislocations of the PH showed that the most significant factors affecting clinical results of treatment were the time from injury to surgery (less or more than 48-hours) and the degree of fragmentation of the bone fragment involving the articular surface of the humeral head. Significantly better results were obtained when the magnitude of the displacement of tubercles did not exceed 10 mm. Since the outcomes of USR were unsatisfactory, we suggest that it should be used only in cases of terminal and irreparable damage of the PH or in patients with low functional demands.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.