INTRODUCTION
Adult Epiglottitis (AE) is a relatively uncommon1 but potentially life- threatening condition and a delay or missed diagnosis can be catastrophic. It should be considered in the differential diagnosis of any adult patient who presents with sore throat and odynophagia. In the majority of the cases, the diagnosis is based on clinical history, physical examination and with help of plain radiography of soft tissue of the neck.2 Because of the non-specificity of its symptoms, and availability of CT scan in the Emergency Department (ED), CT scan of the neck is used in evaluating AE as well as in excluding other conditions such as deep neck spaces, peritonsillar abscess and complications of epiglottitis such as abscess formation. However, there are currently no published reports on the CT scan accuracy in diagnosing AE.
Our case report illustrates the challenges facing the Emergency Physicians in diagnosing AE and the role and limitations of CT scan of neck in evaluating AE.
CASE REPORT
This is a 26 year old African American female complaining of sore throat, difficulty swallowing and shortness of breath after she ate a barbecue eight hour prior to the ED visit. There is no difficulty speaking, cyanosis but feels anxious. Also had a cough one week prior to this visit.
Review of system: positive for sore throat- negative for SOB
On physical examination:
•Vital signs: Temp: 98.6 – O2 sat=99% ( Room Air )- BP= 113/78-HR=82 , RR=16
• General: not in acute distress
• Throat:
▪ marked erythema. No exudates- no peri-tonsillar abscessuvula midline
▪ Neck is supple – no adenopathy.
• Chest: clear- breathing easily on room air- no wheezing/rales/ bronchi. • Cardiovascular and neurological: Within normal limit.
• The reminder of the physical exam= normal Laboratory:
• CBC: increased WBC (13,000/µL). Rapid strep throat: negative.
• Mononucleosis spot test: negative. Initial ED Management:
• Was given Benadryl 50 mg, IV and Solumedrol 125 mg, IV
ED Course:
At 2hr later:
• Persisting sore throat and odynophagia. • ENT consult called and CT scan of the neck ordered
At 6 hr:
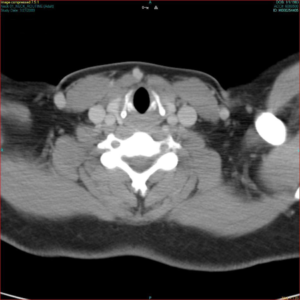
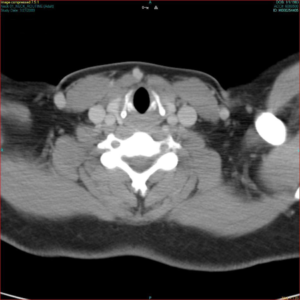
• CT scan result: no acute finding- no asymmetry- no soft tissue swelling (Figure 1)
Figure 1: CT scan with IV contrast with AP view of the larynx. Normal larynx: no acute finding associated with Adult Epiglottitis. No asymmetry, no soft tissue swelling, no abscess.
At 8 hr:
• Direct laryngoscope by ENT showed focal areas of swelling in the epiglottis consistent with Epiglottitis;
• Patient is admitted to ICU and given IV Rocephin, Clindamycin and Decadron with tracheotomy tray at bedside.
At 24 hr:
Repeat enhanced CT of the neck showed thickening of right aspect of epiglottis. Bases of the tongue, vallecula and puriform sinuses are normal. Findings are consistent with acute epiglottitis
At 72 hr:
patient was discharged from the hospital
DISSCUSION
Epiglottitis is a rapidly progressive, potentially lethal inflammation of the epiglottis and larynx that causes airway obstruction. Historically, it was a disease of the childhood, but recent reports have shown an increase in incidence in adult population. The incidence of AE is about 1.8 cases per 100,000 adults 3 with a reported mortality between 7-20%, whereas the incidence in children has significantly decreased due to routine immunization of children with H. influenza since April 1985. Recent reports have shown that other organisms such as group A beta hemolytic streptococcus or staphylococcus aureus have been implicated in AE. A diagnosis of AE (or supraglottitis) should be elicited in any adult patient with a sore throat and dysphagia with other symptoms such as odynophagia, stridor or drooling. AE displays more non-specific and indolent course than in children making its diagnosis more challenging. Clinically, the differential diagnosis includes peritonsillar abscess, abscess in the deep neck space, laryngitis and ingested foreign body.
In the majority of cases, AE is diagnosed by history and confirmed by finding on flexible laryngoscope performed by ENT specialist.
Lateral plain neck radiographs may be helpful in diagnosing AE .It is performed on a single lateral upright view of the neck in extension with a portable equipment in the ED. Since acute airway obstruction can occur any time, no X-rays should be done until airway is secure. Reported sensitivity is 88-100 % and specificity between 87-96 % in diagnosing AE.4 Typical finding include enlargement of epiglottis (thumb sign) typically more than 8 mm, thickening of the ary-epiglottis folds more than 7mm is a sensitive and specific sign and arytenoids and pre-vertebral soft tissue swelling. However x-rays finding in adults are more subtle than in children and epiglottis may be normal.
Because CT scan is readily available in the ED, it often is used in the evaluation of AE and indicated in patients who are unable to undergo adequate physical examination, to exclude other ENT emergencies and identify local complications such peritonsillar or deep neck abscess when direct laryngoscopy is unavailable. CT scan is only recommended for patients with stable airway and requires airway monitoring since patients will be in a supine position which increases the risk of acute respiratory distress. Furthermore, it may require a relatively lengthy period of time away in the Radiology suite with associated anxiety with the procedure itself. To our knowledge, there is no reported sensitivity or specificity of CT scan of the neck in diagnosing AE in our literature. The most common CT findings are thickening of epiglottis,5,6 the ary-epiglottis folds, false and true vocal cords, platysma muscle and prevertebral fascia. The finding of multiloculated fluid collections should raise the suspicion of a deep neck abscess. Loss of vallecula is an independent sensitive and specific sign of AE, but further validation is needed.7
Our case report fits the category of moderate AE8 (no airway intervention, discharged in 3 days) in which CT scan may be insensitive in diagnosing AE, but it is however the best test to diagnose deep epiglottis abscess. Recent development in CT technology using high resolution, 3D reconstruction images may detect lesions not identified by laryngoscopy but further studies need tobe done to demonstrate the role and accuracy of such CT scan in AE. The recent widespread use of Ultrasound in the ED has led to its usefulness in diagnosing AE: Ko et al9 have shown that the measurement of the anteroposterior diameter of the epiglottis was helpful in making the diagnosis of AE. However, this finding is preliminary and need confirmation in a larger scale prospective study. Direct laryngoscopy performed by ENT specialists remains the gold standard in accurately diagnosing AE. When these specialists are unavailable, Emergency Physicians can perform indirect laryngoscopy to establish the diagnosis. Both should be performed only when conditions to secure the airway are available. Current treatments of EA include medical therapy, airway management and ICU admission.
CONCLUSION
In conclusion, our case report illustrates the challenges facing the Emergency Physicians in diagnosing AE and the role and limitations of CT scan. Since there is no reported sensitivity or specificity of CT scan of the neck in diagnosing AE in our literature, it is advisable to follow the current guideline: CT scan is not recommended to establish such diagnosis initially, should only be used to exclude other ENT emergencies and to aid in the diagnosis of AE when an adequate laryngoscopic examination cannot be performed or unavailable.