INTRODUCTION
Cervical strain and whiplash are common diagnoses given to patients who sustain cervical pain after a motor vehicle accident (MVA) with whiplash being the most commonly treated emergency room diagnosis in the USA.1 These patients are routinely seen by primary care physicians and can be referred to outpatient physical therapy (PT) care. The internationally recognized definition of whiplash injury according to the Quebec Task Force (QTF) on whiplash associated disorders (WAD), is an acceleration deceleration mechanism of energy transfer to the neck may result from rear-end or side-impact motor vehicle collisions, but can also occur during driving or other mishaps.2 The whiplash diagnosis is given to patients with cervical pain associated with mva whether or not they have sustained the true quick flexion extension mechanism that defines a whiplash injury. In Quebec, the incidence rates for whiplash are reported as 70 per 100,000 individuals while this is reported as 106 per 100,000 in Australia. In the United Kingdom,3 in 1,000 individuals will sustain a true whiplash injury per year.3 There is also an increase in patients seeking healthcare for WAD in the last 30 years as greater than 3/1000 individuals in North America and Western Europe have sought care for whiplash injuries resulting from MVA.1,4 Though cited costs vary, annual costs attributed to treatment of individuals who develop chronic symptoms and subsequent work loss in the UK is reported as 3 billion pounds per year and up to $230 billion in the USA.
Though the Quebec Task Force (QTF) on WAD was convened to provide clinical practice guidelines, the resultant document is critiqued as lacking rigor due to the dearth of high-level evidence available for review and selection bias in the methodology. The New South Wales Clinical Guidelines for the Management of WAD funded by the Motor Accidents Authority5,6 was undertaken to update the QTF guidelines based upon more recent evidence, however encountered the limitation of low-level evidence and so also deferred to professional expertise of the panel for formation. Therefore, there exist clinical practice guidelines to assist the clinician in the management of WAD, however, clinical expertise continues as a critical component to patient management.
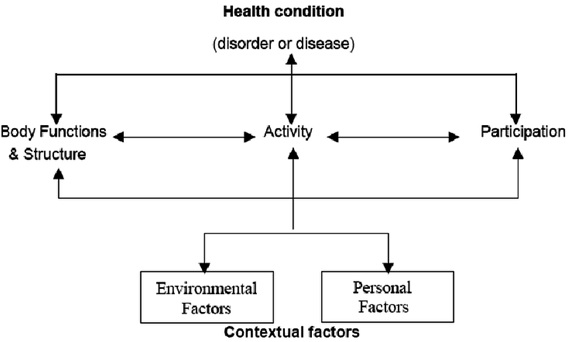
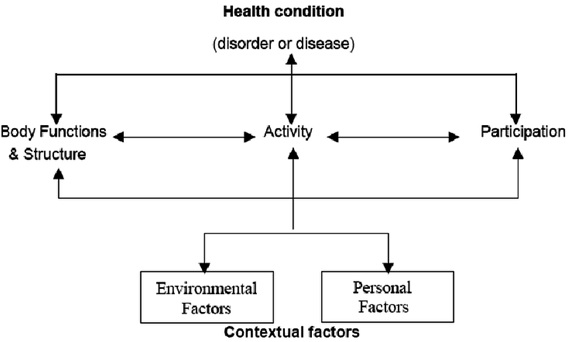
To demonstrate an application of clinical practice guidelines and use of clinical expertise the following is a Case Analysis, whereby a specific real-life situation is used to provide assessment and interpretation of the decisions made in the management of a cervical strain/whiplash injury. The line of reasoning and assessment of the assumptions made with this patient scenario are included following the data presented. In accordance with current clinical practice, the World Health Organization’s International Classification of Functioning, Disability and Health (ICF) Model,7 see Figure 1, is used as a framework for the holistic approach used with this patient case along with the Patient Management Model for PT Intervention that includes, Examination, Evaluation, Assessment, Diagnosis, Prognosis, Intervention.8
With regard to prognosis, various estimates are reported. The QTF concluded that most whiplash injuries are self-limiting and “short-lived”,2 however, other authors have found that between 14 and 42% of patients develop chronic symptoms for longer than 6 months and 10% of these have severe pain of a constant nature.9 Other authors have estimated that the prognosis for patients with a true whiplash injury is “good” for 40% of the instances, they fair “moderately well” in 40% of the cases, and poorly in 20%.10 Predictors of prognosis include the following four categories of factors. Previous medical history, such as prior head injury, pretraumatic headaches, osteoarthritis. Current symptoms of radicular irritation, radiating numbness or severe neck symptoms. Current psychosocial factors such as long-term problems in adjustment to symptoms of an injury or illness (coping mechanisms), family or job related psychosocial issues, financial problems, and finally, socio-demographic factors to include older age, female gender, less than full-time employment and having dependents.2,10 These factors taken into consideration are part of the holistic approach to patient care, under the areas of physical, activity and context both personal and environmental as listed in the ICF model (Figure 1) and affect both recovery and sport performance for active individuals.
Figure 1. International Classification of Functioning, Disability and Health Model
CASE REPORT
The patient for this case is a professional male athlete at the height of his golf career. Prognosis percentages provided by Cote et al,9 were unacceptable, however, based upon the predictors provided by the QTF and MVA reports, the prognosis for this individual is good overall. Use of a problem-solving approach within the ICF model provides opportunity to determine a differential diagnosis and plan of care for return to optimum function as quickly as possible and avoidance of chronic sequelae.
This case also presented the opportunity to assess cervical function and the contribution of core stability to performance. Core stabilization is a “buzz word” in gyms and physical therapy facilities across North America and has gained credibility as an intervention in the clinical setting. The transversus abdominus muscle has been identified as a key muscle of the inner core of the trunk,11 with the longus colli muscle of the anterior cervical region functioning similarly to provide stability to the upper core of the body.12 There is evidence citing that with neck pain, the deep neck flexors can be weak, with patients demonstrating compensation by using the superficial cervical flexors, such as the sternocleidomastoid (SCM) and anterior scalene muscles. The relevance of the longus colli muscle (LCM) to spinal stability, functional outcome and pain management is often overlooked. Therefore, individuals with WAD must be evaluated for segmental strength and stability. Incorporation of core stability training in rehabilitation to include the often overlooked muscle, the LCM can promote full recovery and enhance performance. Spinal segmental stabilization as initially described focused on training co-contraction of the deep core muscles of the transversus abdominus with the multifidus13 More recent recommendations have included the deep core muscles of the cervical region12 and was applied in this case.
Examination
History and systems review: JD is a 31-year old male professional golfer who was in an MVA, assessed in the Emergency Room and subsequently referred to physical therapy (PT) by his primary care physician (PCP) within 30 hours of the injury. JD was in the passenger seat and though wearing a seatbelt, recalls hitting the right side of his head upon the console of the vehicle but also reports a cracked windshield noted after the collision. He was to begin his off-season training program in the following week to prepare for a competitive season to begin in 2 months. In the emergency room (ER), X-rays were taken and during the out-patient PT assessment, he reported no symptoms of dizziness, syncope or nausea. The nature of pain was variable with pain level on a 0-10 scale 5/10 at best and 7/10 at worst; aggravated by cervical and UE active range of motion AROM. Though the primary care physician (PCP) prescribed codeine for pain and flexeril for muscle spasm use at night, neither had been used. When asked about the use of NSAIDs, the patient reported taking 4 generic ibuprofen tablets (800 mg total) with each meal.
Medical history: X-rays taken, uncertain of views and no copies available. Negative for hypertension, diabetes mellitus, prior surgeries. Good health per patient report with yearly physicals and checks for skin lesions due to sun exposure when needed. Negative for anxiety or depression treatments–relevant question due to strong pain medications prescribed by doctor of medicine (MD) and prognostic predictor of outcome with WAD. Hairline fracture of lunate metacarpal due to trauma 8 months prior with good healing and no complications.
Social and activity history: Travels and competes in tournaments 38 weeks per year. Resides with parents and maintains physical fitness with aerobic, flexibility, strengthening and core stability components to fitness program.
Tests and Measures
• Grip dynamometer strength: Right 110 lbs, 108, 110; Left 105 lbs, 104, 105.
• Palpation: Exquisite tenderness along bilateral levator scapulae, erector spinae bilaterally and anterior scalene mm. Increased tissue tension along bilateral upper trapezii mm and SCM.
• Joint Mobility testing: Upper cervical stability testing of C1, C2 ligaments of stability (alar, transverse), also assessed for symmetrical motion and presence of crepitus or signs of fracture. Joint stability and mobility findings: No ligamentous stability at alar nor transverse ligaments. At O-A joint: flexion right and sidebent left positions with decreased right rotation at C1-C2; hypomobility noted C5-6 with decreased SB Right noted in extension; elevated 1st rib left, thoracic hypomobility with decreased extension at segments T3-6. No S&S noted or reported with end-range passive rotation right nor left nor sustained position at end range.
• Functional activities: Unable to sit/stand for more than 15 minutes due to pain and unable to demonstrate golf swing due to reported “weight of head”.
• Neural: Positive for adverse neural tension using Upper Limb Tension Test Pattern #1 Median nerve R>>L; all others negative. No symptoms projecting to extremities, intact to light touch and pressure in dermatomal distribution bilaterally. Reflexes normal and equal bilaterally.
• Patient goals: Tolerate sustained postures for >1 hour. Return to full golf activities. Decrease pain level.
Evaluation
JD presents with joint dysfunction of the cervical spine with strain of soft tissue due to high velocity deceleration. Testing revealed decreased functional mobility due to limitations in range of motion ROM and strength with pain due to both strained soft tissue and impaired joint mobility with probable local inflammation.
Treatment diagnosis and Prognosis: Diagnosis for this athlete falls within Grade II WAD per clinical practice guidelines. Screening and manual therapy assessment did not denote fracture or medical complications, however, physician contacted to rule out fracture based upon radiological findings. Impaired joint mobility, motor function, muscle performance and range of motion associated with localized inflammation denote need for intervention. Function and mobility status were much greater prior to this acute incident. Patient was appropriate for PT treatment with good prognosis for recovery. Plan of care included treatment 2-3 times per week for 4 weeks (as most) to progress to off-season training regimen. Goals included restoration of full ROM and normal strength with recruitment of deep cervical stabilizers to enhance stability with upright postures.
Intervention
Coordination, communication, cocumentation: Communication with referring physician regarding the results of x-rays (negative) and outcome of MD prescribed MRI (negative) to rule out disk herniation.
| Table 1. Measures taken with inclinometer. Muscle testing (MMT)/strength testing inhibited by pain. |
|
Motion/Muscle
|
AROM |
PROM |
MMT-right |
MMT-left
|
|
Cerv.flexion
|
20 degrees |
45 degrees |
4/5 |
|
| Cerv. Extension |
10 degrees |
15 degrees |
4/5
|
|
|
Cerv. Rotation
|
40Right; 30 Left |
45Right; 37 Left |
4-/5 |
4-/5 |
| Cerv. SB right |
30 degrees |
30 degrees |
4-/5
|
4-/5
|
|
Cerv. SB left
|
30 degrees |
40 degrees |
4-/5 |
4-/5 |
| Shldr. Abd |
174 |
175 |
4-/5
|
4-/5
|
|
Lower Traps
|
WNL |
WNL |
4-/5 |
4-/5 |
Therapeutic Exercise/Functional Training
Week 1: Manual therapy: Soft tissue mobilization to deep anterior cervical mm, pericervical/periscapular musculature; joint oscillations to mid-cervical and muscle energy techniques to correct C1-C2, with manipulation of thoracic T3-T7. Education: Resting postures and pain management, use of ice and heat. Athlete had TENS unit and cleared to use as needed. Discontinuance of high level core training program, continued supported cardiovascular training on recumbent bike. No golf. Met at motion analysis bay to confirm “no golf ” when unable to maintain stance to demonstrate swing. Reviewed training schedule plan and competition plans for 1st quarter of year to demonstrate that rehabilitation time will still allow for time to prepare for season. Therapeutic exercise: Initiated activation of deep cervical mm without SCM/ant scalene recruitment taught during 1st visit. In supine, flattening of cervical lordosis indicative of recruitment of LCM. Isometrics: Persis capular musculature in supine with progression to standing with control of cervical compensatory motions. Gentle ANT stretching done for upper extremity.
Week 2: Written results and copies of X-rays and MRI (disk herniation/protrusion to left at C5-6-7) received. No treatment change, with increased education of athlete regarding prognosis. Continued STM to cervical musculature, athlete independent with flexibility and thoracic self-mobilizations. Restored: Full Active Rotation and SB in cervical region. Negative ANT. Therapeutic Exercise Progressed with inner core cervical training with sustained holds 10-30 seconds and isometrics to extension (added trunk core in supine with cervical supported postures: mat and ball). Taped in cervical/scapular neutral.
Week 3: Therapeutic exercise: Interval training on recumbent bike, upper extremity ergometer warm-up. Cervical eccentrics in sitting with sustained holds through range; prone unsupported static trunk/scapular stabilization added with cervical alignment emphasized. Neurodevelopment sequence for exercise progression as outlined by Morgan22 and Commeford and Mottram23 were followed. Full lower extremity gym program resumed.
Week 4: Therapeutic exercise: Supine cervical flexion without compensatory motions, end range perturbation added. Maintenance (1) visit with STM, modality of heat or ice prn and supervision core routine for technique corrections. Noted initiation of superficial muscles prior to deep cervical muscle recruitment with maximal contractions. Requires continued training for safe progression without exacerbation. Continued gym program with limitations, golf putting for 20 minutes, 30 minutes (alternate days). Restored: Full muscular strength (5/5) all motions.
Week 5: Gym and core routine without limitations. Assessment cervical recruitment-good. Chipping 20 minutes plus putts 15 minutes every other day. Approved custom pillow for travel. All PT goals met, released by MD. Per athlete request, continued maintenance, 1x per week, for enhancement of performance with fitness/ wellness visits and direction with progression of exercise program.
Week 6: Continued maintenance/gym program for strengthening. Progress through clubs-each iron 10 strokes, putt alternate days. Driver used on last day of week.
Week 7: Full session with swing coach: Continued progressive increase through off-season-2 weeks projected prior to competition.
Outcomes
Athlete returned to full competition/golf activities and played a successful year without exacerbation of cervical symptoms.
• Upper extremity strength 5/5, pain level 0/5
• Cervical and upper extremity passive and active ROM WNL
• Cervical joint mobility cleared of dysfunction
• Tolerated static postures and full training regimen w/o pain
• Independent with HEP for cervical stabilization exercise program, with postural correction and appropriate resting postures for cervical comfort.
CONCLUSION
Athlete attained full recovery to perform competitively without complications. Training regimen included high level of core stability training for the cervical and trunk region. This case demonstrates that though low-level evidence has been available to support clinical management guidelines for management of whiplash, clinicians can refer to these guidelines but must continue to rely on application of available evidence and clinical expertise for effective patient recovery.