INTRODUCTION
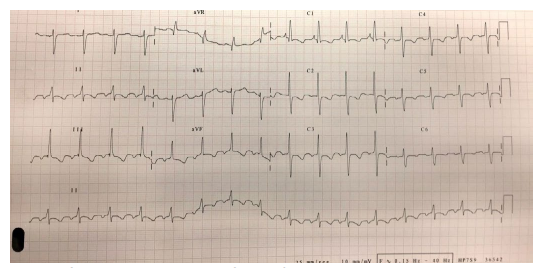
A 56-year-old woman with a past history of seronegative rheumatoid arthritis treated with leflunomide came to the Accident and Emergency (A&E) unit complaining of one month of shortness of breath, grade III New-York Heart Association (NYHA), and 48 hours of dysarthria and gait and postural instability causing several falls. Upon physical examination, we found a wide-based gait with negative Romberg test, dysarthria without language impairment and 2 heart murmurs: a systolic one around the tricuspid area and a holosystolic mitral-area localized. Computed-tomography (CT) scan showed a sub-acute infarct in the left superior cerebellarartery region. Laboratory results revealed an acute respiratory failure and an electrocardiogram (ECG) the following findings (Figure 1).
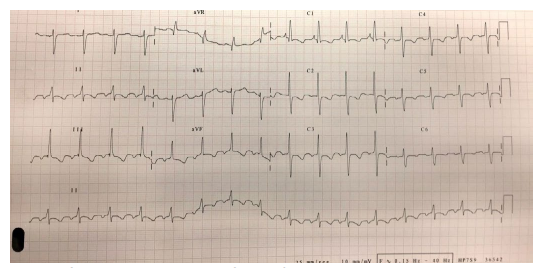
Figure 1: Sinus rhythm with right axis. Criteria of right ventricular hypertrophy and pulmonary hypertension with R-wave bigger than S-wave in V1 and V2 and deep S-wave in V5, V6, I and aVL. P-wave pulmonale. Secondary alterations in repolarization with ST and negative T wave in precordial and inferior leads
The patient underwent full assessment and an angio-CT scan was performed to rule out pulmonary embolism (PE) and interstitial lung disease (ILD). As well as the angio-CT scan, a supra aortic trunks doppler scan was normal. Transthoracic echocardiogram (TTE), however, estimated a systolic
pressure in pulmonary artery of 128 mmHg and the microbubble injection technique, the presence of bubbles in the atrium and left ventricle in the 1st 3 beats after opacification of the right cavities. These highly suggestive findings of patent foramen ovale (PFO) were confirmed by the right heart catheterization and defined as a PFO type interatrial communication. A lack of response to the acute vasodilatador test with epoprostenol and a right to left communication with a continuous shunt were observed. We closed the anatomic defect and started her on ambrisentan, tadalafil, aspirin and optimized her underlying rheumatic condition treatment.
DISCUSSION
Pulmonary hypertension (PH) is a disease characterized by elevated pulmonary artery pressure, which often results in right ventricular failure. It may be idiopathic, familial, or associated with multiple other diseases. PH occurs in men and women of any race or age. PH can be a progressive, fatal disease if untreated, although the rate of progression is highly variable.1 Interestingly, our patient reached an advanced end organ damage stage, but she tailored to her symptoms gradually. After diagnosis, patients with PH should be evaluated in a center with expertise in management of this disease.2
Primary or secondary PH classification no longer exists and a new one including 5 groups has been proposed by the World Health Organization (WHO).3 PH in our case caused right ventricular failure (represented in the TTE and ECG findings) and presented as an acute cerebellar syndrome due to a paradoxical cerebral stroke. Both PFO and aortic regurgitation (AR) were the causes of PH here. As the presence of advanced disease in PH is generally suggested to be less responsive to therapy, we do not expect in our case a great succes.4 A take-home message are the need of a proactive search of right ventricular overload findings in ECG and the clinical suspicion of PFO as the cause of an unexplained cerebral stroke.
CONCLUSIONS
PFO can cause a wide range of manifestations. Not always suspected in the A&E unit, we need to expand the awareness of this entity to general and junior doctors because the management and prognosis of the patients rely on a prompt and accurate response.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.