INTRODUCTION
Cystic lesions of the Brunner gland are rare. They have been referred to as Brunner’s gland cyst, cystic Brunner’s gland hamartoma, Brunner’s gland cystadenoma and mucocele of the Brunner gland. Recently these entities have been grouped under the term Brunner gland cyst. Even with these combined entities, there are only fourteen Brunner gland cysts reported in the English literature. We present two new cases of Brunner gland cyst and compared them to those previously reported. Their clinical presentation and similarities are summarized.
CASE PRESENTATIONS
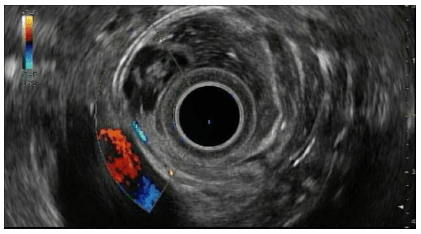
A 69-year-old Hispanic male was referred by his primary care physician to our institution for further studies of a duodenal lesion that was discovered after a workup for acid reflux. Endoscopic ultrasound showed a 17×6 mm septated cyst that appeared to arise from the submucosa of the second portion of the duodenum (Figures 1 and 2). No other abnormalities were noted. The cyst was resected after lifting the lesion with saline and methylene blue.
Figure 1: Radial EUS (7.5 MHz) of cystic duodenal Brunner gland cyst. Anechoic lesion in the deep mucosa/submucosa.
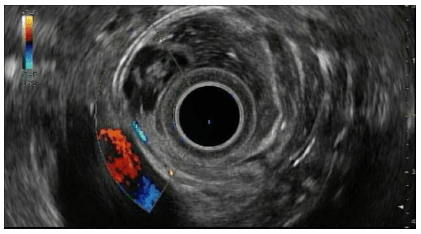
Figure 2: Endoscopic image of lobulated lesion in the second portion of the duodenum.

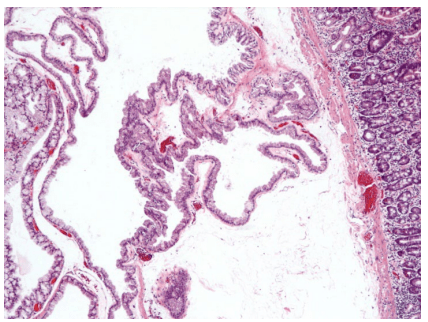
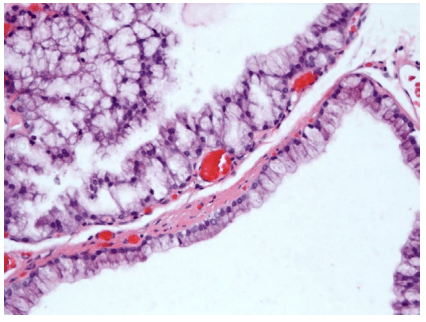
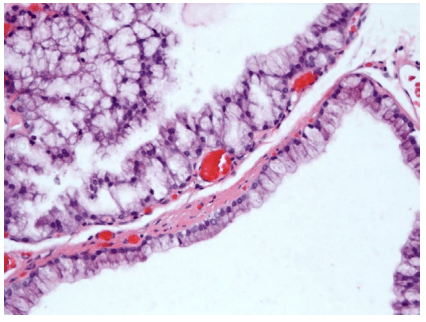
The specimen consisted of an ovoid lesion with a 0.5 cm cystic cavity. Microscopic examination revealed a submucosal multicystic lesion lined by tall, columnar cells with round basally located nuclei (Figures 3 and 4). Most of the cells had abundant clear cytoplasm similar to those seen in the adjacent normal Brunner glands. In other areas, the lining cells were smaller with pink cytoplasm. The cysts were filled with a serous-like fluid. Necrosis, mitotic activity, and nuclear atypia were absent. The cells contained neutral, Periodic Acid Schiff (PAS) positive mucin, similar to the adjacent Brunner’s glands.
Figure 3: Brunner gland cyst of the duodenum demonstrating multiple small cysts lined by fibrous septa (H&E, 100x).
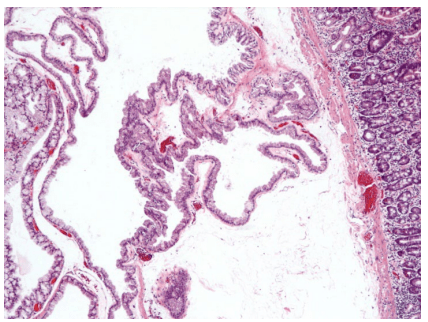
Figure 4: Brunner gland cyst of the duodenum lined by tall, columnar cells with round basally located nuclei (H&E, 400x).
The second patient is a 52-year-old Caucasian man referred to our institution because of epigastric pain and a duodenal mass found at endoscopy. Another endoscopy was performed along with endosonography. An intramural (subepithelial) lesion was found in the second portion of the duodenum. The lesion appeared to originate from within the submucosa (layer 3). The possibilities of pancreatic rest or Brunner’s gland hyperplasia were considered. The lesion was hypoechoic, heterogeneous and multicystic that measured 14.5 mm x 10.9 mm. The outer margins were well defined. An intact interface was seen between the mass and the adjacent structures suggesting a lack of invasion. An endomucosal resection of the mass was performed.
Histologically, the multicystic lesion was located in the submucosa of the duodenum and was composed of tall cells with basally located round nuclei. The cytoplasm was clear and abundant. In areas, there were aggregates of glands by the single row of epithelial cells lining the cysts creating a nodular configuration. No mitosis, necrosis or atypia was observed.
DISCUSSION
Rankin, et al. reported the first cystadenoma of the duodenum in 1933.1 Varnholt, et al. were the first to group Brunner gland cyst, Brunner cyst, mucocele of Brunner gland, and cystic Brunner’s gland hamartoma as one entity.2 Later, Powers, et al. added Brunner gland cystadenoma to this group.3 There are fourteen cases reported in the English literature.1,2,3,4,5,6,7,8,9,10,11,12 Information from these cases and the current two is summarized in Table 1.
| Table 1: Brunner gland cysts reported in the English literature: Patient characteristics, clinical presentation, diagnostic modality and lesion location, and histological characteristics. |
| Year |
Authors |
Diagnosis |
Age, Sex |
Clinical
presentation |
Location |
Size (cm) |
Architecture |
Depth |
# of cysts |
Histology characteristics |
| 2015 |
Moul, et al. (current case) |
Brunner gland cyst |
69, M |
Incidental finding in a patient with acid reflux |
Second portion of duodenum |
1.7 x 0.7 x 0.3 |
Sessile |
Sub-mucosa |
Single |
Focal eosinophilic cells |
| 2015 |
Moul, et al.
(current case) |
Brunner gland cyst |
52, M |
Epigastric pain |
Second portion of duodenum |
1.4 X 1.0 |
Polypoid |
Sub-mucosa |
Single |
Focal eosinophilic cells |
| 2011 |
Galiatsatos4 |
Brunner gland cyst |
72, M |
Incidental |
Distal end of the second part of the duodenum |
2 |
Polypoid |
Not specified |
Not specified |
Normal appearing duodenal mucosa and dilated lymphatic channels and capillaries (pictures not available for review) |
| 2009 |
Park, et al.5 |
Cystic Brunner’s gland hamartoma |
30, M |
Three-day history of nausea, vomiting, and epigastric pain. |
Third portion of the duodenum |
4 x 3 |
Pedunculated |
Sub-mucosa |
Multiple |
Lobular collection of mature Brunner’s glands, multifocal cystic dilation. |
| 2008 |
Powers, et al.3 |
Brunner gland cyst |
46, F |
Dyspepsia and odynophagia |
Two lesions located in the second part of the duodenum |
1.8 and 2.2 |
Sessile |
Sub-mucosa |
Single |
Cystic spaces lined by hyperplastic cells similar to Brunner glands cells. |
| 2008 |
Powers, et al.3 |
Brunner gland cyst |
67, F |
Incidental in a patient with unexplained iron-deficiency anemia |
Second part of the duodenum |
1.5 |
Sessile |
Sub-mucosa |
Single |
Cystic spaces lined by hyperplastic cells similar to Brunner glands cells. |
| 2008 |
Powers, et al.3 |
Brunner gland cyst |
59, F |
Incidental in a patient with abdominal pain, heartburn, steatorrhea |
Duodenal bulb (first portion) |
1.0 |
Nodule |
Sub-mucosa |
Single |
Cystic spaces lined by hyperplastic cells similar to Brunner glands cells. |
| 2007 |
Varnholt, et al.2 |
Brunner gland cyst |
41, F |
Incidental finding in a women being treated for H. pylori-associated gastritis. |
Not specified |
1.1 x 0.9 x 0.6 |
Sessile |
Sub-mucosa |
Single |
Cyst lined by a simple cuboidal-to-columnar epithelium. |
| 2003 |
Yamakawa, et al.6 |
Cystic Brunner’s gland hamartoma |
64, F |
Epigastric pain |
Descending duodenum (second portion) |
2.4 x 1.1 x .5 |
Pedunculated |
Sub-mucosa |
Multiple |
Multilocular cysts lined by columnar epithelium ; dilated ductal structures. |
| 2002 |
Chatelain, et al.7 |
Brunner gland hamartoma with predominant adipose tissue and ciliated cysts |
43, M |
Two-day history of regurgitation. |
Duodenal bulb (first portion) |
3.5 |
Pedunculated |
Sub-mucosa |
Multiple, ciliated |
Prominent mature adipose tissue, hyperplastic lobules of Brunner glands |
| 1980 |
Fisher8 |
Mucocele of Brunner gland |
45, F |
Right upper quadrant pain intermittently for two months |
Not specified |
Not specified |
Not specified |
Sub-mucosa |
Single |
Intact duodenal mucosa with prominently dilated glandular spaces, one being large and cystic. |
| 1978 |
Golan J, et al.9 |
Cystic Brunner’s gland hamartoma |
64, M |
Acute gastrointestinal bleeding; had a known duodenal polyp for 15 years |
First part of the duodenum. |
5 x 4 x 2 |
Pedunculated |
Sub-mucosa |
Multiple |
Cysts were lined by columnar and cuboidal epithelium. The surface epithelium was partly pyloric and partly duodenal. |
|
Taura M, et al.10 |
Brunner’s cyst |
54, F |
Nausea, vomiting, and epigastric pain for several days |
Duodenal bulb (first portion) |
1.5 |
Not specified |
Sub-mucosa |
Single |
Lined by tall columnar cells with basal nuclei. Multinucleated cells were intermingled with the epithelial lining cells. |
|
Wolk DP, et al.11 |
Brunner’s gland cystadenoma |
68, M |
Presented with 20 lb weight loss and eructation. |
Third portion of the duodenum, located on the posterior wall |
3 x 3 |
Not specified |
Sub-mucosa |
Multiple |
Multiple fluid-filled cystic spaces confined to the submucosa, lined by Brunner glands |
|
Hately12 |
Brunner’s gland cyst |
54, M |
Two year history of intermittent vomiting, now after every meal. |
First part of the duodenum. |
1.5 |
Sessile |
Sub-mucosa |
Single |
Cyst lined by columnar epithelium and had a direct origin from one of the Brunner glands. |
|
Rankin and Newell1 |
Simple, multilocular cystadenoma |
54, M |
18 m history of pernicious anemia and ulcer-like dyspepsia. |
– |
2 |
Not specified |
Sub-mucosa |
Multiple |
Cyst lined by cuboidal epithelial cells. |
Brunner gland cysts are benign, as evidenced by the fact that the lesion described by Golan, et al. was present for 15 years without any long-term consequences.9 They are widely believed to be retention cysts that develop after obstruction of a larger duct of the Brunner gland outflow tract.2
Based on this case and the well-described fourteen previously reported cases, the following conclusions can be made. The lesion can occur throughout the duodenum, specifically any place that contains Brunner glands. The large majority are single lesions with one patient reported to have two.3 Most of the lesions are pedunculated and located in the submucosa, but sessile lesions have been reported and one was transmural.8 While some are unilocular, others contain multiple cysts divided by fine septae. The cysts are lined by mucinous, columnar cells with basally located nuclei, resembling normal Brunner gland cells. Eosinophilic cells lining the cyst wall are also common. Only the case described by Chatelain, et al. showed ciliated columnar cells.7 Atypia is rare, and mitosis is only reported in one case.10 Ultrastructural studies performed by Taura, et al. in 1977 demonstrated epithelial cells containing membrane-bound secretory granules in the cytoplasm, mainly in the apical region, and a well-developed Golgi apparatus. The luminal surfaces contained microvilli. These features suggested that the cells of Brunner gland cysts were functionally more active than normal Brunner gland cells. Another distinct histological feature was the lack of neuroendocrine cells within the Brunner gland cysts, which is not true of normal Brunner’s glands.10
There is no sex predilection; fifty-three percent were male. The age range was 30 to 72 years of age, with the average being 55 years. The lesions ranged from 1 to 5 cm in size, the average being 2.3 cm in greatest dimension. While increased size correlated with more clinical symptoms, the patient with the largest reported lesion was not symptomatic from the lesion but from an adjacent ulcer.9 Nonetheless, most clinical symptoms are regurgitation, vomiting, and epigastic pain. However, it may be discovered incidentally for unrelated symptoms. Most often, the lesions are located in either the first or second portion of the duodenum. This corresponds to the most common locations of the Brunner’s gland, which are mostly concentrated in the first portion and gradually decrease in number throughout the length of the duodenum.13
The differential diagnosis on endoscopic imaging includes duplication cysts, lipomas, neuroendocrine tumors and Brunner gland hamartomas. Using endoscopic ultrasound it is possible to differentiate the echostructure (cystic, solid, hypo- or hyperechoic) and wall layer of involvement. The differential diagnosis of hypoechoic/anechoic duodenal lesions would be mainly duplication cysts, stromal cell tumors and neuroendocrine tumors. Our first patient underwent resection to ensure his was not a cystic neuroendocrine lesion. Histologically the main differential diagnosis is Brunner’s gland hamartoma, formerly known as Brunner’s gland adenoma. These lesions are admixtures of Brunner’s glands, ducts, adipose tissue and lymphoid tissue. While their ducts may be dilated, cystic lesions are not characteristic of this entity.14
Brunner gland cysts are rare benign lesions of the duodenum. The treatment is surgical excision or polypectomy. Increased awareness of these lesions helps for a better recognition of this entity.
CONFLICTS OF INTEREST: None.
DISCLOSURES
No consent is required to our article publication referenced above.