1. Malaisse WJ. Hormonal and environmental modification of islet activity. In: Steiner DF, Frankel N, eds. Handbook of physiology. New York: American Physiological Society. 1972; 237-260.
2. Prentki M, Matschinsky FM. Calcium, cAMP, and phospholipid-derived messengers in coupling mechanisms of insulin secretion. Physiol Rev. 1987; 67: 1185-1248. doi: 10.1152/physrev.1987.67.4.1185
3. MacDonald MJ. Elusive proximal signals of β-cells for insulin secretion. Diabetes. 1990; 39: 1461-1466. doi: 10.2337/diab.39.12.1461
4. Laychock SG. Glucose metabolism, second messengers and insulin secretion. Life Sci. 1990; 47: 2307-2316. doi: 10.1016/0024-3205(90)90269-w
5. Newgard CB, McGarry JD. Metabolic coupling factors in pancreatic beta-cell signal transduction. Annu Rev Biochem. 1995; 64: 689-719. doi: 10.1146/annurev.bi.64.070195.003353
6. Deeney JT, Prentki M, Corkey BE. Metabolic control of β-cell function. Semin Cell Dev Biol. 2000; 11: 267-275. doi: 10.1006/scdb.2000.0175
7. Newgard CB, Lu D, Jensen MV, et al. Stimulus/secretion coupling factors in glucose-stimulated insulin secretion: insights gained from a multidisciplinary approach. Diabetes. 2002; 51(3): S389-S393. doi: 10.2337/diabetes.51.2007.S389
8. Berggren PO, Leibiger IB. Novel aspects on signal transduction in the pancreatic β cell. Nutr Metab Cardiovasc Dis. 2006; 16(1): S7-S10. doi: 10.1016/j.numecd.2005.11.005
9. Metz SA. Membrane phospholipid turnover as an intermediary step in insulin secretion.Putative roles of phospholipases in cell signaling. Am J Med. 1988; 85: 9-21. doi: 10.1016/0002-9343(88)90393-2
10. Metz SA. The pancreatic islet as a Rubik’s cube. Is phospholipid hydrolysis a piece of the puzzle? Diabetes. 1991; 40: 1565-1573. doi: 10.2337/diab.40.12.1565
11. Lawrence M, Shao C, Duan L, McGlynn K, Cobb MH. The protein kinases ERK1/2 and their roles in pancreatic β cells. Acta Physiol (Oxf). 2008; 192: 11-17. doi: 10.1111/j.1748-1716.2007.01785.x
12. Lang J. Molecular mechanisms and regulation of insulin exocytosis as a paradigm of endocrine secretion. Eur J Biochem. 1999; 259: 3-17. doi: 10.1046/j.1432-1327.1999.00043.x
13. Poitout V. Phospholipid hydrolysis and insulin secretion: a step toward solving the Rubik’s cube. Am J Physiol Endocrinol Metab. 2008; 294: E214-E216. doi: 10.1152/ajpendo.00638.2007
14. Metz SA, Rabaglia ME, Pintar TJ. Selective inhibitors of GTP synthesis impede exocytotic insulin release from intact rat islets. J Biol Chem. 1992; 267: 12517-12527.
15. Metz SA, Meredith M, Rabaglia ME, Kowluru A. Small elevations of glucose concentration redirect and amplify the synthesis of guanosine 5-triphosphate in rat islets. J Clin Invest. 1993; 92: 872-882. doi: 10.1172/JCI116662
16. Komatsu M, Noda M, Sharp GW. Nutrient augmentation of Ca2-dependent and Ca2+-independent pathways in stimulus-coupling to insulin secretion can be distinguished by their guanosine triphosphate requirements: studies on rat pancreatic islets. Endocrinology. 1998; 139: 1172-1183. doi: 10.1210/endo.139.3.5859
17. Straub SG, James RF, Dunne MJ, Sharp GW. Glucose augmentation of mastoparan stimulated insulin secretion in rat and human pancreatic islets. Diabetes. 1998; 47: 1053-1057. doi: 10.2337/diabetes.47.7.1053
18. Kowluru A, Seavey SE, Li G, et al. Glucose- and GTP-dependent stimulation of the carboxylmethylation of Cdc42 in rodent and human pancreatic islets and pure β cells: evidence for an essential role for GTP-binding proteins in nutrient-induced insulin secretion. J Clin Invest. 1996; 98: 540-555. doi: 10.1172/JCI118822
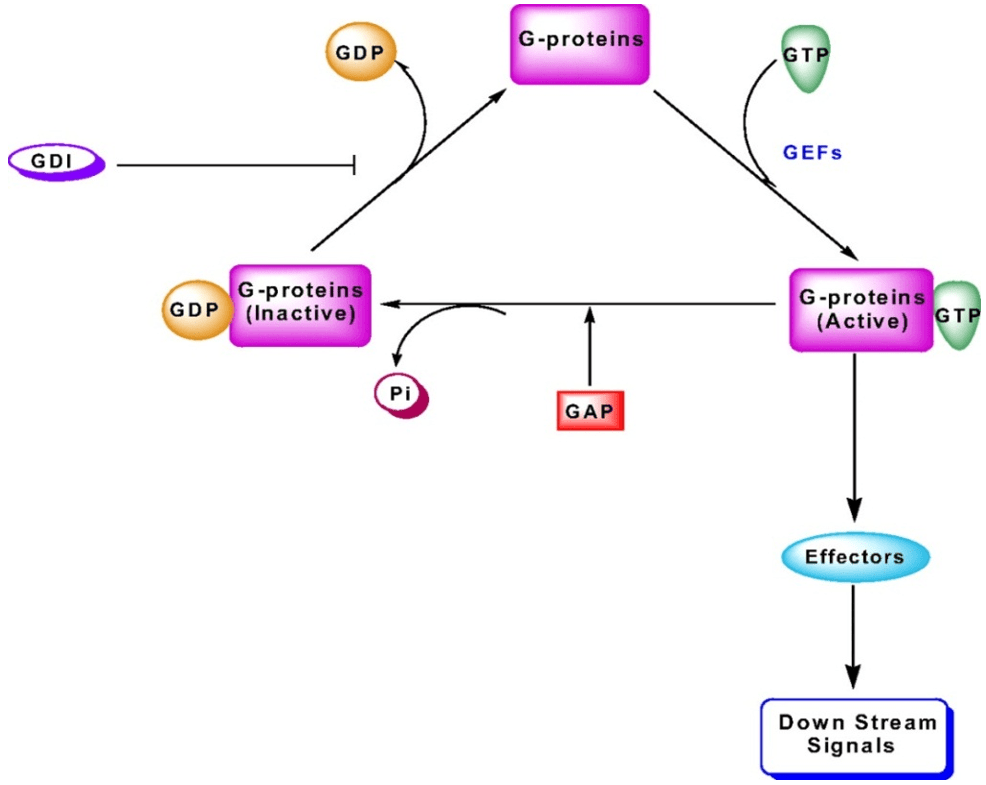
19. Kowluru A. Regulatory roles for small G-proteins in the pancreatic β cell: lessons from models of impaired insulin secretion. Am J Physiol Endocrinol Metab. 2003; 285: E669-E684. doi: 10.1152/ajpendo.00196.2003
20. Wang Z, Thurmond DC. Mechanisms of biphasic insulin-granule exocytosis- roles of the cytoskeleton, small GTPases and SNARE proteins. J Cell Sci. 2009; 122: 893-903. doi: 10.1242/jcs.034355
21. Robertson RP, Seaquist ER, Walseth TF. G proteins and modulation of insulin secretion. Diabetes. 1991; 40: 1-6. doi: 10.2337/diab.40.1.1
22. Seaquist ER, Walseth TF, Redmon JB, Robertson RP. G-protein regulation of insulin secretion. J Lab Clin Med. 1994; 123: 338-345. doi: 10.2337/diab.40.1.1
23. Gilman AG. G proteins: transducers of receptor-generated signals. Annu Rev Biochem.1987; 56: 615-649. doi: 10.1146/annurev.bi.56.070187.003151
24. Birnbaumer L. Receptor-to-effector signaling through G proteins: roles for beta gamma dimers as well as α subunits. Cell. 1992; 71: 1069-1072. doi: 10.1016/S0092-8674(05)80056-X
25. Clapham DE, Neer EJ. New roles for G-protein βγ-dimers in transmembrane signaling. Nature. 1993; 365: 403-406. doi: 10.1038/365403a0
26. Takai Y, Sasaki T, Matozaki T. Small GTP-binding proteins. Physiol Rev. 2001; 81: 153-208. doi: 10.1152/physrev.2001.81.1.153
27. Casey PJ, Seabra MC. Protein prenyltransferases. J Biol Chem. 1996; 271: 5289-5292. doi: 10.1074/jbc.271.10.5289
28. Maurer-Stroh S, Washietl S, Eisenhaber F. Protein prenyltransferases. Genome Biol. 2003; 4: 212.1-212.9. doi: 10.1186/gb-2003-4-4-212
29. Seabra MC, Reiss Y, Casey PJ, Brown MS, Goldstein JL. Protein farnesyltransferase and geranylgeranyltransferase share a common α subunit. Cell. 1991; 65: 429-434. doi: 10.1016/0092-8674(91)90460-G
30. Fu HW, Casey PJ. Enzymology and biology of CaaX protein prenylation. Rec ProgHorm Res. 1999; 54: 315-342.
31. Veluthakal R, Kaur H, Goalstone M, Kowluru A. Dominant negative-subunit of farnesyl-and geranylgeranyltransferase inhibits glucose-stimulated, but not KCl stimulated, insulin secretion in INS 832/13 cells. Diabetes. 2007; 56: 204-210. doi: 10.2337/db06-0668
32. Kowluru A, Li G, Rabaglia ME, et al. Evidence for differential roles of the Rho subfamily of GTP-binding proteins in glucose- and calcium-induced insulin secretion from pancreatic β cells. Biochem Pharmacol. 1997; 54: 1097-1108. doi: 10.1016/S0006-2952(97)00314-6
33. Regazzi R, Kikuchi A, Takai Y, Wollheim CB. The small GTP-binding proteins in the cytosol of insulin-secreting cells are complexed to GDP dissociation inhibitor proteins. J Biol Chem. 1992; 267: 17512-17519. doi: 10.1016/S0021-9258(19)37072-3
34. Kowluru A, Rabaglia ME, Muse KE, Metz SA. Subcellular localization and kinetic characterization of guanine nucleotide binding proteins in normal rat and human pancreatic islets and transformed β cells. Biochim Biophys Acta. 1994; 1222: 348-359. doi: 10.1016/0167-4889(94)90040-x
35. Daniel S, Noda M, Cerione RA, Sharp GW. A link between Cdc42 and syntaxin is involved in mastoparan stimulated insulin release. Biochemistry. 2002; 41: 9663-9671. doi: 10.1021/bi025604p
36. Kowluru A, Chen HQ, Tannous M. Novel roles for the Rho subfamily of GTP-binding proteins in succinate induced insulin secretion from β TC3 cells: further evidence in support of succinate mechanism of insulin release. Endocr Res. 2003; 29: 363-376. doi: 10.1081/erc-120025043
37. Nevins AK, Thurmond DC. Glucose regulates the cortical actin network through modulation of Cdc42 cycling to stimulate insulin secretion. Am J Physiol Cell Physiol. 2003; 285: C698-C710. doi: 10.1152/ajpcell.00093.2003
38. Nevins AK, Thurmond DC. A direct interaction between Cdc42 and vesicle-associated membrane protein 2 regulates SNARE-dependent insulin exocytosis. J Biol Chem. 2005; 280: 1944-1952. doi: 10.1074/jbc.m409528200
39. Nevins AK, Thurmond DC. Caveolin-1 functions as a novel Cdc42 guanine nucleotide dissociation inhibitor in pancreatic β-cells. J Biol Chem. 2006; 281: 18961-18972. doi: 10.1074/jbc.M603604200
40. Wang Z, Oh E, Thurmond DC. Glucose-stimulated Cdc42 signaling is essential for the second phase of insulin secretion. J Biol Chem. 2007; 282: 9536-9546. doi: 10.1074/jbc.M610553200
41. Li J, Luo R, Kowluru A, Li G. Novel regulation by Rac1 of glucose-and forskolin-induced insulin secretion in INS-1 β cell. Am J Physiol Endocrinol Metab. 2004; 286: E818-E827. doi: 10.1152/ajpendo.00307.2003
42. McDonald P, Veluthakal R, Kaur H, Kowluru A. Biologically active lipids promote trafficking and membrane association of Rac1 in insulin-secreting INS832/13 cells. Am J Physiol Cell Physiol. 2007; 292: C1216-C1220. doi: 10.1152/ajpcell.00467.2006
43. Asahara A, Kido Y, Shigeyama Y, et al. Rac1 regulates glucose induced insulin secretion through modulation of cytoskeletal organization in β cells. Diabetes. 2008; 57(1): A55.
44. Greiner TU, Kesavan G, Ståhlberg A, Semb H. Rac1 regulates pancreatic islet morpholgenesis. BMC Dev Biol. 2009; 9: 2. doi: 10.1186/1471-213X-9-2
45. Kowluru A, Amin R. Inhibitors of post-translational modifications of G-proteins as probes to study the pancreatic beta cell function: potential therapeutic implications. Curr Drug Targets Immune Endocr Metabol Disord. 2002; 2: 129-139. doi: 10.2174/1568008023340668
46. Lawrence JT, Birnbaum MJ. ADP-ribosylation factor 6 regulates insulin secretion through plasma membrane phosphatidylinositol 4,5-bisphosphate. Proc Natl Acad Sci. 2003; 100: 13320-13325. doi: 10.1073/pnas.2232129100
47. Grodnitzky JA, Syed N, Kimber MJ, Day TA, Donaldson JG, Hsu WH. Somatostatin receptors signal through EFA6A-ARF6 to activate phospholipase D in clonal β-cells. J Biol Chem. 2007; 282: 13410-13418. doi: 10.1074/jbc.M701940200
48. Hammar E, Tomas A, Bosco D, Halban PA. Role of the Rho-ROCK (Rho-associated kinase) signaling pathway in the regulation of pancreatic-cell function. Endocrinology. 2009; 150: 2072-2079. doi: 10.1210/en.2008-1135
49. Kowluru A. Small G proteins in islet beta-cell function. Endocr Rev. 2010; 31: 52-78. 10.1210/er.2009-0022
50. Graciano MF, Santos LR, Curi R, Carpinelli AR. NAD(P)H oxidase participates in the palmitate-induced superoxide production and insulin secretion by rat pancreatic islets. J Cell Physiol. 2011; 226(4): 1110-1117. doi: 10.1002/jcp.22432
51. Buffa L, Fuchs E, Pietropaolo M, Barr F, Solimena M. ICA69 is a novel Rab2 effector regulating ER-Golgi trafficking in insulinoma cells. Eur J Cell Biol. 2008; 87: 197-209. doi: 10.1016/j.ejcb.2007.11.003
52. Chan SL, Monks LK, Gao H, Deaville P, Morgan NG. Identification of the monomeric G-protein, Rhes, as an efaroxan-regulated protein in the pancreatic β-cell. Br J Pharmacol. 2002; 136: 31-36. doi: 10.1038/sj.bjp.0704680
53. Sharoyko VV, Zaitseva II, Varsanyi M, et al. Monomeric G-protein, Rhes, is not an imidazolineregulated protein in pancreatic β-cells. Biochem Biophys Res Commun. 2005; 338: 1455-1459. doi: 10.1016/j.bbrc.2005.10.145
54. Taylor JP, Jackson DA, Morgan NG, Chan SL. Rhes expression in pancreatic β-cells is regulated by efaroxan in a calcium-dependent process. Biochem Biophys Res Commun. 2006; 349: 809-815. doi: 10.1016/j.bbrc.2006.08.102
55. Lopez JA, Kwan EP, Xie L, He Y, James DE, Gaisano HY. The RalAGTPase is a central regulator of insulin exocytosis from pancreatic islet cells. J Biol Chem. 2008; 283: 17939-17945. doi: 10.1074/jbc.M800321200
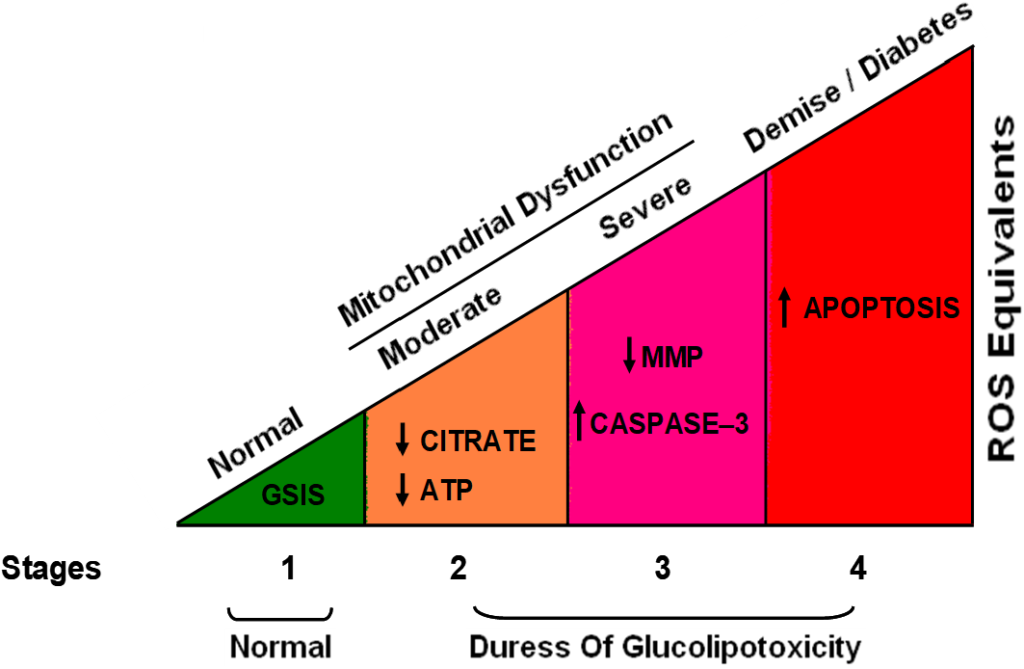
56. Syed I, Jayaram B, Subasinghe W, Kowluru A. Tiam1/Rac1 signaling pathway mediates palmitate-induced, ceramide-sensitive generation of superoxides and lipid peroxides and the loss of mitochondrial membrane potential in pancreatic beta-cells. Biochem Pharmacol. 2010; 80: 874-883. doi: 10.1016/j.bcp.2010.05.006
57. Syed I, Kyathanahalli CN, Jayaram B, et al. Increased Phagocyte-Like NADPH Oxidase and ROS Generation in Type 2 Diabetic ZDF Rat and Human Islets. Diabetes. 2011; 60: 2843-2852. doi: 10.2337/db11-0809
58. Didsbury J, Weber RF, Bokoch GM, Evans T, Snyderman R. Rac, a novel ras-related family of proteins that are botulinum toxin substrates. J Biol Chem. 1989; 264(28): 16378-16382.
59. Wang Z, Pedersen E, Basse A, et al. Rac1 is crucial for Ras-dependent skin tumor formation by controlling Pak1-Mek-Erk hyperactivation and hyperproliferation in vivo. Oncogene. 2010; 29: 3362-3373. doi: 10.1038/onc.2010.95
60. Sosa MS, Lopez-Haber C, Yang C, et al. Identification of the Rac-GEF P-Rex1 as an essential mediator of ErbB signaling in breast cancer. Mol Cell. 2010; 40: 877-892. doi: 10.1016/j.molcel.2010.11.029
61. Hayashi-Takagi A, Takaki M, Graziane N, et al. Disruptedin-Schizophrenia 1 (DISC1) regulates spines of the glutamate synapse via Rac1. Nat Neurosci. 2010; 13: 327-332. doi: 10.1038/nn.2487
62. Bopp A, Wartlick F, Henninger C, Kaina B, Fritz G. Rac1 modulates acute and subacutegenotoxin-induced hepatic stress responses, fibrosis and liver aging. Cell Death and Disease. 2013; 4: e558. doi: 10.1038/cddis.2013.57
63. JeBailey L, Wanono O, Niu W, Roessler J, Rudich A, Klip A. Ceramide-and oxidant-induced insulin resistance involve loss of insulin-dependent Rac-activation and actin remodeling in muscle cells. Diabetes. 2007; 56: 394-403. doi: 10.2337/db06-0823
64. Ueda S, Kitazawa S, Ishida K. Crucial role of the small GTPase Rac1 in insulin-stimulated translocation of glucose transporter 4 to the mouse skeletal muscle sarcolemma. FASEB J. 2010; 24: 2254-2261. doi: 10.1096/fj.09-137380
65. Iizuka M, Konno S. Wound healing of intestinal epithelialcells. World J Gastroenterol. 2011; 17: 2161-2171. doi: 10.3748/wjg.v17.i17.2161
66. Babbin BA, Jesaitis AJ, Ivanov AI, et al. Formylpeptide receptor-1 activation enhances intestinal epithelialcell restitution through phosphatidylinositol3-kinase-dependent activation of Rac1 and Cdc42. J Immunol. 2007; 179: 8112-8121. doi: 10.4049/jimmunol.179.12.8112
67. Lemichez E, Aktories K. Hijacking of Rho GTPasesduring bacterial infection. Exp Cell Res. 2013; 319: 2329-2336. doi: 10.1016/j.yexcr.2013.04.021
68. Citalán-Madrid AF, García-Ponce A, Vargas-Robles H, Betanzos A, Schnoor M. Small GTPases of the Ras superfamily regulateintestinal epithelial homeostasis and barrierfunction via common and unique mechanisms. Tissue Barriers. 2013; 1: e26938: 1-28. doi: 10.4161/tisb.26938
69. Kowluru A. Friendly, and not so friendly, roles of Rac1 in islet β-cell function: lessons learnt from pharmacological and molecular biological approaches. Biochem Pharmacol. 2011; 81(8): 965-975. doi: 10.1016/j.bcp.2011.01.013
70. Benitah SA, Frye M, Glogauer M, Watt FM. Stem cell depletion through epidermal deletion of Rac1. Science. 2005; 309: 933-935. doi: 10.1126/science.1113579
71. Asahara S, Shibutani Y, Teruyama K, et al. Ras-related C3 botulinum toxin substrate 1 (RAC1) regulates glucose-stimulated insulin secretion via modulation of F-actin. Diabetologia. 2013; 56: 1088-1097. doi: 10.1007/s00125-013-2849-5
72. Pi J, Collins S. Reactive oxygen species and uncoupling protein 2 in pancreatic β-cell function. Diabetes Obes Metab. 2010; 12(2): 141-148. doi: 10.1111/j.1463-1326.2010.01269.x
73. Graciano MF, Santos LR, Curi R, Carpinelli AR. NAD(P)H oxidase participates in the palmitate-induced superoxide production and insulin secretion by rat pancreatic islets. J Cell Physiol. 2011; 226(4): 1110-1117. doi: 10.1002/jcp.22432
74. Newsholme P, Morgan D, Rebelato E, et al. Insights into the critical role of NADPH oxidase(s) in the normal and dysregulated pancreatic beta cell. Diabetologia. 2009; 52: 2489-2498. doi: 10.1007/s00125-009-1536-z
75. Oliveira HR, Verlengia R, Carvalho CR, Britto LR, Curi R, Carpinelli AR. Pancreatic beta cells express phagocyte-like NADPH oxidase. Diabetes. 2003; 52: 1457-1463. doi: 10.2337/diabetes.52.6.1457
76. Pi J, Bai Y, Zhang Q, et al. Reactive oxygen species as a signal in glucose-stimulated insulin secretion. Diabetes. 2007; 56: 1783-1791. doi: 10.2337/db06-1601
77. Krause KH. Tissue distribution and putative physiological function of NOX family NADPH oxidases. Jpn J Infect Dis. 2004; 57(5): S28-S29.
78. Geiszt M. NADPH oxidases: new kids on the block. Cardiovasc Res. 2006; 71: 289-299. doi: 10.1016/j.cardiores.2006.05.004
79. Bedard K, Krause KH. The NOX family of ROS generating NADPH oxidases: physiology and pathophysiology. Physiol Rev. 2007; 87: 245-313. doi: 10.1152/physrev.00044.2005
80. Banfi B, Maturana A, Jaconi S, et al. A mammalian H+ channel generated through alternative splicing of the NADPH oxidase homolog NOH-1. Science. 2000; 287(5450): 138-142. doi: 10.1126/science.287.5450.138
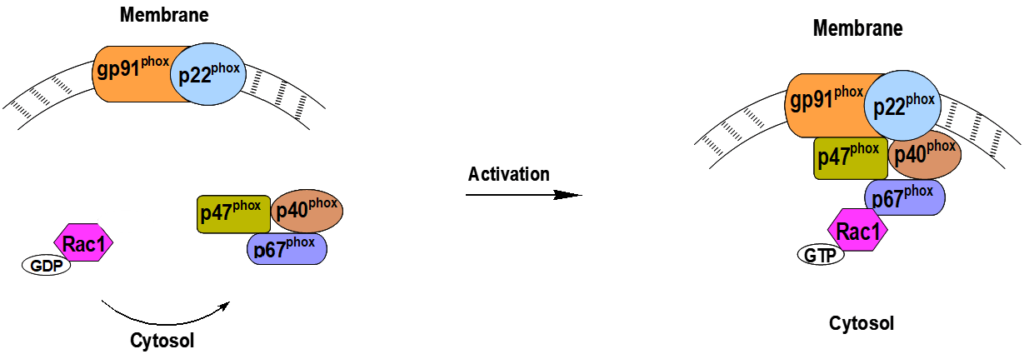
81. Sumimoto H, Miyano K, Takeya R. Molecular composition and regulation of the Nox family NAD(P)H oxidases. Biochem Biophys Res Commun. 2005; 338: 677-686. doi: 10.1016/j.bbrc.2005.08.210
82. Cheng G, Diebold BA, Hughes Y, Lambeth JD. Nox1-dependent reactive oxygen generation is regulated by Rac1. J Biol Chem. 2006; 281: 17718-17726. doi: 10.1074/jbc.M51275120
83. Martyn KD, Frederick LM, von Loehneysen K, Dinauer MC, Knaus UG. Functional analysis of Nox4 reveals unique characteristics compared to other NADPH oxidases. Cell Signal. 2006; 18: 69-82. doi: 10.1016/j.cellsig.2005.03.023
84. Hordijk PL. Regulation of NADPH oxidases: the role of Rac proteins. Circ Res. 2006; 98: 453-462. doi: 10.1161/01.res.0000204727.46710.5e
85. Abo A, Pick E, Hall N, Totty N, Teahan CG, Segal AW. Activation of the NADPH oxidase involves the small-GTP binding protein p21rac1. Nature. 1991; 353: 668-670. doi: 10.1038/353668a0
86. Knaus UG, Heyworth PG, Evans T, Curnutte JT, Bokoch GM. Regulation of phagocyte oxygen radical production by the GTP-binding protein Rac 2. Science. 1991; 254: 1512-1515. doi: 10.1126/science.1660188
87. Babior BM. NADPH oxidase: an update. Blood. 1999; 93(5): 1464-1476.
88. Borregaard N, Tauber AI. Subcellular localization of the human neutrophil NADPH oxidase b-cytochrome and associated flavoprotein. J Biol Chem. 1984; 259(1): 47-52.
89. Gorzalczany Y, Sigal N, Itan M, Lotan O, Pick E. Targeting of Rac1 to the phagocyte membrane is sufficient for the induction of NADPH oxidase assembly. J Biol Chem. 2000; 275(1): 40073-40081. doi: 10.1074/jbc.M006013200
90. Morgan D, Rebelato E, Abdulkader F, et al. Association of NAD(P)H oxidase with glucose-induced insulin secretion by pancreatic beta-cells. Endocrinology. 2009; 150(5): 2197-2201. doi: 10.1210/en.2008-1149
91. Syed I, Kyathanahalli CN, Kowluru A. Phagocyte-like NADPH oxidase generates ROS in INS 832/13 cells and rat islets: role of protein prenylation. Am J Physiol Regul Integr Comp Physiol. 2011; 300(3): R756-R762. doi: 10.1152/ajpregu.00786.2010
92. Uchizono Y, Takeya R, Iwase M, et al. Expression of isoforms of NADPH oxidase components in rat pancreatic islets. Life Sci. 2006; 80(2): 133-139. doi: 10.1016/j.lfs.2006.08.031
93. Shen E, Li Y, Li Y, et al. Rac1 is required for cardiomyocyte apoptosis during hyperglycemia. Diabetes. 2009; 58(10): 2386-2395. doi: 10.2337/db08-0617
94. Subasinghe W, Syed I, Kowluru A. Phagocyte-like NADPH oxidase promotes cytokine-induced mitochondrial dysfunction in pancreatic β-cells: evidence for regulation by Rac1. Am J Physiol Regul Integr Comp Physiol. 2011; 300: R12-R20. doi: 10.1152/ajpregu.00421.2010
95. Veluthakal R, Madathilparambil SV, McDonald P, Olson LK, Kowluru A. Regulatory roles for Tiam1, a guanine nucleotide exchange factor for Rac1, in glucose-stimulated insulin secretion in pancreatic beta-cells. Biochem Pharmacol. 2009; 77: 101-113. doi: 10.1016/j.bcp.2008.09.021
96. Kowluru RA, Kowluru A, Veluthakal R, et al. TIAM1-RAC1 signalling axis-mediated activation of NADPH oxidase-2 initiates mitochondrial damage in the development of diabetic retinopathy. Diabetologia. 2014; 57(5): 1047-1056. doi: 10.1007/s00125-014-3194-z
97. Sidarala V, Veluthakal R, Syeda K, Vlaar C, Newsholme P, Kowluru A. Phagocyte-like NADPH oxidase (Nox2) promotes activation of p38MAPK in pancreatic β-cells under glucotoxic conditions: evidence for a requisite role of Ras-related C3 botulinum toxin substrate 1 (Rac1). Biochem Pharmacol. 2015. doi: 10.1016/j.bcp.2015.04.001
98. Zhou S, Yu D, Ning S, et al. Augmented Rac1 Expression and Activity are Associated with Oxidative Stress and Decline of β Cell Function in Obesity. Cell Physiol Biochem. 2015; 35: 2135-2148. doi: 10.1159/000374019
99. El-Benna J, Dang PM, Périanin A. Peptide-based inhibitors of the phagocyte NADPH oxidase. Biochem Pharmacol. 2010; 80(6): 778-785. doi: 10.1016/j.bcp.2010.05.020
100. Mizrahi A, Berdichevsky Y, Casey PJ, Pick E. The quintessential NADPH oxidase activator: a prenylated p47PHOX-p67PHOX-Rac1 chimera – membrane association and functional capacity. J Biol Chem. 2010; 285(33): 25485-25499. doi: 10.1074/jbc.M110.113779
101. Acharya JD, Ghaskadbi SS. Islets and their antioxidant defense. Islets. 2010; 2: 225-235. doi: 10.4161/isl.2.4.12219
102. Jacob S, Ruus P, Hermann R, et al. Oral administration of RAC-alpha-lipoic acid modulates insulin sensitivity in patients with type-2 diabetes mellitus: a placebo-controlled pilot trial. Free Radic. Biol. Med. 1999; 27: 309-314. doi: 10.1016/S0891-5849(99)00089-1
103. Sena CM, Nunes E, Gomes A, et al. Supplementation of coenzyme Q10 and alpha-tocopherol lowers glycated hemoglobin level and lipid peroxidation in pancreas of diabetic rats. Nutr. Res. 2008; 28: 113-121. doi: 10.1016/j.nutres.2007.12.005
104. Asayama K, Kooy NW, Burr IM. Effect of vitamin E deficiency and selenium deficiency on insulin secretory reserve and free radical scavenging systems in islets: decrease of islet manganosuperoxide dismutase. J. Lab. Clin. Med. 1986; 107: 459-464.
105. Xiao C, Giacca A, Lewis GF. Oral taurine but not N-acetylcysteine ameliorates NEFA-induced impairment in insulin sensitivity and β-cell function in obese and overweight, non-diabetic men. Diabetologia. 2008; 51: 139-146. doi: 10.1007/s00125-007-0859-x
106. Veluthakal R, Palanivel R, Zhao Y, McDonald P, Gruber S, Kowluru A. Ceramide induces mitochondrial abnormalities in insulin-secreting INS-1 cells: potential mechanisms underlying ceramide-mediated metabolic dysfunction of the beta cell. Apoptosis. 2005; 10: 841-850. doi: 10.1007/s10495-005-0431-4
107. Decorde K, Teissedre PL, Sutra T, Ventura E, Cristo JP, Rouanet JM. Chardonnay grape seed procyaidin extract supplementation prevents high-fat diet-induced obesity in hamsters by improving adipokine imbalance and oxidative stress markers. Mol Nutr Food Res. 2009; 53: 659-666. doi: 10.1002/mnfr.200800165
108. Kaneto H, Nakatani Y, Kawamori D, et al. Role of oxidative stress, endoplasmic reticulum stress, and c-Jun N-terminal kinase in pancreatic β-cell dysfunction and insulin resistance. Int J Biochem Cell Biol. 2006; 38: 782-793. doi: 10.1016/j.biocel.2006.01.004
109. de la Rosa LC, Vrenken TE, Hannivoort RA, et al. Carbon monoxide blocks oxidative stress-induced hepatocyte apoptosis via inhibition of the p54 JNK isoform. Free Radic Biol Med. 2007; 44: 1323-1333. doi: 10.1016/j.freeradbiomed.2007.12.011
110. Mosen H, Salehi A, Alm P, et al. Defective glucose-stimulated insulin release in the diabetic Goto-Kakizaki rat coincides with reduced activity of the islet carbon monoxide signaling pathway. Endocrinology. 2005; 146: 1553-1558. doi: 10.1210/en.2004-0851
111. Mosen H, Salehi A, Henningsson R, Lundquist I. Nitric oxide inhibits, and carbon monoxide activates, islet acid α-glucoside hydrolase activites in parallel with glucose-stimulated insulin secretion. J Endocrinol. 2006; 190: 681-693. doi: 10.1677/joe.1.06890
112. Nakayama M, Inoguchi T, Sonta T, et al. Increased expression of NAD(P)H oxidase in islets of animal models of Type 2 diabetes and its improvement by an AT1 receptor antagonist. Biochem Biophys Res Commun. 2005; 332(4): 927-933. doi: 10.1016/j.bbrc.2005.05.065
113. Ismail S. Mechanisms of regulation of islet function by NADPH oxidase. Diss. Wayne State University, 2011.