CASE REPORT
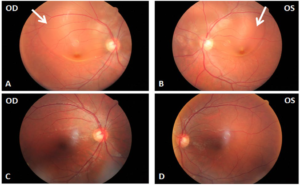
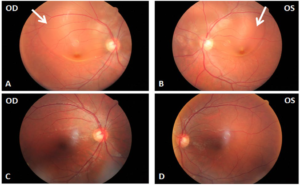
A 30-year-old caucasian primigravida was diagnosed with arterial hypertension at 34 weeks of gestation. At 36th week, labor induction was performed for severe preeclampsia. During labor, blood pressure was controlled with labetalol and convulsion prophylaxis was performed with magnesium sulfate. She had a vaginal delivery without complications and forty-eight hours later complained of intense fronto-occipital headache, blurred vision and metamorphopsia with a sudden decrease in visual acuity. Blood pressure during the postpartum period was 170/110 mm Hg. Blood samples showed no abnormalities. The previous ocular history was unremarkable. The patient was transferred from a secondary to a tertiary hospital in order to have an adequate ophthalmologic evaluation that revealed visual acuity of 2/10 and 4/10 in the right and left eye, respectively. Fundoscopy, retinography (Figures 1A and 1B) and Optical Coherence Tomography (OCT) showed bilateral bullous retinal detachment of the posterior pole with no hemorrhage or retinal exudates and also contributed to exclude the presence of a macular hole in both eyes. There was no retinal tear on peripheral retina examination. Neurological examination was normal and cranial computed tomography scan showed no lesions. Blood pressure was controlled with 48 hours of labetalol. Magnesium sulfate was performed in accordance to the Department´s protocol for the management of severe preeclampsia. Ophtalmologic re-evaluation on days 2 and 4 improved significantly, without specific therapy. She was discharged asymptomatic on day 7 with controlled blood pressure. Follow-up examination 2 weeks later showed complete resolution of the retinal detachment (Figures 1C and 1D). Visual acuity remained 8/10 for both eyes.
Figure 1: Retinography: images A) B) at admission, there is a bullous retinal detachment of the posterior pole involving the macula (arrows) and extending superiorly beyond the limits of the superior temporal vascular arcade. The area of retinal detachment is smaller on the left (OS) than on the right eye (OD). Images C) D) at 2 weeks follow up, normal retinography showing complete resolution of the bilateral bullous retinal detachment
COMMENT
Retinal detachment is an unusual cause of visual loss in pregnancy, being observed in 1% of preeclamptic patients and up to 10% of eclamptic patients.1
According to a review of all case reports of retinal detachment associated with preeclampsia/eclampsia published between January 1990 and December 2010, it is usually bilateral (89%), more frequent in nulliparous women (60%), women with a cesarean delivery (76%) and tends to be diagnosed in the postpartum period (69%).1 There is no specific treatment for serous retinal detachment associated with preeclampsia. In these cases the only recommended treatment should target preeclampsia, requiring magnesium sulfate for seizure prophylaxis and anti-hypertensive drugs for severe hypertension. Bed rest and fluid restriction, an ophthalmologic and neurologic examination as well as neuroimaging could be also helpful in the management of preeclampsia with important visual symptoms. Unless there is an associated retinal tear, surgery is never necessary for resolution of serous retinal detachment. Visual disturbances are transient and visual acuity is completely and spontaneously recovered within weeks to months.2
There is no confirmed link between teratogenic effects of fluorescein angiography and breastfeeding. Furthermore, fluorescein angiography is useful as a screening method for diffuse choroidal ischemia. Despite the possibility of identifying a retinal detachment based on the clinical picture and fundus examination, OCT is important for disclosing a macular hole in the differential diagnosis.3,4
During the first 48 hours postpartum, symptoms associated with aggravated preeclampsia usually develop before hospital discharge and are promptly diagnosed and managed. However, in the subsequent days, they are more frequently diagnosed at the emergency room if puerperal women return for medical help. In our Department, in accordance to what is suggested by Barton, et al.5 we insist on giving both verbal and printed instructions on which symptoms should bring immediately the puerperal women to the emergency room. The aim of this measure is to diagnose the earliest an imminent worsening of the preeclampsia.
With this case report, we aim to highlight the importance of prodromal symptoms, mainly headaches and visual disturbances, which may raise our index of suspicion for complicated preeclampsia in the postpartum period.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Ana Fonseca for making the ophthalmologic diagnosis and for providing the images presented and Dr. Ana Aguiar for her contribution to the obstetrical management of the patient.