INTRODUCTION
Bier Spots (BS) are small, irregular, hipopigmented and transient macules. They are usually found on the arms and legs of young adults. These hypopigmented macules can be elicited by placing an affected the arms and legs in the dependent position. When the affected extremities are raised, the macules disappear.1
CASE REPORT
A 33-year-old man was referred to the outpatient clinic with a 4-year history of asymptomatic, white spots on his face. He had numerous, light colored spots over his face in a mottled pattern. Although the spots were asymptomatic, these spots bothered the patient cosmetically. Emotional stress does not aggravates his lesions. Hot weather aggravates his spots. He had no history of vascular disease and family history of such lesions. There were no associations with hyperhidrosis or acrocyanosis and nail or mucosal abnormalities. He has been a smoker for 15 years. He did not consume alcohol. He was diagnosed with alopecia areata six months ago. He was also diagnosed with epilepsy 31 years ago. He underwent epilepsy treatment. When he was two years old, he had started to use carbamazepine. He stopped to use carbamazepine when he was 18 years old. He was diagnosed with deep venous thrombosis in his left leg. He has been using coumadin for six months. He was diagnosed with insomnia three years ago.
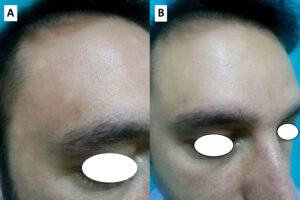
Examination revealed hypopigmented macular lesions with irregular border and a background blanching erythema spread over the face, especially over his forehead. There were no similar skin lesions in any other body areas such as trunk, upper and lower extremities. Lesions appeared when his head was in a dependent position, in 10 seconds (Figure 1A). The lesions had disappeared in 10-15 seconds after he elevated his head (Figure 1B). Clinical examination was normal. Laboratory investigation, including blood count, serum biochemistry, erythrocyte sedimentation rate, rheumatoid factor revealed no abnormality. Electrocardiography and echocardiography were normal. Based on clinical findings, the patient was diagnosed with ‘Bier spot’.
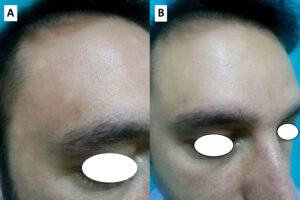
Figure 1: (A) White macules against a background of erythema on a 33-year-old man’s face in the dependent position. (B) The lesions disappeared, after the patients raised his head.
DISCUSSION
BS was first described in 1898. BS is more frequently in women than men.2 The etiology is unknown. BS is thought to be an exaggerated but physiological, vasoconstrictive response induced by venous stasis-associated hypoxia or, conversely, by a failure of the venoarteriolar reflex in dermal ascending arterioles in response to venous filling.3 To date, these white lesions have been given several names, including BS, exaggerated physiologic speckled mottling of the skin, physiologic anemic macules, nevus anemicus, speckled mottling of the limbs, constitutive speckled vascular mottling of the skin, and angiospastic macules.4
On the trunk, lower extremities, and upper extremities, including the palms were generalized, hypopigmented, 1-10 mm macules interspersed with blanching, erythematous macules. The lesions gave a reticulated, mottled appearance. The lesions were associated with dependency of the limbs. The spots almost disappeared completely with elevation of the limbs.1,4 In our case, BS was on his face. To the best of our knowledge, this is the first case report on the face. BS appeared when his head was in a dependent position, in 10 seconds and BS disappeared in 10-15 seconds after he elevated his head.
Some cases have been reported in association with miscellaneous disorders, such as insomnia, alopecia areata, varicosity, palmar hyperhidrosis, tachycardia, deep vein thrombosis during pregnancy, cryoglobulinemia, scleroderma, renal crisis, aortic hypoplasia, lichen planus, and Peutz-Jeghers syndrome.2,4 Our case was diagnosed with insomnia, alopecia areata, epilepsy, and deep venous thrombosis. The present case used carbamazepine for 16 years. It is important to be suspicious of systemic disease in patients with BS, because the spots are occasionally the first sign of such disease, but these spots are more often idiopathic.5
Fan et al reported that the BS in four generalized cases became more visible with emotional stress, but less visible after physical activity.4 BS of the our case does not become more visible with emotional stress, but hot weather aggravates his spots.
Because idiopathic BS is asymptomatic and possibly transient, no treatment is required.6 The present patient did not undergo treatment.
CONCLUSION
This is the first case report that presented BS on the face. While evaluating white macules on patients’ face, BS should be considered in the differential diagnosis.
CONFLICTS OF INTEREST
The authors declare no competing interest.
FUNDING
No financial support was received for this paper.
CONSENT
The patient has provided written permission for publication of the case details.