INTRODUCTION
Bystanders are individuals who witness an emergency situation, have the potential to play a critical role in providing immediate life-saving medical aid as well as vital assistance to those in need. In fact, as bystanders are present at the scene, they bridge the gap between the very first moments of the occurring of the event and the arrival of first responders to the scene, by responding and potentially, by decreasing the likelihood of the victim’s death.
In this time-frame, “the Silent Response Gap”1 and right after the emergency or disaster has struck, whether it be a person experiencing a medical crisis or injury due to an automobile accident, mass shooting, explosion, fire, storm or an earthquake, the presence and active help of bystanders, who might have been injured themselves, is critical.
During these initial moments, the only responders are those who are already present at the scene. Emergency services teams might arrive within minutes, hours or even days. The help provided by bystanders can be lifesaving and include: resuscitation, hemorrhage control, transfer to the nearest hospital or clinic, notifying the emergency services, clearing the disaster scene from other people to prevent them from being adversely affected, search and rescue, psychological support, preventing a suspect escaping the scene and providing vital information regarding the sequence of events. These actions are critical during the first moments immediately after the event has occurred and might have significant impact on the victims, the rescuers, the entire response efforts, situation management and investigation. Active bystanders may represent the “Good Samaritan” who chose to take effective action rather than being passive or ignoring the victim, in spite of various barriers that might otherwise inhibit them from helping. Among these barriers are: lack of knowledge regarding the diagnosis of the case and how to handle it and potential legal liability by causing unintentional harm to the victim.2,3 In several countries including USA, Canada, Hong Kong, Australia and Israel “Good Samaritan Law” has been enacted in order to encourage bystanders to provide medical assistance without being potentially sued in case of unintentionally doing harm or damage.1 A recent study on first-aid learners in Hong Kong has revealed that the Good Samaritan Law is widely acknowledged, however, cardio-pulmonary resuscitation (CPR) would be delayed or even not been provided due to fear of liable consequences.4 Furthermore, Vaillancourt et al5 mentioned that although medical assistance can and should be learned, such as CPR and bleeding control, it is the helpers’ behaviors that should be changed – including eliminating the fear of being sued or being contracted by a disease while taking care of the victim.
Given the understanding of the important role of bystanders in responding to emergency scenes, the main question is how bystanders helping actions can be encouraged and made most effective? Research has shown that bystanders are willing to intervene and provide help,6 but are limited by various settings and demands7 or the risk to themselves.8 Bloch et al9 analyzed surveillance camera recording of violence in public place and found other forms of bystanders intervention on the active-passive continuum of bystander intervention (hesitant, shifting, and ambivalent behaviors). However, despite various campaigns to raise awareness of the importance of bystanders help, and basic medical training for the general population,10,11 especially in the USA and Canada, active bystanders assistance could be improved in terms of increasing the number of helpers and effectiveness of their aid.
Given this, it is crucial to study the function of bystanders as time-zero responders before the arrival of professional first responders) in terms of the effectiveness of their actions, and provide insights on how to assimilate their assistance into the configuration of emergency medical efforts and disaster management. This will be done by presenting a new framework, which categorizes bystanders help according to two basic factors: presence at the scene and the degree of social organization established on-site.
WHY DO PEOPLE HELP OTHERS IN NEED?
In 1964 Kitty Genovese was brutally murdered in New York. The murder investigation has revealed that 38 people witnessed Genovese’s attack and murder, but no one reached out to help her. This has evoked a wide public debate on the moral, social, psychological and legal aspects of providing assistance to strangers in need. Social psychologists, Latane et al12 have termed the “bystander effect” to describe the tendency to avoid providing help to those in need when there are others present, who also witness the critical event. According to the “bystander effect,” the presence of others leads to “diffusion of responsibility”, which means that each of the individuals present does not take action as he or she believes that someone else will provide the help. Consequently, no one helps. Furthermore, due to “pluralistic ignorance”, when comparing ourselves to others, we assume that someone else will “know better”.
1. In the USA, there is no such federal law, but rather, each state has enacted the law separately.
what to do, also leading to refraining from providing help to those in need. Lastly, due to evaluation apprehension, people tend to be afraid of being judged as acting inappropriately during uncertainties, and as a result, avoid taking action.12,13,14
Latane et al12 research has led to several research avenues, mostly focusing on ways to explain how to reduce the bystander’s effect and increase helping behavior. Evolutionary biology uses altruism as the trait behind the willingness to help others. Altruism involves feeling strong empathy with someone in need and the willingness to reduce his or her suffering. Altruism has an evolutional explanation, as one would even risk harm or death to himself in order to enhance the chances of survival of his relatives or other human beings around him. Furthermore, recent explanations highlight the willingness to reduce negative feelings if no help is provided. In other words, it seems that helping behavior is also related to some personal benefit, in terms of emotional regulation. Also, empathy and distress were found to be related to helping behavior. While feeling distressed prevents the individual from providing help, empathy increases the chances of helping without external reward.15 A recent study by Hortensius et al16 using virtual reality simulation and neuroimaging has revealed that stress is the immediate response characterizing potential bystanders, which leads to a ‘freeze’ or behavioral (‘basement’) inhibition.17,18,19 However, emotional, motivational, and dispositional factors, such as emotion regulation and perspective taking, affect levels of empathy, which lead, in turn, to helping behavior.
Recently, another important dimension was found to influence the occurrence of “bystander effect”, i.e. lower levels of providing help. This is the degree to which the situation is perceived as dangerous, to both the victim and the helper. It was found in experimental and case studies that when the situation is perceived as dangerous, acts of moral heroism tend to appear, and bystanders are more likely to step up, put themselves at risk, and provide the needed assistance.19,20,21,22 Furthermore, Fischer et al20 suggest that in dangerous situations, participating bystanders can have a positive effect on another person who might be willing to act. This leads to an opposite function of the presence of others in an emergency situation – instead of leading to a passive reaction within the present crowd, bystanders presence can lead to support the action of at least one individual who engages in saving behavior.
IMMEDIATE RESPONDERS’ MEDICAL ASSISTANCE
Bystanders medical intervention might be critical in situations where the time until the arrival of environmental management systems (EMS) decreases chances of survival. Such situations include but are not limited to: out-of-hospital cardiac arrest (OHCA), severe bleeding and airway occlusion among other trauma cases and mass casualty incidents. For these cases public campaigns and training courses provided for the general public are intended to increase efficacy, awareness and cooperation among citizens when witnessing a person in need. For example: “stop the bleed” (stopthebleed.org/),25 “you are the help until help arrives” (community. fema.gov/until-help-arrives),26 and “hands-only CPR” (cpr.heart. org/en/cpr-courses-and-kits/hands-only-cpr).27 Results from studies in various countries reveal an increase in survival rates and bystanders intervention in some settings (national clinical registry, pre-post training measurements etc.),1,10,28,29 but not others (randomized clinical trial).30,31
Medical Aid
Out-of-hospital cardiac arrest (OHCA), where chances of survival are less than 10%,32-34 has been widely examined for the effectiveness of bystanders interventions.35,36,37 Overall, Bystander CPR rates found in Japan are 40.2%, 41% in Korea, and only 10.5% in the United Arab Emirates.38 In Sweden CPR before EMS arrival was performed in 51%39 and 45% in Norway. Hasselqvist et al39 report that CPR can double that chances of survival if performed quickly before the arrival of the EMS. Also, a recent meta analysis of the use of bystander automated external defibrillator (AED) found positive association between AED and survival to hospital discharge and better neurological outcomes.40 Furthermore, a study examining data from, a non-metropolis area in North Carolina has also found that CPR and AED performed by bystanders increases chances of survival.41 These results highlight the importance of bystanders intervention especially in sparsely populated areas, where medical infrastructure is limited and the immediate medical assistance is critical.
Another life-threatening emergency situation is hemorrhage which is considered a critical cause of potentially preventable cases of death due to an injury, especially among young people.42 Campaigns and courses are dedicated for population training regarding “how to stop the bleed” with success in knowledge of how to use tourniquets31,43 and self-efficacy to use it.44
Mass Casualty Incidents
Mass casualty events are characterized as being sudden, unexpected and large scale involving multiple casualties with various degrees of injuries, physical damage across a wide area, and potential for continuous and cascading risks and damage (for example, falling debris, fires, chemical spill and secondary explosions). In such events, the number and medical severity of victims exceeds the capacity of emergency services to provide assistance and care, and therefore bystanders can play a vital role as force multipliers in various positions. These include: preliminary medical aid, search and rescue, scene management (traffic control, on-site security), transportation or evacuation to hospitals and helping the victims by contacting relatives, collect belongings of the victims, language translation, and other supports.45
Bystanders help was documented in many disaster events around the world, including earthquakes, hurricanes, terror attacks and gas explosions.18,19,45,46,47,48 Findings show that people tend to converge in the scene in the immediate aftermath of the disaster or mass casualty incident,49,50 and assist the victims in any way available.51,52 Furthermore, another important aspect of the help provided is reflected in the social organization which evolves during the helping process. Ashkenazi18 reported on new social stratification of “victims” and “rescuers” which had developed in the aftermath of Haiti earthquake (2010). Also, norms of mutual help characterize the affected community. People provide and share important resources from food, water and shelter to workplaces and transportation.7,18 In fact, in contrast to the “bystander effect”, when bystanders connected with one another, even by eye witness reporting social cohesion emerged and help was increased.53 Drury54 and Drury et al55 suggested that a shared identity emerged to enhance collaboration among those who experienced the London bombings in 2005.
In addition, acts of leadership, taken by bystanders who step up, are also evident. Bystanders who provide leadership by directing activity and creating meaning47 during times of chaos serve as an important resource in the entire scene management. Moreover, these findings suggest that bystander leadership allows for self-organization of these bystanders as a group in order to provide assistance. As a consequence, more effective bystander management would lead to more effective utilization of those people as an important resource.
NEW FRAMEWORK FOR ACTIVE BYSTANDERS HELP DURING EMERGENCIES
Research and case studies on bystanders active participation in emergency scenes has mainly focused on explanations for active helping and rates of helping in particular events such as medical emergencies, violence, harassment and bullying. Furthermore, much attention is given to exploring ways to improve training and education for the general population in order to increase helping behavior, especially life-saving practices. However, the effectiveness of the active bystanders behavior is less apparent, mainly due to objective measurement limitations. Nevertheless, given the wide scale of potential bystanders interventions and the emerging need to increase the public’s awareness of and capabilities for helping those in need, it is important to understand how to improve the effectiveness of bystanders management efforts. We therefore suggest a new framework for understanding bystanders intervention based on two main factors:
Presence of Potential Savers at the Scene Over Time
Right after the event has occurred, at T1 (the Silent Response Gap), bystanders are the only potential helpers on-site. Later, upon the arrival of official first responders, at T2, the resources to manage the scene increase dramatically. However, dependent on the size of the event and multiple contributing factors, the arrival of first responders to the scene might be delayed and the length of the silent gap will be extended accordingly. Until the arrival of first responders, in this critical period of time (the Silent Response Gap), effective bystanders intervention is critical for both managing the scene and providing life-saving aid. The moment first responders arrive, the ‘formal’ responding phase begins, and bystanders may play a new role as helpers under the command of the official first responders.
Social Organization
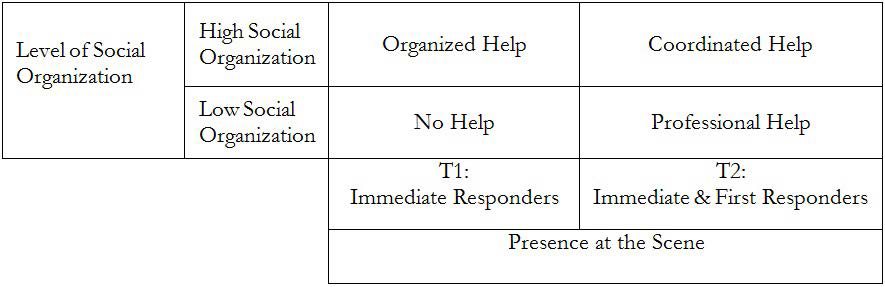
The presence of bystanders, and later on, first responders, activates a social process between the two groups: within the bystanders themselves (while the emergence of a bystander-leader accelerates this process) and between bystanders and first responders. The first social organization (among the bystanders) lead to “organized help”, while the second (between bystanders and first responders) lead to “coordinated help” (Figure 1). The social process is practically based on a shared identity among the crowd,56 which may stimulate collective behavior. This process can start immediately with the emergence of a bystander-leader, or by help given by individuals who are capable of acting during these moments. Those who are prone to act might call other bystanders to help, by showing support of active helpers calling emergency line or readiness to follow other instructions.
Figure 1. Frameworks for Evolving Help Effectiveness: Types of Help Provided by Bystanders Over Time and as Function of the Evolving Social Organization
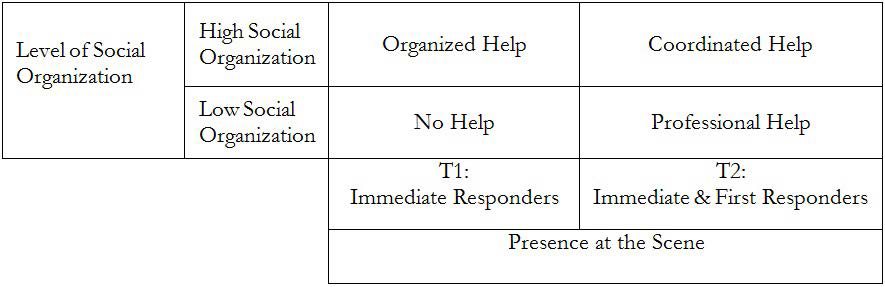
The person who emerges as a bystander-leader, might be a person who is competent or experienced, in terms of education (medical doctor, nurse, paramedic), or training (a police officer, firefighter, an individual who has first aid training). It might also be the first person to recuperate from the “basement behavior”,17 by assessing the situation and initiating appropriate action. We suggest that the social organization which develops over time on-site reinforces the help provided by bystanders, and subsequently, by first responders. The focus is on this social process – communication, shared values, grouping of strangers, and activation of emerging norms – which lead to collective behavior. The emergence of a leader should accelerate the response and the positive consequences. At first (T1), bystanders react or do not react as an outcome of the evolving social relationship among themselves. Later (T2), upon the arrival of professional first responders, the social organization allows for a hierarchical response led by the first responders. Optimal response would include connectivity and coordination between first responders and bystanders, so that aid is provided with multiple forces in terms of their quality, quantity and speed.
Putting these two main factors on a matrix reveals an evolution of bystanders help over time as a function of the changing social organization on-site (Figure 1):
The framework reveals four types of help options:
1. Before the arrival of first responders (T1): a. No help: The worst response; Bystanders are mostly passive; first responders are still away b. Organized help: Ordered response by only bystanders (immediate responders) [This presumes bystander leadership has emerged] 2. After the arrival of first responders (T2): a. Professional help: The most common current response. First responders are active, while bystanders are told to leave the scene. b. Coordinated help: The desired response. First responders and bystanders are responding together with full social engagement and collaboration within one official command structure.
This framework highlights the spectrum ranging from “no help” – where no bystander becomes active, to “coordinated help”, which maximizes the capabilities of all involved bystanders as well as the professional first responders and other available resources. In terms of life-saving, shifting from no help to coordinated help is linear over time parallel with the evolving social organization. However, it also has an exponential effect, as immediate organized help would likely decrease the extent of severe disability and mortality. For example, given ten injured people after a bombing, if no one helps – all ten might die. If effective bystander assistance is provided, two or three of them might be saved. But if coordinated help is provided in a timely manner, all casualties might be prevented.
Therefore, the effective response combines the presence of optimal (not maximal) amount of emergency forces which are socially organized to include the active bystanders. Two main elements increase the effectiveness of bystanders response: (a) if bystanders react immediately and together as an organized group (organized help); and (b) if upon the arrival of first responders, the helping process that has already begun, will be maximized while first responders leverage the presence and actions of bystanders as helpers, instead of disregarding and pushing them out of the scene (coordinated help). The coordination between professional first responders and active bystanders is the desired outcome as this would likely improve the professional approach to the victims, shorten the time for triage and transportation to the hospitals, save lives, decrease suffering and severe diability and elevate community resilience.
Using this framework allows for a better understanding of what first responders could expect from bystanders when arriving at emergency or disaster scene. As bystanders can become an asset, not an obstacle, coordinated help between professional first responders and bystanders will enable immediate and more accurate care for the victims. Furthermore, this framework will also serve as a basis for more adequate and effective training courses, awareness and education campaigns, and most importantly, an improved bystanders management.
CONCLUSION
Active bystanders are an integral part of the emergency scene. During the silent response gap, from the moment the emergency has occurred until the arrival of first responders, only bystanders are there to help, and research has shown that their actions are effective in saving lives. However, in reality, professional emergency forces tend to disregard bystanders and send them away from the scene. We highlight the importance of leveraging the social process which develops among bystanders and between bystanders and first responders in order to better cooperate, decrease mortality and increase the volume, quality and speed of help.
Bystanders motivation to help and get involved in the emergency operations is high, and is mainly based on social and psychosocial factors such as norms and shared identity.14 The range of roles and actions, which bystanders potentially could take, are wide and include medical aid, psychosocial assistance, search and rescue and intervention during acts of violence or harassment. Moreover, by converging at the emergency scene, bystanders self-organize and develop emergent social order including deconstruction of social stratification, share of goods, and new life-routine.18 Given that bystanders are present in the emergency area, it is important to increase the effectiveness of their helping actions. The effective and timely response is dependent on the social organization of bystanders. The emergence of a bystander-leader, who will, first, step up and approach the victim(s), organize and assign responsibilities to other bystanders can generate such an organized help quickly. This social organization will be effective during both dangerous and non-dangerous situations,6,20 as well as isolated events such as a person who has collapsed in the street or a car crash) or mass casualty events.
The presented framework (Figure 1) suggests that specific helping types can be expected at a mass casualty incident area of an emergency as a function of the social organization among bystanders and between bystanders and first responders. Over time, social mechanisms develop during emergencies especially in complex situations, where the resources of first responders are overwhelmed. In such cases, the coordinated response of bystanders with first responders would lead to more reliable and effective results. Policy makers in the area of emergency response should focus on understanding by standers behavior during emergencies. This will lead, first of all, to saving lives, as well as increased social resilience and enhanced trust between emergency authorities and citizens. Further, it will lead to better preparedness at both the structural-organizational level (in terms of how to utilize the capacities of bystanders and manage them) as well as at the level of public awareness and individual preparedness (in terms of public campaigns raising awareness and training courses for specific skills).
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.