INTRODUCTION
One of the most preventable errors that could occur during spinal surgery is operating on the wrong site. Surgery done on the wrong site includes either operating at an unplanned side or level. In spinal surgery, the most common error for wrong site surgery is a procedure done one level above the intended level.1
Wrong-level spinal surgery is considered a ‘never-event’ and is under-reported.2 The rate of wrong level spine surgery ranges widely in the literature. It is estimated that at least 50% of spine surgeons will perform at least one wrong level procedure in their career.3,4 A national survey done on incorrect site surgery among neurosurgeons in Canada-based on anonymous questions self-assessment-concluded that corrected wrong level lumbar discectomies rate was estimated to be 12.8 per 10,000 operations, which was much higher than cervical discectomies at 7.6 per 10,000 operations. Risk factors for such occurrences were recognized to be fatigue, increased time pressure and urgent operations.5
A wrong level surgery can potentially have significant emotional, physical, financial and legal consequences on the patient as well as surgeons and the importance of preventing this event cannot be overemphasized.1
Careful pre-operative assessment along with robust pre- and intra-operative localization techniques is crucial in improving the quality of the surgery. Historically, the surgeons use palpation or “counting” from a fixed reference point such as L5-S1 vertebrae for determining the level of operation in lumbar spine surgery.6 More recently, X-rays and fluoroscopy are increasingly and almost universally used. However, use of X-rays once and only at the beginning of the procedure is not thought to be enough and there are standard operating procedures (SOPs) occasionally suggested to define the use of X-rays during these procedures,5 which are sometimes modified by organizations for local use. It remains the collective responsibility of the organization; however, to ensure that such SOPs are strictly followed to avoid errors during the surgery. We could not find any such audit in the literature regarding compliance with similar SOPs elsewhere. We performed a prospective audit in our department to assess if the SOP was being followed.
METHODS AND TECHNIQUE
This is a prospective audit of a total of 409 patients undergoing a lumbar discectomy or decompression within a single neurosurgical department. Caldicott approval has been taken for this audit.
The SOP followed in our department has been described below:
• After general anesthesia, patients lies in prone position
• Check list and consent confirmed out loud with theater team
• Skin palpation of spinous process for counting level
• 18 G needle inserted vertically through skin at a disc space level
• Lateral X-rays obtained using Siemens Ziehm vision (Small field of view of 0.8 m²).
1. Step 1 X-ray: Pre-operative X-ray to identify the targeted level, which should be confirmed by 2 clinicians (compulsory). It is considered adequate if the needle-points towards disc space;
2. Step 2 X-ray: Intra-operative X-ray after skin incision but before decompression in case of doubt of the trajectory (optional);
3. Step 3 X-ray: Intra-operative X-ray at the end of the procedure and prior to closure, either marking the inside of the disc space or the superior and inferior edges of the decompression (compulsory).
The number of X-ray exposures should be recorded for each step. This SOP has been adopted from Tayside National Health Service (NHS) healthcare and the broad information available from NHS choice UK5 as there are no general universal SOP descried in literature particularly in the US or the Royal Colleges. We have modified the local SOP by adding an intra-operative X-ray.
In view of the clinical importance of following the SOP during surgery, in one of the morbidity and mortality meetings in Department of Neurosurgery in 2015, it was decided to perform a prospective audit in the department to check compliance to the SOP. It was meant to be a clinical audit rather than a research project and in accordance with local practice, the decision of the department was felt to be adequate in carrying out the audit project.
The first cycle of this audit included 202 patients from June to November 2015 (6 months).
The second cycle (re-audit) included 207 patients from December 2015 to May 2016, to see the significance of the change implemented. The data was collected from theatre logbook, medical notes and PACS. Number of times intra-operative X-rays detected an incorrect level at each stage of the procedure was identified. Categorical factors (level of pathology and correct/incorrect level in interpretative level check) were tested with Chi-squared test. Continuous factors (number of pre-operative X-rays required) were tested using the Mann-Whitney U-test. p value were calculated for both with p<0.05 as significant.
RESULTS
In the First Cycle
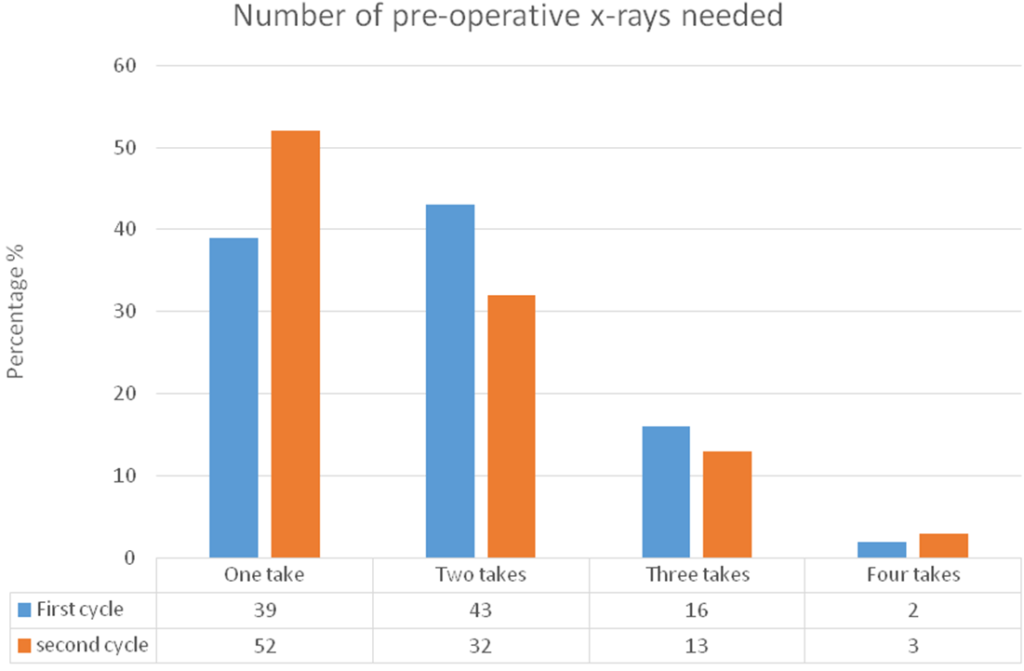
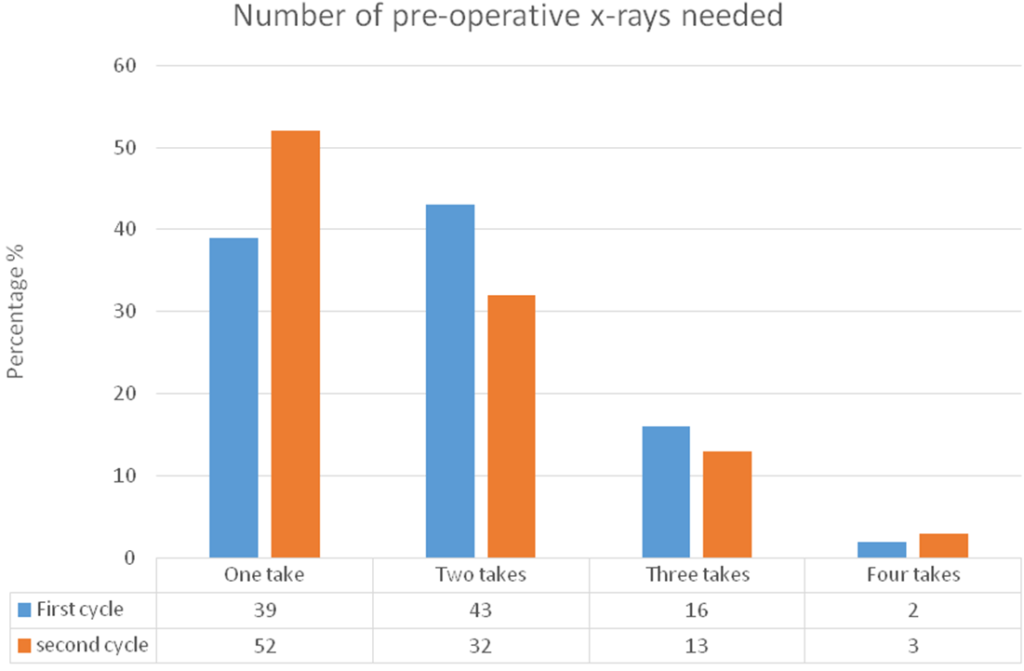
There were 202 patients included (114 had a discectomy and 88 had decompression). One patient did not have pre-operative X-ray step 1 level check; however, the number of step 1 X-ray exposures was recorded in only 143 cases. The number of pre-operative step 1 X-rays required for those patients were as follows: 39% required one exposure, 43% required two exposures, 16% required three exposures and 2% required four exposures (Figure 1). Palpation was found to be accurate in 39% patients.
Figure 1: Comparative Graph of the Number of Pre-operative X-ray (Step 1) Needed in both Cycles.
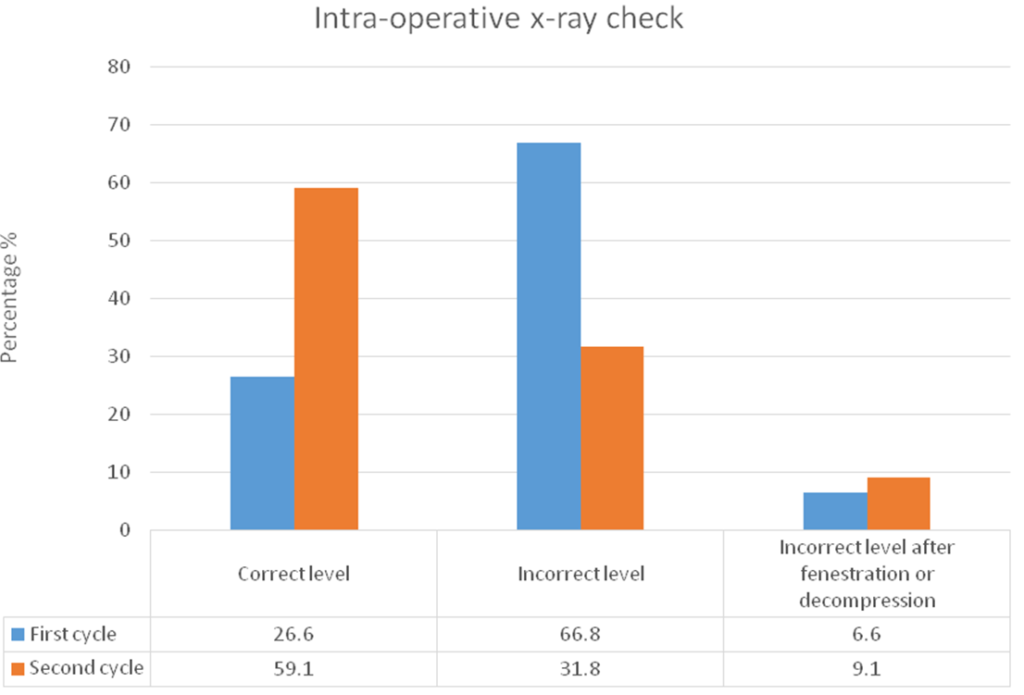
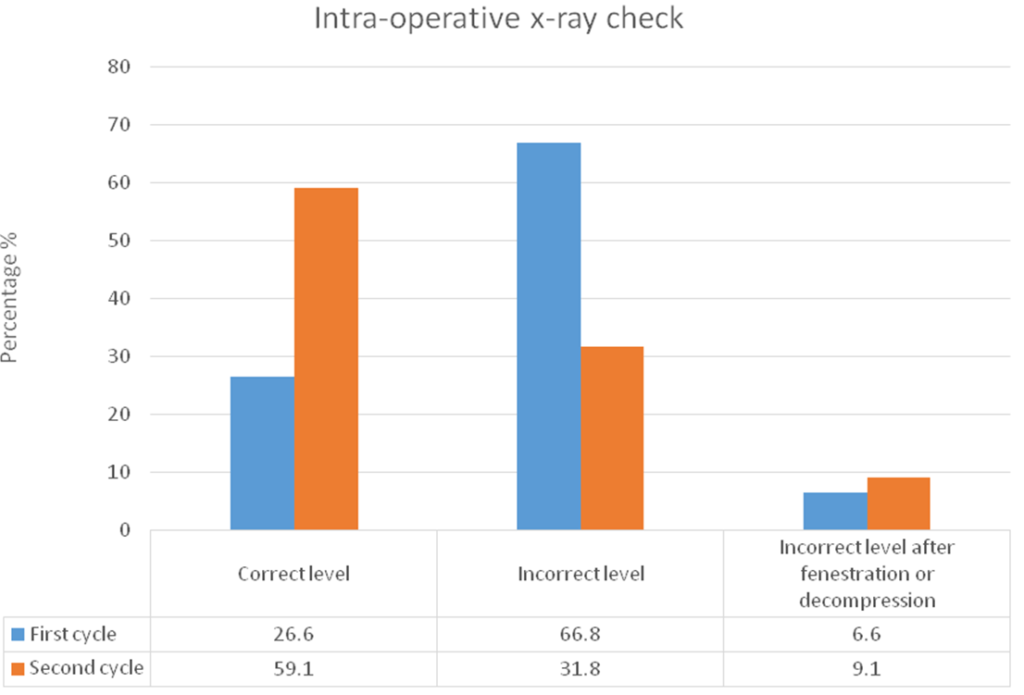
Intra-operatively step 2 X-ray (optional) was performed in 28 cases (13.9%); 8 cases (26.6%) confirming the correct level; however, in 18 cases (66.8%) the X-ray detected a wrong level before the decompression, nonetheless in 2 cases (6.6%) the step 2 X-ray was obtained after the fenestration or decompression (Figure 2). Every patient had X-ray step 3 level check before closure.
Figure 2: Percentage of Correct and Incorrect Levels During Intra-operative X-ray Check (Step 2) when in Doubt in both Cycles.
In the Second Cycle (Re-Audit)
There were 207 patients included (127 had a discectomy and 80 had decompression). All patients in the second cycle had a pre-operative X-ray step 1 check. The number of pre-operative X-rays required for those patients were as follows: 52% required one exposure, 32% required two exposures, 13% required three exposures and 3% required four exposures (Figure 1). Palpation was found to be accurate in 52% patients.
Intra-operatively step 2 X-ray was performed in 22 cases (10.6%); 13 cases (59.1%) confirmed the correct level, 7 cases (31.8%) were on the incorrect level before decompression and 2 of the cases (9.1%) had incorrect level after fenestration and decompression (Figure 2). Every patient had X-ray step 3 level check before closure.
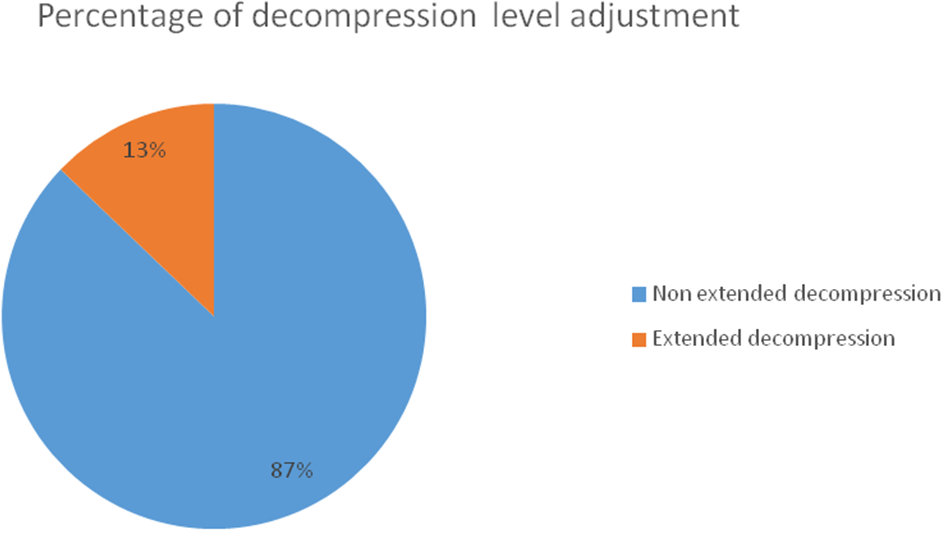
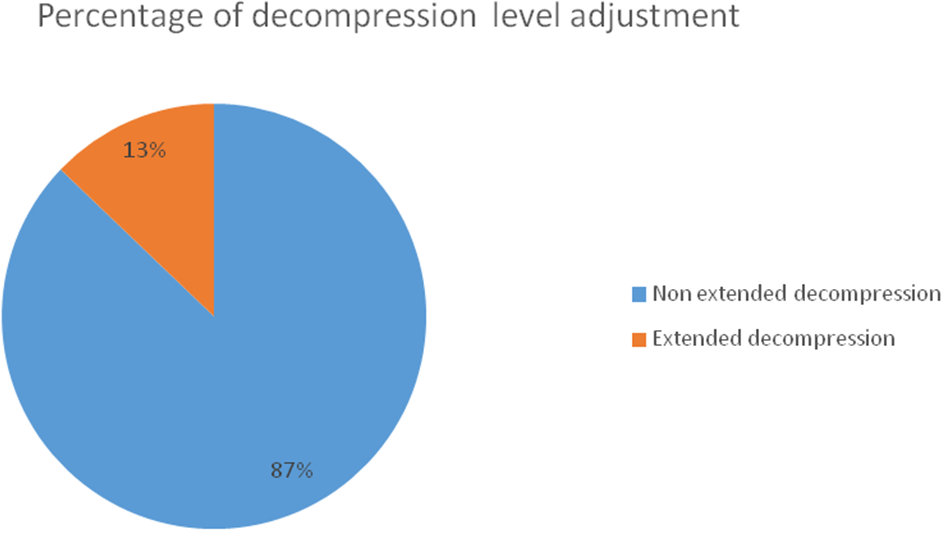
We also decided to look at the number of patients who required further decompression during their surgery in the re-audit. We obtained a step 3 X-ray level check of the superior and inferior edges of lumber decompression and checked for adequate decompression. We found that 8 patients out of 80 required further decompression superior or inferior as it was deemed inadequate by the surgeon. 2 cases were single level, 2 cases were 2 levels and 4 cases involved three or more levels of decompression (Figure 3).
Figure 3: Percentage of Patients having Extended Decompression in Second Cycle (Re-Audit).
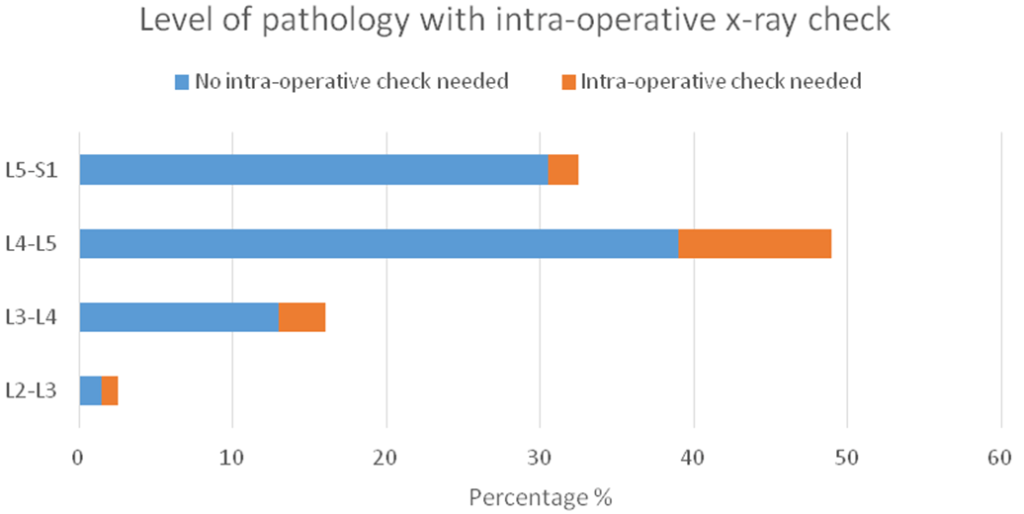
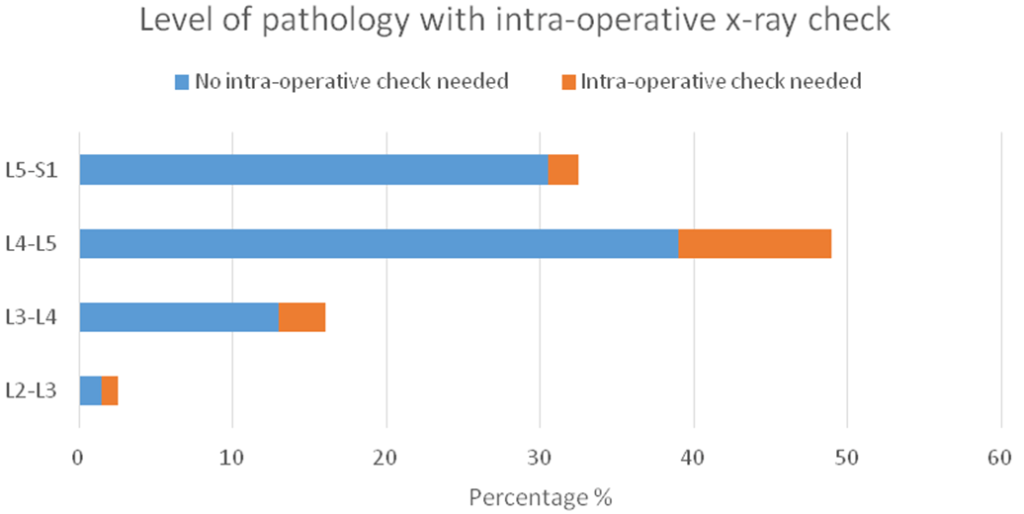
The most common level of pathology identified in the second cycle was L4-L5 followed by L5-S1. There was a statistically significant correlation (p=0.0435, Chi square test) between the level of pathology and the use of intra-operative X-ray check in cases of doubt (Figure 4). However, there was no significant correlation between the pathology level and localization errors (p>0.05).
Figure 4: Level of Pathology and the Percentage of Intra-operative X-ray Check (Step 2) Needed in Cases of Arising Doubt in Each Intervertebral Level (p<0.05).
There was no difference in surgical time before and after this audit (first and second cycles).
Notably, transitional vertebra did not have any implication of the wrong level marking or the surgical counting because it was well agreed prior to surgery between the 2 clinicians on what to call each level and how to determine the right level on X-ray (Figures 5, 6, 7 and 8).
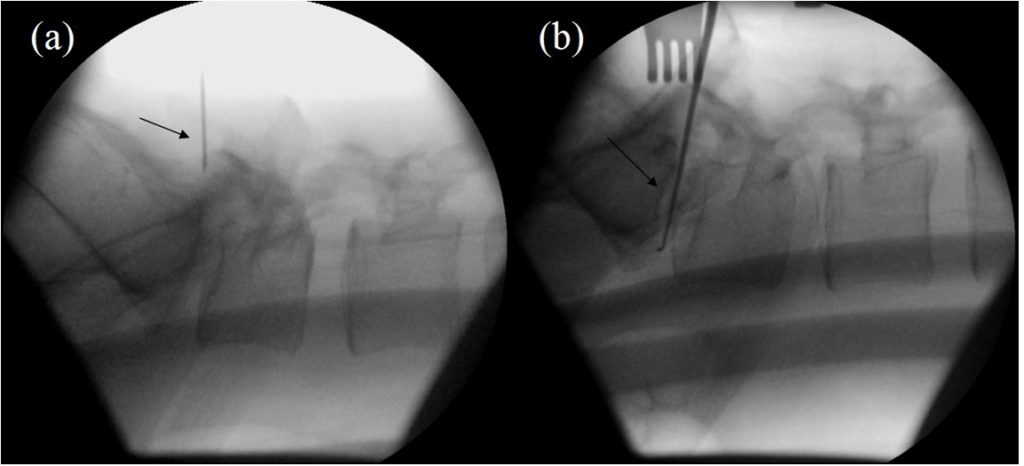
Figure 5: Pre-operative (Step 1) X-ray (a) Shows Needle (Arrow) Projecting towards L5/S1 disc. Intra-operative X-ray (Step 3) in (b) Showing Hook (arrow) within L5/S1 Disc Space.
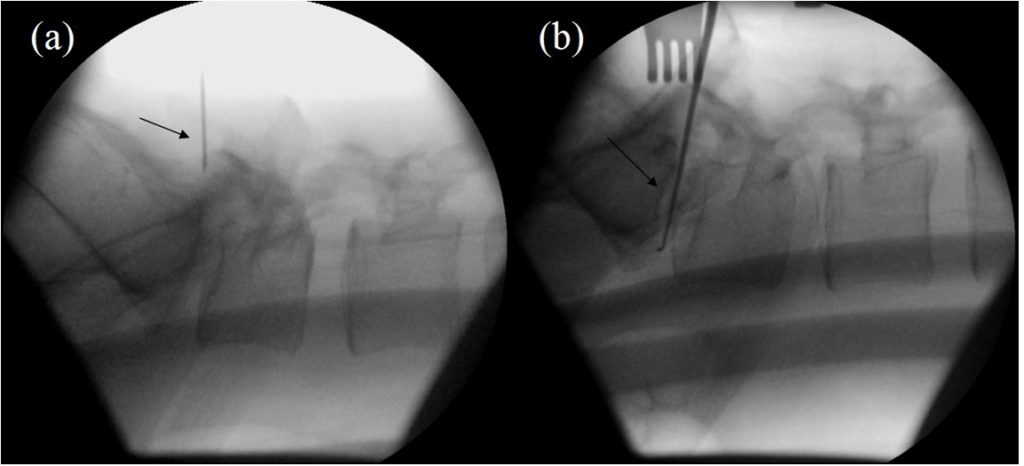
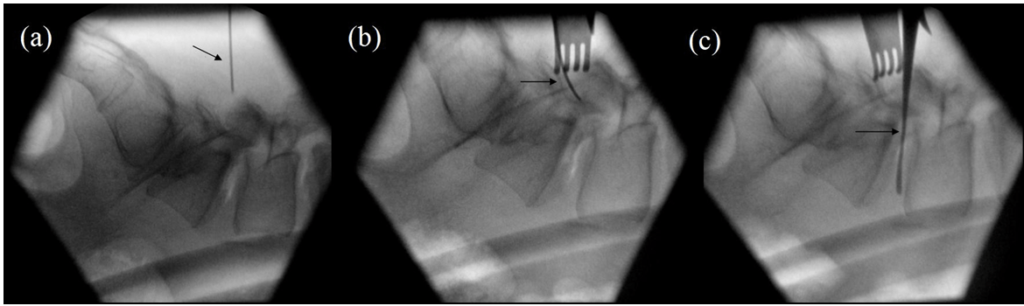
Figure 6: Pre-operative (Step 1) X-ray (a) Shows Needle (Arrow) Projecting Towards L4/5 disc.
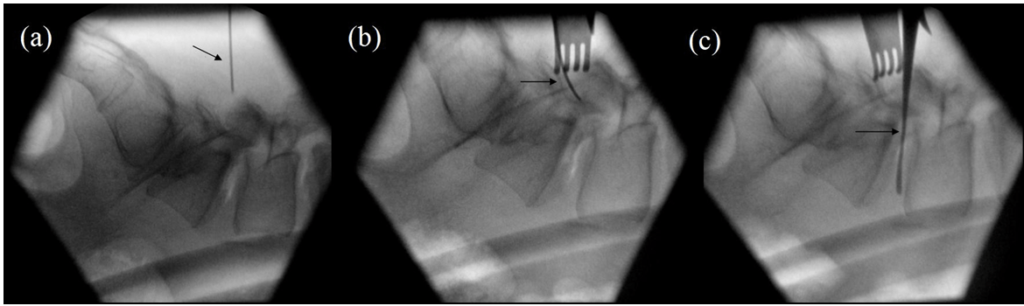
Intra-operative (Step 2) X-ray (b) Shows Needle (arrow) below L4/5 disc. Intra-operative X-ray (Step 3) (c) Shows the Hook (arrow) within L4/5 disc.
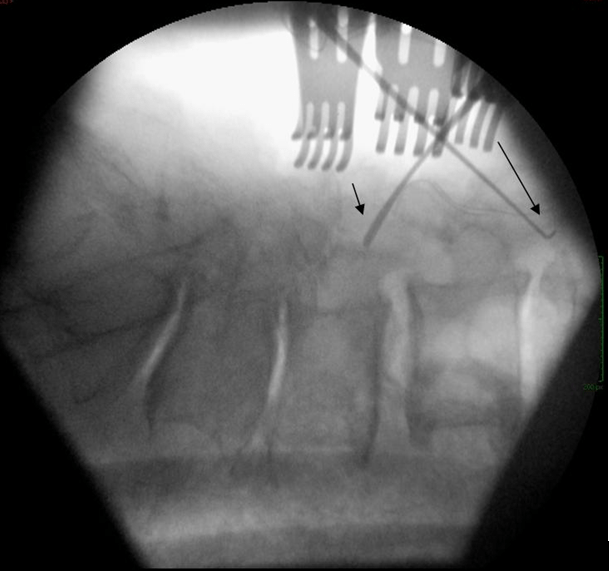
Figure 7: Intra-operative (Step 3) X-ray Shows Hooks (Arrows) at the Superior and Inferior Margins of Decompression.
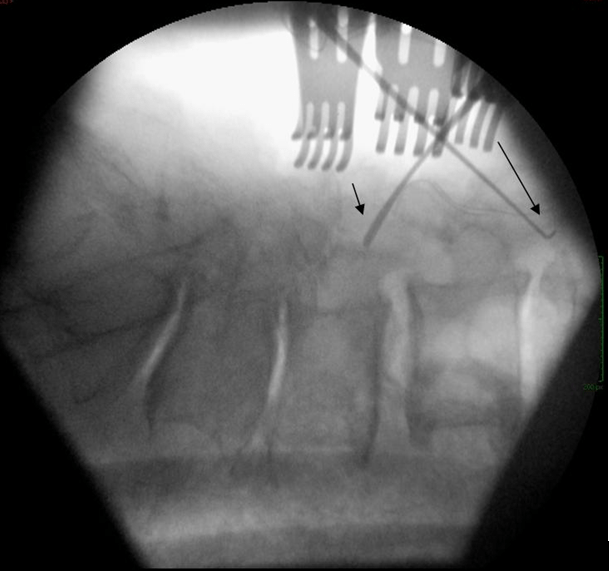
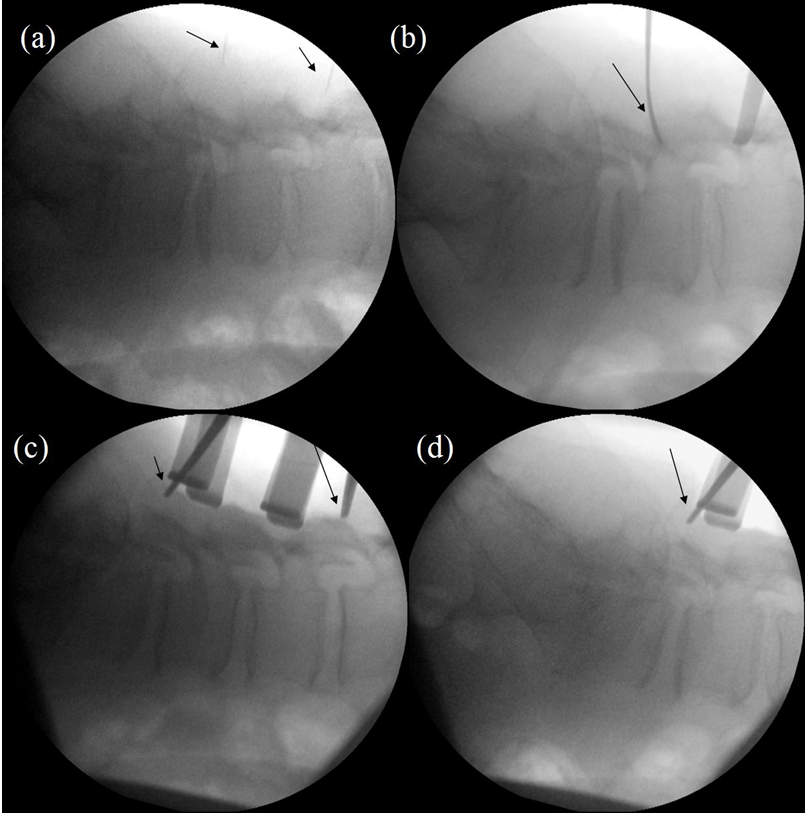
Figure 8: Preoperative (Step 1) X-ray (a) Shows Needles (Arrows) at Superior and Inferior Margins of Planned Multilevel Decompression.
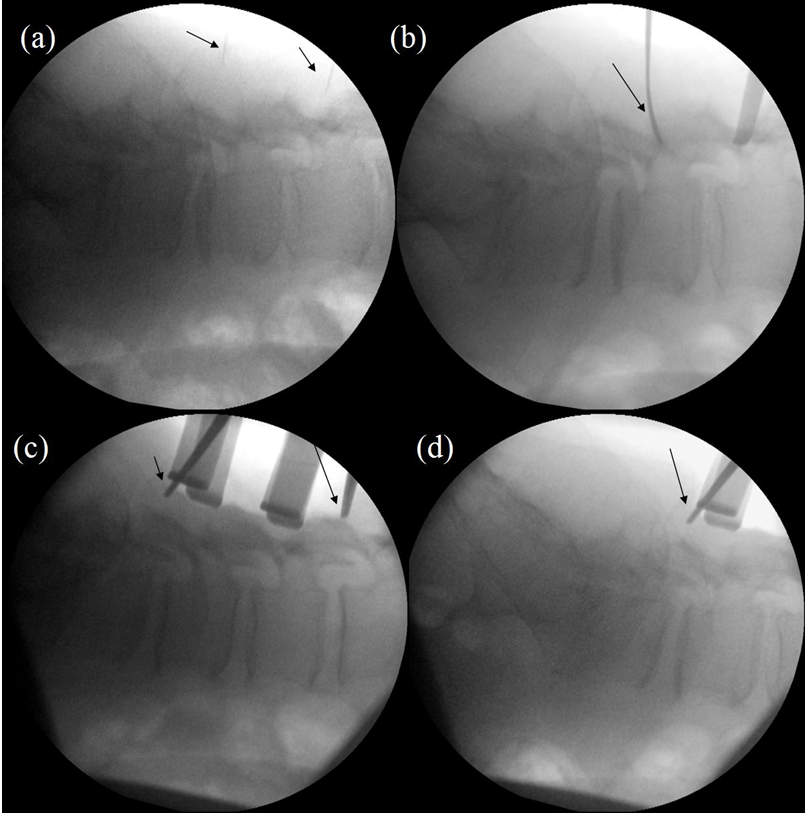
Intra-operative (Step 2) X-ray (b), Confirms the Level by the Needle (Arrow). Intra-operative (Step 3) X-ray (c) Shows Hooks (Arrows) at the Superior and Inferior Margins of Decompression, However, the L5/S1 Junction is Not Included. Intra-operative (Step 3) X-ray (d) Shows Hook (Arrow) at the Inferior Margins of Decompression, the L5/S1 Junction is Now Included, thereby Confirming the Exact Level of Decompression.
DISCUSSION
Spinal surgery is a complex procedure, which involves a coordinated team work and significant planning. Appropriate communication is crucial element to ensure the best outcome and to avoid any unnecessary complication or errors such as wrong level surgery because of the significant implications for the patient, the surgical team and the institution.
Even though wrong level spinal surgery is a “never event” however it is still one of the potential complications and suspected to be under reported.1 A national survey conducted by Mayer et al identified that 55% of surgeons disclosed that they started operating on a wrong spinal level, which was corrected intra-operatively.7
To ascertain the correct level of surgery, traditionally, the most common anatomical landmark for palpation has been counting the facet joint and spinous process followed by lamina and interspinous ligaments.2 There are several potential reasons why it may be difficult to consistently and accurately establish correct level by palpation. One in five patients do not have the normal fifth lumbar-type vertebra. Patients with unusual spine anatomy or deformity such as scoliosis or hyperlordotic make it difficult to count the correct level. Use of intra-operative imaging on morbidly obese patients is also challenging and has a higher risk of errors.8 It was notable that the palpation alone was found to be accurate only in 39% and 52% patients in cycles 1 and 2 respectively.
The use of X-rays to localize the level has emerged and established as a very important method to prevent the risk of wrong level surgery.1 However, there is no consensus about optimum use of X-rays during the surgery. The use of X-rays during surgery can vary from pre-operative X-rays to various combinations of intra-operative X-rays or fluoroscopy. Both Spot X-rays and fluoroscopy have been used by spinal surgeons without clear preference. A national survey of members of the North American Spine Society (NASS) showed a 56% reported using plain radiographs and 44% used fluoroscopy as the localization method.9 Some of the survey results would suggest that a substantial number of surgeons use both techniques in combination.7
Use of pre-operative X-rays alone, although thought to be widely in use, may be inadequate. Performing lumbar microsurgery involves a very small incision. In fact, one level lumbar spine incision in a microdiscectomy or microdecompression is approximately 2.5-4 cm. This gives a very small window to identify the appropriate operating level.6 In our local SOPs, therefore, we include additional (Step 2 and Step 3 X-ray exposures) to confirm that a correct and adequate level is being operated upon.
The aim of this audit was to review our compliance with our SOPs using multi step X-rays to identify lumbar spinal level, determine the accuracy of lumbar spine level marking by palpation, the intra-operative error rate following pre-operative X-ray level marking and to determine the adequacy of decompression during lumbar spine surgery. No Step 1 pre-operative X-rays were obtained for 1 patient in cycle 1, although 100% compliance was noted in cycle 2. The recording of number of X-ray exposures also clearly improved to 100% during cycle 2. We identified that using anatomical landmarks as a localization method was often difficult with 1 exposure alone and as a result we had to take more than single exposure (step 1) in at least 48% of our patients. We also found that using additional X-rays (step 2 and step 3) gave us the opportunity to correct the surgical level during surgery and prevented wrong level surgery in 27 cases. In 8 cases we found that the operating surgeon deemed the decompression level was insufficient after (step 3) X-ray of the superior and inferior margin and further extension of surgery was required. Most of the cases needed superior margin extension of decompression. The risk was also higher in multilevel decompression rather than single level. Eventually, at the end of procedure, all our patients had adequate surgery performed in both cycles.
It was also noticed that the most common level of pathology was L4-L5 level, which was also associated with a significantly higher incidence (p<0.05) of intra-operative doubt resulting in use of additional X-rays exposures to identify any localization errors.
The current audit clearly shows palpation and even preoperative X-rays as being inadequate in ensuring correct level surgery or adequate decompression. It establishes the superiority of our SOP by using X-rays during surgery at different stages rather than merely at the beginning of the procedure. We are not aware if this practice is widespread or limited as no published data is available regarding the same; our audit is the first known audit of its kind. Also, as we noticed, it is also important to continue to audit practice so ensure that the SOP is also followed in real practice including all steps, as bypassing some of the steps can potentially result in wrong level surgery with its associated complications.
CONCLUSION
We have developed an SOP in our department that essentially involves multi-step X-rays during lumbar spinal surgery to accurately identify and then reconfirm correct level during the procedure that allows necessary corrections at appropriate time. We have also highlighted that use of pre-operative X-ray alone is inadequate. We have also audited our practice to ensure that the SOP is followed appropriately in our institution. Our results show that it is possible to avoid both, a wrong level spinal surgery for discectomy and ensuring adequate surgery for decompression (including multilevel), by developing and adopting such SOP.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.