INTRODUCTION
Social scientists, specifically anthropologists, have a specific role in public health emergencies, particularly during unprecedented and sudden health crisis outbreaks of infectious diseases like the current coronavirus disease-2019 (COVID-19) pandemic.1,2,3 At the early stage of a pandemic or epidemic attack, due to the infectious nature of the diseases and the lack of effective treatment or vaccines, nations or states have to implement basic public health regulations like lockdown, travel restrictions, workplace closures and closer of academic institutions. These actions significantly impacted the life and livelihood of the people. Therefore, the acceptance and response of such restrictions may depend not only on the individual decision-making power but also perceptions of the community as a whole, their current socio-economic condition and socio-cultural acceptance. However, successful public health restrictions also depend on the appropriateness of the regulation in regional and local contexts, which may vary temporally and in spatial ways.4 This is particularly true for nations with enormous geographical and population diversities like India.
Social science research engages in the critical analysis of the socio-cultural phenomenon. It throws light on local people’s preparedness and perception of diseases, acceptance of public health protocol, trust towards public healthcare facilities, and influence of indigenous/traditional belief systems on healthcare-seeking behaviours.5 Paul Farmer, American Medical Anthropologist and Physician, designated this approach as “critical anthropology of emerging infection”. Later, this approach was used in anthropological research several times, specifically during public health outbreaks.6 The Farmer’s call has also been tested and received successful results during the Ebola disease outbreak in Guinea, Liberia and Sierra Leone during 2103-16, Zika virus disease in North, Central and South America, Pacific Islands, and Southeast Asia between 2015-2016 and cholera epidemic in Yemen in 2017.7,8,9 In recent times, anthropologists are getting involved more in finding out the social-cultural pathways of different infectious diseases. This cultivation not only enhance the knowledge of anthropology but also makes a solid footmark on the action-oriented public health emergencies research in the era of multidisciplinary approaches devoid of imposing the disciplinary boundaries during an urgent health crisis.10 Against this backdrop, the present article discloses some crucial questions in public health emergencies and the involvement of Indian anthropologists. Also, it highlights the current challenges and future opportunities for Indian anthropologists to engage their research in this emerging domain of public health research. It outlines the basic concept of a public health emergency, the historical background of public health emergencies in India and the preparedness of the people, the anthropological role in dealing with public health emergencies, especially methodological challenges and opportunities, and the role of Indian anthropologists in public health emergency research so far and a brief description of a case study during COVID-19 pandemic for understating local people responses regarding institutional trust, preparedness and behaviour measures for COVID-19.
METHODOLOGY
For the present study, both secondary and primary data were used. To obtain the secondary data, a specific literature review was done using the key word “Public Health Emergencies”, combined with “Public Health”, “COVID-19”, “Anthropology”, “Preparedness”, “Response”, “Medical Anthropology”, “World Health Organization (WHO)”, “Pandemic”, “Infectious Diseases” and “India” on PubMed and Google Scholar from April 2020 to September 2021. A manual search for relevant materials, and examined articles from several nonacademic sources (e.g. news, websites, etc.) was also used for the analyzing the facts. Finally, PRISMA guidelines were used to screen the related articles, to obtain primary data, the qualitative survey was carried out in a Santal village, “Majhi Kadamdih”, located in Balarampur block, 35 km southwest of Purulia district town of West Bengal, India. The study was initiated through secondary data search and then used telephonic interviews and WhatsApp messages for data collection from April 9-22, 2020 as used by Drabble et al11 A structured schedule was used to collect the data involving locally trained volunteers from the village. The objective was to find out the community preparedness and response to COVID-19. The specific questions were asked to the 100 adults’ villagers for conceptualizing the institutional health trust, preparedness and behaviour measures for COVID-19. Verbal consent from all participants was obtained prior to this survey. I chose my key informant on the basis of rapport from previous fieldwork in the said regions for the last three years. Therefore, the primary data collection survey was done using the digital ethnography method. Underberg and Zorn defined digital ethnography as a method of “representing real-life cultures through combining the characteristic features of digital media with the elements of story”.12
RESULTS AND DISCUSSION
What is a Public Health Emergency?
Public Health Emergency (PHE) is a state of exceptional threat condition due to outbreak of specific illness or disease or health condition due bioterrorism, epidemic or pandemic disease, or novel and highly fatal infectious agents. There is a high-risk situation of getting infected by many human populations in a short period, which causes substantial human fatalities or long-term disability. This is a unique situation where public health personnel go beyond the conventional public health approaches to promote and protect the health of people and the communities where they live, learn, work and play. The public health emergency of international concern is defined during the 2005 World Health Assembly under International Health Regulation (IHR) as:
An extraordinary event which is determined, as provided in these
regulations:
• To constitute a public health risk to (an) other State(s) through the international spread of disease;
• To potentially require an orchestrated international response.
This specific definition focused on three astonishing words as, “serious”, “unusual”, or “unexpected”, which engaged not only public health action and promotion within the state or national boundaries but also urged instant international action. This is the specific urgency to the government to take immediate action by implementing the public health emergency law, which alters the current state regulation and imposes a new way of action to combat urgent health crises and ensure efficient governance in an emergency.13 It requires a well-organized “Strategic Information and Response Center on Health Surveillance” and well-equipped “National Public Health Emergency Alert and Response Network”. The nation should have specific guidelines for preparedness and responses to overcome health emergencies. WHO proposed only three phases of public health emergency action as (i) pre- preparedness, (ii) Response, and (iii) Recovery. On the other hand, Centre for Disease Control (CDC) divided the actions into the six intervals sequentially as (i) Investigation (ii) Recognition (iii) Initiation (iv) Acceleration (v) Declaration (vi) Preparation.14,15,16 However, both agreed to prepare mitigation through nonpharmaceutical intervention (NIPS) by involving people and communities’ mitigation strategies like physical distancing, wearing masks and hand washing apart from getting vaccinated and taking medicine. Therefore, understanding socialites and culture cross-culturally may be a prerequisite to promoting the NIPs in sustainable ways during public health emergencies.17 In this context of the current COVID-19 pandemic situation, eminent anthropologist Nichter18 stated that “This is not a onetime unforeseen pandemic –we need to invest in preparedness and rapid response systems. We must be prepared for a future in which emerging and re-emerging diseases are expected”.
Based on WHO data and Sands et al,19 the major emerging and re-emerging infectious diseases outbreaks for the last two decades like Severe Acute Respiratory Syndrome (SARS), ZIKA virus, H1N1 Influenza, Ebola, Middle-East Respiratory Syndrome (MERS) and finally COVID-19. Firstly, it is observable that the intensities of epidemics and pandemics have been higher in the last decade than in the previous decade. Secondly, even the medical facilities (including drugs, diagnostics and vaccines) develop day by day. Over the last decades, there have been enormous challenges in controlling over repeated infectious diseases outbreaks. Infectious disease outbreaks that turn into epidemics and potential pandemics can cause massive loss of life and substantial economic disruption. Therefore, adopting appropriate behaviours in the time of public health emergency among the community members and strong state governance are essential in the coming time.
Public Health Emergencies and Preparedness in India
India is the 7th largest nation in the world. It is a land of diverse ethnic and religious groups with a rich kaleidoscopic cultural heritage. It has a distinctive geographic region and contrasting physical environments, from mountains in the north to sea in the west and east. It contains varieties of different ecological niches and divergent backgrounds. However, the rapidly changing environments and anthropogenic activities may lead to subsequent disasters and public health emergencies in recent times. The disaster may be natural or artificial. Although the nation and state have limited control over the occurrence of natural disasters like earthquakes, floods, landslides etc., they may have the power to mitigate the hazards after such natural disasters by optimizing the preparedness of the human communities through knowledge generation and its promotion along with ensuring the health facilities for immediate action.20,21
On the other hand, manufactured disasters like hazardous material spills, fires, groundwater contamination, transportation accidents, structure failures, mining accidents, explosions and acts of terrorism might be avoidable by making the rigid state and national governance structure and monitoring regularly intervals. The “Bhopal Gas Tragedy” in 1984 was India’s first major industrial disaster, and it was also considered the world’s worst disaster. Immediately after the incident, more than 3800 people died due to poisonous gas, along with over 2,000 animals were killed by the gas that night, most of the livestock that people relied on for food. The heavy gas was absorbed into local rivers, making the water undrinkable and poisoning the fish. This situation has created a condition of a public health emergency. Soon after the tragedy, local hospitals were overwhelmed, and doctors tried hard to find out the nature of gas involved in such bodily injury.22 Srivastava23 described that incident by stating that “The city had four major hospitals, but there was a shortage of physicians and hospital beds. There was also no mass casualty emergency response system in place in the city”. Therefore, there was a lack of plans for public health emergencies. After that tragic event, the government realized to establish sufficient public health infrastructure when hazardous industries chose sites for manufacturing plants.24
In the case of infectious and contagious diseases as the leading causes of public health emergencies throughout the globe, India is also experiencing the degradation of the natural environment and under-preparedness of healthy behaviour, which has increased the chance of man-vector interaction. This condition is often reflected in public health hazards like anthrax, cholera, plague etc. WHO listed a sizable number of public health emergencies of infectious and communicable diseases in India during the new millennium specifically for generating knowledge and creating awareness’s of the global community for their preparedness and healthy responses under the International Health Regulation (Table 1).
| Table 1. Public Health Emergencies in India during New Millennium |
|
Year
|
Disease |
Area/State
|
| August, 2001 |
Cholera |
121 sample positive from 5 districts of Odisha |
| February, 2002 |
Pneumonic plague |
16 cases in Hat Koti village, Shimla district, Himachal Pradesh |
| June 2003 |
SARS |
3 probable cases , one each from Karnataka, West Bengal and Gujrat |
| November, 2003 |
Dengue |
2185 laboratory confirmed cases of dengue fever have been reported in Delhi |
| May 2005 |
Meningococcal Disease |
Cases is at 368 with 37 deaths (Case Fatality Rate=10.1%) in Delhi |
| September 2005 |
Japanese encephalitis |
1145 cases of have been reported from 14 districts of Uttar Pradesh Province |
| October 2006 |
Chikungunya |
The affected states are Andhra Pradesh, Andaman & Nicobar Islands, Tamil Nadu, Karnataka, Maharashtra, Gujarat, Madhya Pradesh, Kerala and Delhi |
| May 2017 |
Zika virus |
3 cases have been reported in Bapunagar area, Ahmedabad District, Gujarat |
| July 2018 |
Nipah virus |
19 cases was localized to two districts in Kerala State: Kozhikode and Malappuram |
| January 30, 2020 – September 13, 2021 |
COVID-19 |
33,26,4175 cases and 442,874 death throughout India |
| September 24, 2021 |
Nipah virus |
An single case in Kozhikode district, Kerala state, India |
| Sources: World Health Organization (WHO)56,57 |
It is noted from Table 1 that public health emergencies in India in the context of the global community’s awareness occurred in a regular interval, either in a small prevalence or confined to a specific region. The local health personnel for the rapid response team has acted positively and resisted the further spread of those diseases. For example, in July 2018, the case of the Nipah virus was mainly confined to the Kozhikode and Malappuram districts of Kerala. As the prevalence of the disease was small and limited to the specific district, the state and national medical experts have visited that places and generated awareness and best practices of combating the virus attacks from fruit bats. These all are considered as an epidemic in the Indian context. Still, the scenario is entirely different in the case of COVID-19, a current pandemic throughout the world and unprecedented public health emergencies with a chance of more than 30 million cases and 0.4 million death in India up to 13th September 2021. A similar kind of devastating influenza epidemic happened in India during 1918. It is considered to be the worst epidemic in the 20th century in India. It is also thought that more people were died due to this influenza epidemic compared to the total causalities of the First World War.25 Hardiman26 showed that western India, mainly Maharashtra and Gujarat, was affected the most. This influenza 1918 epidemic changed the course of the people from west India, specifically indigenous groups who lived in extreme poverty. The local indigenous people from southern Gujarat contextualized the influenza epidemic in their culture and termed that incidence as “Manmodi”.
To tackle these kinds of public health emergencies, the nation needs a complete preparedness plan through the public health care system, community engagement and individual responses. The responsibilities do not only lie to the government but also every citizen of the nation. However, this is a continuous learning process, where planning, implementation, reformulation and correction in action are often requisite. Indian public health care infrastructure has a mixed health care system incorporating public and private health care providers. In general, the urban population is majorly dependent on private health care facilities.27 There is no doubt that India has several comprehensive health and nutritional plans for mother and child health, but the pace of achievements of the targets is comparatively slow. Rural groups are facilitated by the public healthcare infrastructure, developed as a three-tier system (Sub-centers, Primary health centres and community health centres). The direction of the healthcare planning always comes from the top as national and implemented into the village level through primary health centres (PHC). In contrast, feedback of the implementation comes from the reverse direction as from the PHC to the national level.28,29
Does the question come whether these health infrastructures and community involvement are sufficient to deal with public health emergencies in India? The picture of the current scenario exposed during the COVID-19 pandemic. In this context, Chatterjee30 reported in The Lancet Infectious Diseases on 17th April 2020 that “Under-investment in public health-care system poses a challenge to India’s COVID-19 containment plans”. India’s investments in health were 1.5% of the GDP, which is considered one of the lowest investments around the world. People more trust private practitioners rather than public healthcare facilities when they are felt sick. Therefore building trust is one of the significant challenges during public health emergencies in India. The state of Kerala is a little bit exceptional. The state investment in health is comparatively higher in Kerala than in other states in India, along with solid implementation plans during public health crises like community participation, volunteer engagement and awareness generation through radio and local languages.31
Another area of concern in public health emergencies in India is the lack of legal architecture. India has no rationally structured legislation even though a public health bill was already drafted in 2017 but not implemented yet. Along with it, India follows the 124-years-old Epidemic Diseases Act of 1897 and Disaster Management Act 2005 to combat the current pandemic issue, which is also debatable.32 Therefore, it is expected for the citizen of India to follow healthy behaviour at the time of public health emergencies in a particular way. To put the right direction for healthy behaviour during health crises, there is a need to understand community behaviour, traditional norms and values, and other socio-cultural and economic factors even in the micro-level community. In this context, social scientists, Anthropologists, in particular, have proved themselves as one of the potential players in public health emergencies, specifically for successfully resisting the outbreak of infectious diseases.1,33
Anthropology in Public Health Emergencies
Anthropology, the systematic and scientific study of human adaptation, variation and evolution based on time and space, has its central focus on the study of human biology and culture in an integrated way. Anthropologists are trying to understand the fundamental question of human origin in this globe. They reveal any subject matter in multidimensional ways through their holistic approaches. Within the capacity of anthropological understanding, the study of social practices in public health and specifically health emergencies like health and hygiene behaviour is often encountered by those anthropologists who study the health and disease of the community. This kind of approach is traditionally considered the approach in medical anthropology and concentrates on micro-level communities’ world-wide. However, in the mid-1980s, during the redefining of the scope of medical anthropology, there was a paradigm shift from narrow focus as mere cultural brokers for mainstreaming public health to macro-level of political economy, the national level of political and class structure, institutional level of the health system, community level of popular and folk beliefs and actions, micro-level of illness experience, behaviour and meaning.34,35 That was the rise of the concept of critical medical anthropology. Parker et al36 argued that we need to focus on the ‘anthropology of public health’ passionately, which not only deals with ill health conditions and deprivation of people but is also committed to understanding the phenomenon by analyzing the event critically, keeping in mind the beliefs and practices of all stakeholders. Recently Hahn et al3 clearly stated that “Anthropological approaches are recommended to address several facets of public health practice: problem analysis, intervention design, evaluation, and the public health enterprise itself”.
Public health emergency is a specific state of public health practice, which Paul Framer (Physician cum Anthropologist) designated as “critical anthropology of emerging infections” in 1996 specifically for the most vulnerable population throughout the world.37 Framer and his colleagues founded non-governmental organizing in 1987, namely as “Partners in Health”, and called for “Aggressive Preparedness” during health emergencies without negotiating disciplinary boundaries.38 The application of anthropological knowledge, as well as methodologies, is gaining momentum during the recent large-scale outbreaks of Ebola virus disease (EVD) (2013- 2016; Guinea, Liberia and Sierra Leone), Zika virus (2015-2016; North, Central and South America, Pacific Islands, Southeast Asia) and cholera (2017; Yemen). The public health practitioners felt the need for an Anthropological understanding to examine the specific socio-cultural pathways of these infectious diseases and barriers to healthcare practices to resist the spread of the conditions.10 In this context, Dr Cheikh Niang, an African eminent medical anthropologist, raised his voice for anthropology based on reality. He helped the WHO to sort out the Ebola problem in Western Africa. He argued that listening to people and helping them adapt their customs are essential in the fight against Ebola in Western Africa. After that, he was considered one of the prime team members for framing the policies of WHO during public health emergencies.39
In this regard, one of the leading Anthropological forums, American Anthropological Association, has formed a group titled “Anthropological Responses to Health Emergencies (ARHE)”. It is a Special Interest Group (SIG) for Medical Anthropology. The primary purpose of this group is to form a network among the members to advocate and respond to the sudden outbreak of different public health issues and emergencies. They devote themselves to knowledge generation, raising awareness to limit human suffering in the context of epidemic or pandemic outbreaks. SIG started to nurture the Zika virus and measles outbreaks and vaccine hesitancies among the general population and was recommended to the world population. During COVID-19, this group responded to its capacity.40 Ennis-McMillan et al41 two active members of that group, gave the anthropological response to COVID-19 control for aggressive preparedness and response towards communities. They traced the constructive cultural model of COVID-19, how people build stigma and so-called “othering” in the Pandemic, what kind of responses are required to health communication and social surveillance, and finally traced the importance of pandemic response to local people governance”. Besides, they suggested looking at the pandemic and health emergency issues through co-morbidity and syndemic approach as also proposed by Singer,35 where the socio-cultural facet is considered an essential wing. Based on the infield experiences during the Ebola epidemic of West Africa, 2014-16, Kutalek and Jong stated that “The Ebola outbreak has proven the necessity of culturally sensitive responses in a setting where public health systems are overwhelmed”. This may be the core of anthropological work and the unique style of applying participant observation as a vital tool in Anthropological literature.42 The primary question arises regarding the methodological implication in a public health emergency, where an ethical approach should be ensured during the intervention.
In the broader sense, anthropologists study social phenomena holistically. They observed the human attitudes and behaviours based on empirical reality in the field and tried to discover the interconnections between communities, institutions and environments. They maintained a valued social system and community ethics.43 They have their fundamental research method as participant observation, where they consider themselves as both member of the communities as well as observers. They often systematically describe their observation in the form of ethnographic accounts, which include evidence of the ways of living of the community members, even in terms of health behaviour and attitudes. This evidence-based health behaviour and attitudes may be used for clinical and public health interventions. However, the time considered for formulating ethnographic accounts requires a long approach, which may not be suitable for public health emergencies. Therefore they need some rapid tools for evaluating the attitudes and behaviours of the people, specifically during a health crisis. “Rapid Assessment Procedures” and Knowledge, Attitudes and Practices Survey are the two essential methods in this regard. These tools are well-defined, validated and smoothly executed previously for combating health emergencies. These methods may help unfold the crisis rapidly instead of analysing the interconnectedness between different social phenomenons in-depth.44,45 Médecins Sans Frontières (MSF),46 for example, have developed rapid assessment tools using qualitative methods to assess household, community and structural aspects to ensure a more comprehensive approach to understanding potential vulnerabilities for people in crisis. Now it is crucial to find out the specific roles of anthropologists in public health emergencies. Stellmach et al10 critically discussed two fundamental questions, i.e. what are the merits of involving anthropologists and what are the demerits or beyond the scope of anthropological approach during public health emergencies. He showed that anthropologists could be involved in different public health emergency research steps based on need, characters, and specialisation.
Anthropologists are suitable for designing the effective public health emergency programme and formulating the research design. They may also involve interpreting the local norms, and investigating the culture understating the health crisis and responsive behaviour of the community members. They may again apply in event analysis and post hoc assessment. One of the classic examples of formative research was the exploration of structural determinants of HIV infection in Haiti by Paul Framer.47 While Nichter48 critically described that when the government viewed the disease as a virus attack, the rural villages recognized the viral outbreak as a culturally constructed socio-politically governed “disease of development”. During the Ebola outbreak, anthropologists showed the absolute power to use the fundamental academic methods, data interpretation and theoretical orientation for policy advocacy of public health emergency in combating the Ebola disease.2 However, anthropological knowledge and action may not suit an extreme and immediate health crisis, which often results from natural disasters.49
Indian Anthropologists and Public Health Emergency Research
Research in public health emergencies and advocacy is rarely done by Indian anthropologists as public health emergency events also infrequently occur in India. On the other hand, the involvement of anthropologists and other social scientists in public health emergency planning and programme in India is sporadic. There is hardly any anthropologist involved in the Indian Council of Medical Research (ICMR) Rapid Response Team for COVID-19, formed during the early stage of the health crisis during the current pandemic.50 However, several academic discourses happened in the form of webinars since the beginning of COVID-19 in India. For instance, on 7th July 2020, the Department of Anthropology, University of Delhi, India, organized a webinar on “Anthropological Response to COVID-19” to unfold the multidimensional nature of the Pandemic. In that platform, a number of anthropological thoughts have been explicitly discussed in COVID-19 prevention and management angles and its impact on mental health. Anthropologists were exchanged their knowledge and views of the socio-cultural and economic negotiating nature of lockdown and physical distancing during the pandemic. They also contributed to the discussion on the genetic and epigenetic implications of COVID-19.51
Moreover, the major challenge identified by the participants was the anthropological fieldwork. In this regard, digital technology may be the only need-based solution but it is debatable in its functional appropriateness and approaches in anthropological research. However, the issues of Anthropological application in public health or emergencies lie in medical anthropology approaches. During the current pandemic, Adams et al52 explained Anthropologists’ jobs under such health crisis conditions. They said we should observe experience, participate, and write critical insights into apparent and implicit situations. In this connection, India has had a great tradition of nurturing and conceptualizing medical anthropology for more than ninety-years, as stated by eminent Indian medical anthropologists Professor Joshi.53 He explained that the journey began in 1923 by S.C. Mitra (a social anthropologist from the University of Calcutta), who wrote: “On the Cult of the Godlings of Disease in Eastern Bengal”. At the same time, P. O. Bodding published on Santals’ indigenous concept and beliefs of disease in 1925. The appropriate blending of science and tradition, medicines and ethno-medicines; anthropology and public health, and above all, indigenous wisdom and clinical practice in the promotion of the health of India’s people would go a long way in providing accessible, affordable, equitable and culturally routed health care. However, he did not emphasis the public health emergencies and the contribution of Indian Anthropologists due to apparent reasons, as stated earlier.
A Case Study during COVID-19 Pandemic
Based on the above discussion, it has been established that there is a specific role of anthropologists during public health emergencies, and there is a dearth of study in India, which requires applied and action-oriented approaches rather than building only the theoretical understandings like Conspiracy Theories on COVID-19 for Preparedness Programs.54 The current pandemic opens a new academic environment and novel thinking for anthropologists to look critically into different challenges public health personnel face. Some of the obstacles are fear of isolation/quarantine by the rural and remote communities, non-acceptability of rural healthcare services, rumors and fear of policing, stigma, unknown co-morbid conditions, accepting of migratory labour in their native settlements, and relaxing attitudes towards COVID-19 physical restrictions and hygiene practices and so on. To unfold the inner dynamics at the community level, one has to probe an in-depth study. We have done one pilot study in the Purulia district of West Bengal State in India using the digital ethnographic method.
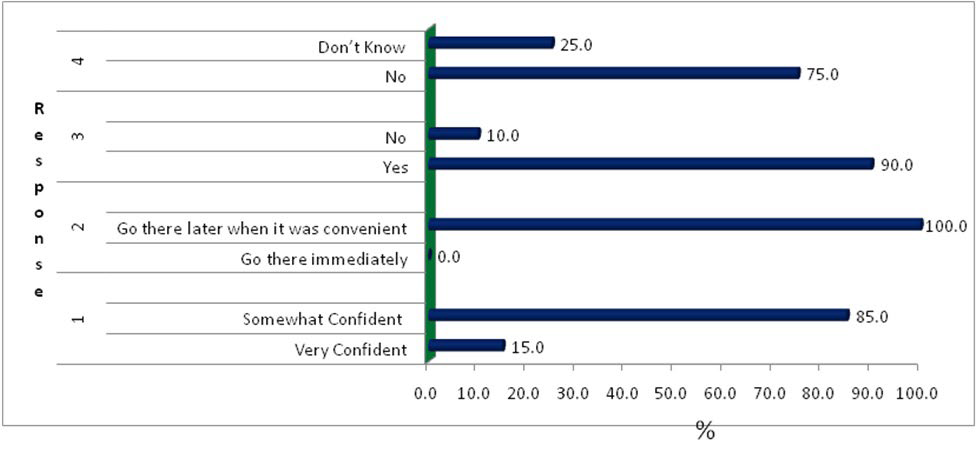
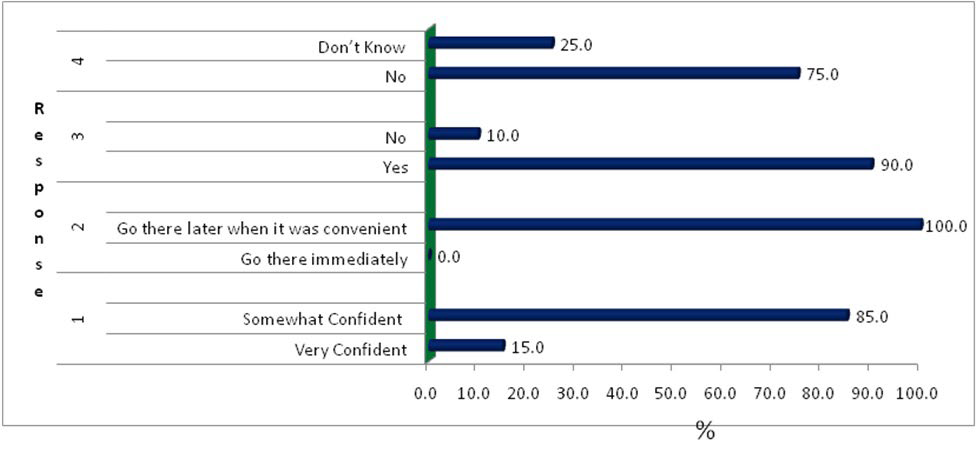
From Figure 1, it was clear that the Santal villagers were underprepared to tackle the COVID-19 pandemic. They were not confident in their primary public health care system. They would have tremendous fear regarding isolation if they asked to go into quarantine. However, they had enough food for their consumption, but they were entirely unaware of the unpredicted nature of the COVID-19 pandemic. They conceptualize the pandemic in their ways, primarily through cultural construction, evident in their initial ritualistic behaviours.
Figure 1. Percentage Distribution of Responses Regarding Institutional Trust, Preparedness and Behaviour Measures for COVID-19
One of the key informants told us that-
“Every Santal village of Purulia district have initially performed the worship of the Deities [Marag Buru and Jaher Era] in the traditional worship place [Jaher Than] right after the Lockdown. We[Santal villagers] prayed together to our traditional god and goddess to save from these unknown disease threats, and if we will able to resist it, we will perform a grant feast and worship in our Jaher Than.”
The findings from this study highlighted the urgent need for awareness generation regarding the COVID-19 response among the studied Santal group and building the truest towards the public healthcare system. Social scientists, specifically anthropologists, who have micro-level visions, deal with the community from their socio-cultural points of view to overcoming the challenge. Moreover, despite the government initiative to distribute food during the initial lockdown, the community members engaged in distributing rice from the platform of the “All India Majhi Forum of the Santal community”, mainly to their underprivileged households, not only the Santal group but also to the other neighbouring community members. Rascouët-Paz55 asked Anthropologists “Anthropologists helped during Ebola. Could they help now?”. It also framed the challenges towards the Anthropologists for their motivating and scientific approaches for public health emergencies. These will be the learning opportunities for anthropology in the future, especially for Indian anthropologists to put their foot for holistically public health emergency research.
CONCLUSION
There is an insightful connection between anthropological research and public health emergency, specifically in local people’s preparedness and response during sudden health crises. Based on world literature, it was observed that anthropologists substantially contribute to finding out the social-cultural pathways of emergency diseases and interprets the phenomenon in bio-cultural ways. Yet, the contribution of Indian anthropologists is limited, possibly due to not recognising anthropological knowledge during an emergent health crisis by the public health sector. COVID-19 opens up anthropologists’ opportunities to contribute to this new dimension of research with their robust methodology and rich historical literature on indigenous beliefs and practices of diseases in the coming time.
ACKNOWLEDGEMENTS
I would like to express my sincere gratitude to the study participants.
FUNDING
None.