INTRODUCTION
Sarcoidosis is a multi-system inflammatory disease with an unknown etiology that impacts quality of life (QoL) and can lead to end organ failure.1 Sarcoidosis can be difficult to diagnose because its clinical presentation can reflect an array of varying etiologies, such as tuberculosis, lupus, idiopathic uveitis, and granulomatosis with polyangiitis.1,2 It is important to identify sarcoidosis to provide appropriate treatment that targets its pathogenesis of the inflammatory formation of non-caseating granulomas. Sarcoidosis can commonly present with fatigue, fever, weight loss, cough, dyspnea, chest pain, uveitis, erythema nodosum, and joint arthritides.1 Its initial presentation can be asymptomatic and be detected incidentally on chest X-ray. There are varying tests that can help guide a diagnosis for sarcoidosis. These include: laboratory tests, such as angiotensin-converting enzyme levels, radiographs, such as chest X-rays demonstrating bilateral perihilar lymphadenopathy, and histopathology showing non-caseating granulomas.1 Once diagnosed, first-line treatment for sarcoidosis is prednisone. Second-line treatments include methotrexate or hydroxychloroquine, and third-line treatments include infliximab or adalimumab.3
CASE PRESENTATION
The patient is a 73-year-old male with a past medical history of diastolic heart failure (ejection fraction of 55% as of May 2022), atrial fibrillation, cerebral vascular accident/transient ischemic attack, Type 2 diabetes mellitus (T2DM), hypertension and hyperlipidemia who was brought to the emergency department (ED) by family due to confusion, light-headedness, nausea and vomiting for the past two-days. In addition to the above, the patient is also experiencing worsening fatigue, a 30-pound weight loss over the previous three to four-months, and shortness of breath (SoB) on exertion for the last 2-months. The patient denied orthopnea, paroxysmal nocturnal dyspnea, bilateral lower extremity edema, hematemesis, melena, and diarrhea. The patient did not report any use of oxygen at home. Social history includes a 30 pack-year smoking history, quitting 10-years ago. Patient’s home medications included aspirin, atorvastatin, buproprion, digoxin, duloxetine, lisinopril, metformin, metoprolol, torsemide, rivaroxaban, insulin aspart 40 units three times daily and insulin glargine 70 units twice daily.
The physical examination was significant for an ill-appearing patient. Cardiac examination revealed tachycardia with an irregular rhythm. Mild bipedal pitting edema was noted. Pulmonary examination revealed that the lungs were clear to auscultation bilaterally. Remainder of the physical exam was unremarkable. Complete blood count revealed eosinophilia (78%), leukocytosis (29,700/uL). Complete metabolic panel revealed a non-fasting glucose level of 67 mg/dL, creatinine was 2.56 mg/dL and calcium was at 12.1 mg/dL. Urine analysis revealed large leukocytes, positive nitrites and numerous bacteria.
Given the results of the patient’s urinalysis and complete blood count, the patient was diagnosed with delirium secondary to acute cystitis. His hypoglycemia was attributed to poor nutrition. In terms of the hypercalcemia work-up, the patient’s ionized calcium was 1.49 mmol/L, parathyroid hormone (PTH) was<4.0 (below normal reference range), 25-hydroxyvitamin D level was 32 ng/dL (within normal limits) and 1,25-dihydroxyvitamin D level 78 pg/mL (elevated), respectively. Despite being adequately treated for five days, the patient’s leukocytosis did not improve, and antibiotic regimen was broadened for treatment of presumed sepsis.
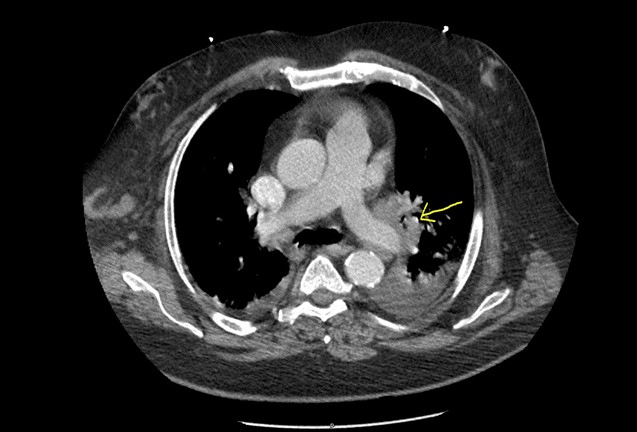
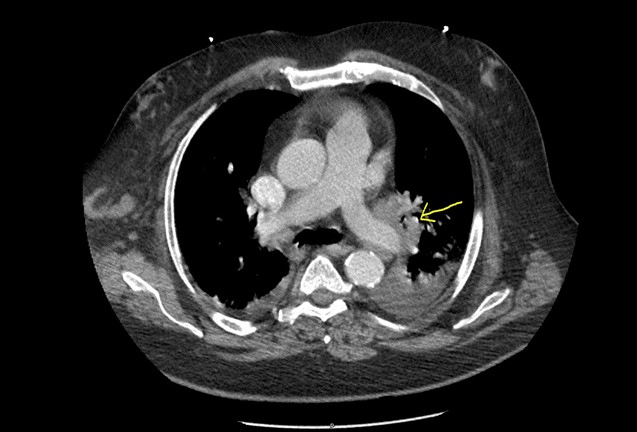
With no clinical significance, elevated 1,25-dihydroxyvitamin D and hypercalcemia made clinical suspicion high for lymphoma or sarcoidosis. Granulomas in sarcoidosis express high-levels of 1-alpha hydroxylase, the enzyme that catalyzes the hydroxylation of 25-hydroxyvitamin D into its active form, 1,25-dihydroxyvitamin D. This in turn leads to the hypercalcemia seen in this disease. Computed tomography (CT) of the chest, abdomen, and pelvis revealed extensive lymphadenopathy (See Figure 1: Hilar lymphadenopathy yellow arrow]. Oncology and pulmonology were consulted for lymphadenopathy and eosinophilia. Antibiotics were discontinued as infectious etiology was ruled out. Several tests, including serum immunoglobulins, histoplasma galactomannan urine antigen, and strongyloides immunoglobulin G (IgG) antibody were unremarkable. Sputum culture for acid fast bacilli and fungal organisms were negative. Interventional radiology was consulted for lymph node biopsy. Right axillary lymph node biopsy results showed no evidence of malignancy but did show chronic granulomatous inflammation. No eosinophilia was appreciated.
Figure 1. CT of the Chest, Abdomen and Pelvis
A serum antineutrophilic cytoplasmic antibody (ANCA) vasculitis panel was drawn and was negative, ruling out eosinophilic granuloma with polyangiitis. After confirming a negative ANCA test, the patient was subsequently started on Prednisone 0.5 mg/kg po daily (60 mg po daily) for treatment of sarcoidosis. Angiotensin converting enzyme (ACE) levels were 26 and 30 units/L, which were within normal limits.
After 12-days in the hospital, the patient was stable for discharge. His calcium was within normal limits (10 mg/dL), creatinine back to baseline (1.24 mg/dL), and eosinophil count within normal reference range (1%). Urine culture did not demonstrate any growth. It is evident that the patient’s overall clinical status began to improve after initiating steroids. The patient was placed on a steroid taper for the duration of a year. Additionally, the patient was prescribed Bactrim for prophylaxis of Pneumocystis jirovecii pneumonia (PCP) in the setting of presumed immunosuppression secondary to prescription of long-term steroid use.
DISCUSSION
As presented above, this is a case of sarcoidosis found incidentally on lymph node biopsy in a patient who presents with light-headedness, nausea, and vomiting in the setting of a persistent leukocytosis and eosinophilia. Given the patient’s significant recent weight loss, dyspnea on exertion, and smoking history, malignancy was a consideration. However, it is important to note that sarcoidosis can present with non-respiratory symptoms. The patient discussed above presented with symptoms that could be due to a myriad of etiologies, whether infectious, malignant or otherwise.3
It is imperative to establish the diagnosis of sarcoidosis as soon as possible in order to promptly initiate treatment. Oral glucocorticoids are the first line treatment, and most patients respond rather well-initially. Despite adequate treatment, however, greater than 10% of patients with pulmonary sarcoidosis develop progressive disease, and the disease itself carries a mortality rate of approximately 7% within a 5-year follow-up period.4
Sarcoidosis should be on the differential in patients who present with persistent leukocytosis and multiorgan involvement, as in the patient discussed above. Multiorgan involvement can enhance the diagnostic certainty but only biopsy showing non-caseating granulomas confirms the diagnosis.5
CONCLUSION
Sarcoidosis is a multi-system inflammatory disease with an unknown etiology that impacts QoL and can lead to end organ failure. The usual patient presents with respiratory symptoms, including exertional dyspnea, persistent dry cough, chest pain, and wheezing. However, in the case report above, the patient did not endorse any of these symptoms. Rather, he presented with light-headedness, nausea, and vomiting. The patient’s leukocytosis persisted despite being adequately treated for sepsis secondary to urinary tract infection (UTI). Imaging and biopsy revealed a granulomatous disease, sarcoidosis. Once diagnosed, the patient was rapidly started on the first- line treatment, prednisone. His symptoms immediately began to improve.
CONSENT
The authors have received written informed consent from the patient.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.