INTRODUCTION
Laser-assisted in situ keratomileusis (LASIK) today is the commonest corneal refractive surgery performed around the world.1 As with every surgical procedure the post-operative complications of LASIK affect the patient satisfaction and outcome of the surgery. Superficial punctuate keratitis (SPK) in the form of superficial punctuate epithelial erosions are one of the earliest complications noted within hours after surgery in the early post-operative period.2,3,4,5 It not only affects the patient satisfaction but can be an early sign of forth coming complications after LASIK. Though the SPKs as a part of post-LASIK dry eye often develops at around 6 months post-operatively, the pathogenesis behind the early post-operative SPKs is likely to be different.2 Damage to the epithelium in such cases is likely to be due to intra-operative methods used to handle the corneal flap. Various pre-operative patient related factors and different intra-operative techniques play an important role.
Pre-operative factors are like an age of more than 40 years, hyperopia, greater corneal thickness, and surface drying during the microkeratome’s pass have shown greater risk of corneal epithelial defects after LASIK.5 Certain intra-operative factors like, use of anaesthetic eye drops, site of hinge of corneal flap, use of microkeratome or Femto Second (FS) laser, thickness of corneal flap, affect the incidence of corneal epithelial defects.
An epithelial defect can increase the patient’s risk of developing Diffuse Lamellar Keratitis (DLK) 24-fold, with subsequent flap striae and epithelial in-growth.6 Hence, early identification of epithelial abnormalities post-LASIK and finding intra-operative factors responsible for the same is important. In present, blunt air cannulas and specialized cellulose sponges like the Weck-cel sponge are being used to manipulate the corneal flap. Weck-cel sponge is commonly used to absorb irrigating fluids and quell the cells. The bed and flap are swept with such lint-free sponges to clear the interface of epithelial and other debris.5 A 27-G blunt cannula is often used to put corneal flap back in position after laser ablation.7 In our study, we found that by using air cannula instead of Weck-cel sponge the incidence of SPK in the form of epithelial erosions can be reduced. This is the first study as per our knowledge to show changes in incidence of SPK post-LASIK by comparing two alternative methods to handle the corneal flap intra-operatively.
MATERIAL AND METHODS
This is a randomized prospective comparative study comprising of 192 eyes of 96 patients undergoing LASIK for myopia or myopic astigmatism in both eyes. Patients were selected for this study after obtaining approval from the institutional review board and ethical committee. An informed consent was taken from the patients. LASIK with femto second laser was performed on both the eyes, in which air-canula was used for one eye and Weck-cel sponge used for the other eye respectively. Two groups, Air canula group and the Weck-cel sponge group were divided. Using simple randomization with SAS software a randomized numerical list was generated for 96 patients prospectively, distributing each eye (right or left) of every patient randomly into either of these 2 groups.
All patients underwent a thorough ophthalmic examination including Uncorrected visual acuity (UCVA), Best Corrected Visual Acuity (BCVA), slit lamp examination, dilated fundus evaluation using +90D and indirect ophthalmoscopy, corneal topography using the keratron scout analyser, wave front analysis using I-design (Abbot medical optics), Schirmers, tear film break-up time, pachymetry and specular microscopy. All patients were prescribed topical gatifloxacin 0.3% (Zymar, Allergan, USA) three times a day, one day prior to the surgery. All patient underwent a femtosecond assisted LASIK using the Intralase femto second (Abbott medical optics) and excimer laser (Abbott medical optics). No microkeratome was used. All the patients had a superior hinge and intra-operatively in the group 1 patients the flap was repositioned using the air canula and in group 2 patients the flaps was repositioned with the help of Weck-cel sponge. All patients were seen at the end of 2 hours after the procedure and the incidence of SPKs were noted and graded using the Oxford scheme as proposed by Bron, et al. by an independent observer who was not aware of the study protocol.8 Patients were put on tapering doses of antibiotic and steroid combination for 15 days and lubricant for a month. All patients were followed up at the end of one week and one month.
STATISTICAL METHODS
Statistical Analysis System (SAS) software was used for randomization of the eyes to either of the groups, Air canula group or the Weck-cel sponge group. The outcome measures in grades were expressed as percentage and compared. To find statistical association pertaining to clinical significance, the data was converted to a binary format as whether clinically significant (>or = grade 3 SPK) or not (<Grade 3 SPK). A Chi-square test was used with 1 degree of freedom to find which surgical technique had an association with higher grades of SPK.
RESULTS
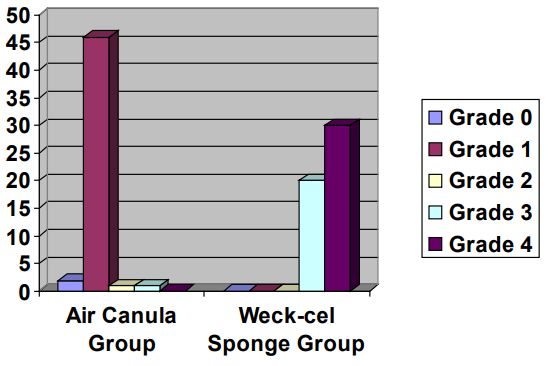
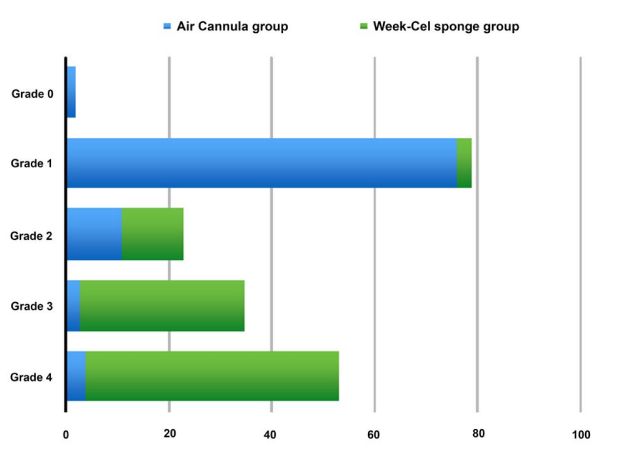
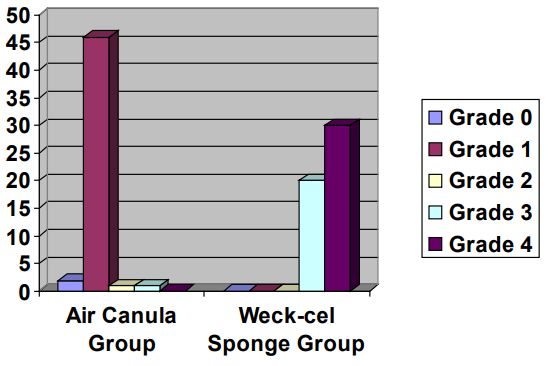
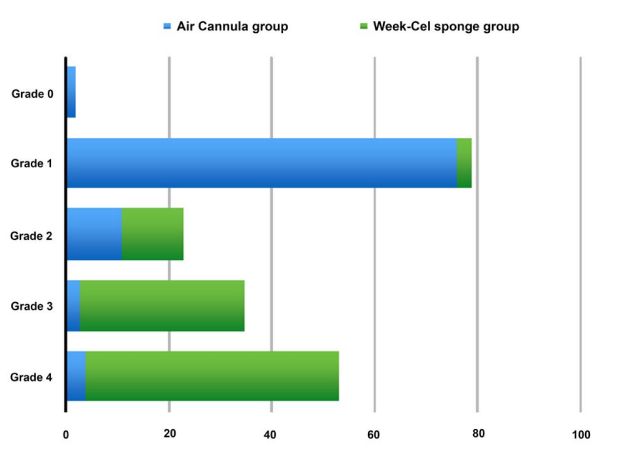
The mean age of the study was 21+/-10 years. Out of total 192 eyes 51(26.8%) eyes showed Grade 4 SPKs of which 49(96%) belonged to the Weck-cel sponge group and 2(4%) eyes belonged to the air canula group. The number of eyes in Weck-cel sponge group with Grade 4 , Grade 3, Grade 2, Grade 1, Grade 0 SPKs were 49(51%), 32(33.3%), 12(12.5%), 3(3.1%) respectively. Similarly the number eyes in Air canula group with Grade 4 , Grade 3, Grade 2, Grade 1, Grade 0 SPKs were 24%), 4(4.1%), 11(11.45%), 76(79.1%), 2(2%) respectively. The number of eyes with clinically significant grades (Grade 4 and Grade 3) in Weck-cel sponge group was 81(84.3%) as compared with 7(7.2%) eyes of the Air canula group. (Graphs 1 and 2)
Graph 1: Incidence of SPKs in air cannula and Weck-cel sponge group.
Graph 2: Grades of SPK in both group.
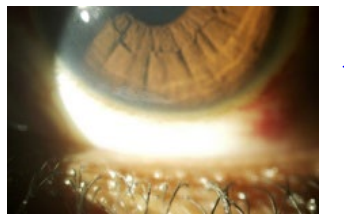
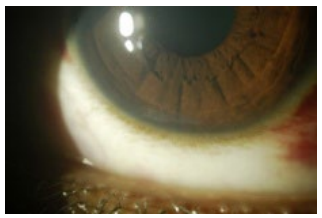
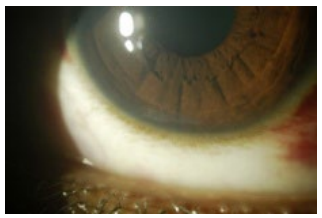
In order to study the association of both groups with clinically significant higher grades of SPK, Chi-Square test was used by considering the outcome as clinically significant if Grade 3 or Grade >3 (Figure 1). SPKs or clinically insignificant if Grade <3 (Figure 2) SPKs were present. The Chi-square test showed the Weck-cel sponge group was significantly associated with the clinically significant grades of SPK (p<0.001) at 1 degree of freedom. So the incidence of higher grades of SPKs in the Weck-cel sponge group is less probable to be due to a chance.
Figure 1: Showing grade 3 SPK.
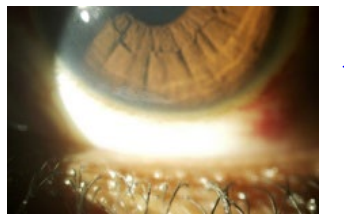
Figure 2: Showing grade 2 SPK.
DISCUSSION
SPKs occurring as a complication of LASIK have been previously described in context with post-LASIK dry eye and neurotrophic epitheliopathy.9,10 Immediately after LASIK, 95% of patients report some dry eye symptoms.11 The LASIK-induced change in corneal shape may affect the relationship between the eyelids and ocular surface and lead to abnormal tear distribution during blinking.11,12,13,14 The main proposed cause of SPKs in post-LASIK dry eye is iatrogenic corneal nerve damage. LASIK disrupts both the dense sub-basal nerve plexus and stromal corneal nerves in the creation of the anterior stromal flap and excimer laser ablation of the cornea.9
Though with the use of femto-second laser the complications associated with the micro-keratome are reduced, an association of use of the laser with the early post-operative SPKs is yet to be determined. SPKs in such scenarios are mainly an outcome of chronic inflammatory environment of the cornea. Adding to which loss of corneal sensations for first few months can play a role in occurrence of late post-operative SPKs leading to a dry eye.9 But whether any of these factors play any role in early pre-operative SPKs is yet to be proven. It is likely that mechanism behind the early pre-operative SPKs are related to immediate intra-operative events. In our case series, we found that SPKs can be found in early pre-operative stage in all LASIK operated cases but their severity differs based on type of instrumentation.
We came across that the incidence of Grade 4 and Grade 3 SPKs are higher with the use of Weck-cel sponge in the immediate post-operative period. Possible reason for the same could be the finely corrugated surface of the sponge which helps it in being porous and absorbing the excess fluid and keeping the corneal surface dry during surgery. Compared with the metal air cannula which happens to be smooth in its surface, handling of the corneal flap could yield lesser damage to the epithelial surface. Since the operative conditions and procedure undertaken were similar for both the eyes in all the cases, it is more likely that the structural properties of the surface of air cannula and the Weck-cel sponge plays important role in the incidence of early post-operative SPKs. Apart from SPKs, many patient related pre-operative risk factors have been associated with the post-operative epithelial defects.15
The intra-operative epithelial defects during LASIK have an association with the age of the patient and duration of use of contact lenses.15,16 With age of the patient more than 40 years the chances of post-operative epithelial defects are more and the chances of the same are more in the other eye after occurrence in the fellow eye.15,16 Intra-operative epithelial defects in the first eye is highly predictive of epithelial defects in the second eye of the same patient. Since this being a first study as per our knowledge to report difference in incidence of SPKs post-operatively after LASIK due to intra-operative factors, an association with pre-operative and patient related factors is what needs to be studied further. In this study, we found that using Weck-cel sponge to be associated with more SPKs in the immediate post-operative period and could affect the post-operative patient satisfaction. Instead an air cannula to manipulate the corneal flap intra-operatively could prevent SPKs with higher grades post-LASIK.
CONFLICTS OF INTERESTS
The authors declare that they have no conflicts of interests.