INTRODUCTION
Lichen nitidus (LN) is rare disorder, with minute, shiny, flattopped papules, usually on trunk and genitalia.1 Actinic lichen nitidus is a photo-induced eruption, with clinical and histologic features of lichen nitidus.2 It is seen commonly in dark skinned patients. It has been termed “summertime lichenoid eruption” previously.3,4 Dermoscopic features of palmoplantar and non-palmoplantar LN have been described scantily in the past. Cutaneous LN showed round, elevated, shiny, smooth surface without scales with reddish vascular network, while palmoplantar LN showed pits with thin scales as well as punctate hemorrhagic variants.5,6
CASE REPORT
A 27-years-old male with type V skin type presented to dermatology out patient department (OPD) with complaints of asymptomatic minute grouped and discrete, skin colored, flat topped papules on dorsal aspect of fingers, knuckles, wrists, forearms, dorsal aspect of legs and face of 3 months duration (Figures 1A, 1B, 1C). Lesions appeared at the onset of summer. Lesions initially started from dorsal aspect of the fingers, with gradual involvement of the forearms and legs. Patient also had a few discrete lesions on his forehead, but oral cavity, palms, soles, nails and genitalia were spared. There is history of appearance of lesions at sites of scratching, with evidence of koebnerization (Figures 2A, 2B). There is no history of itching or oozing from the lesions. There is no significant family history or similar history in the past.
Figure 1. Multiple Skin Colored, Flat-Topped Papules on Dorsal Aspect of Fingers and Knuckles

Figure 2. Discrete Minute Flat Topped Skin Colored Papules on Forehead and Koebnerization on the Leg and Forearm

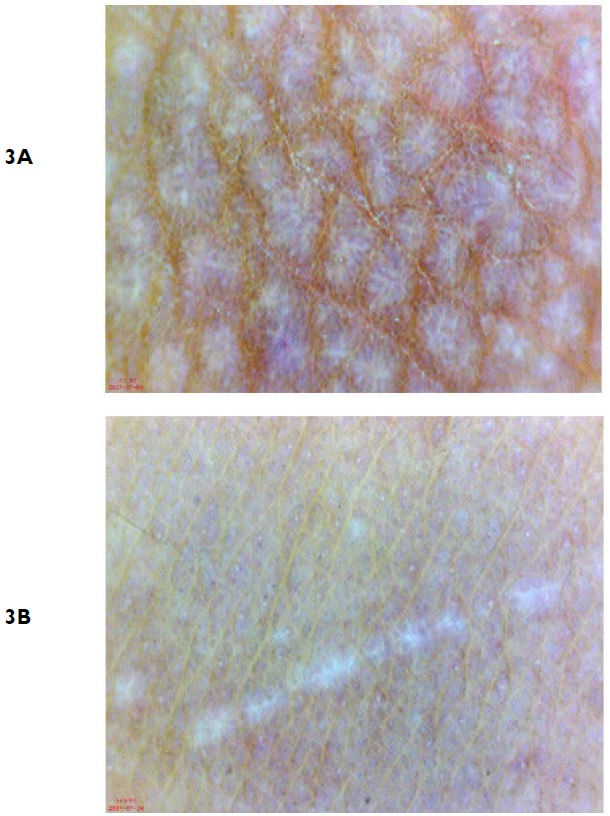
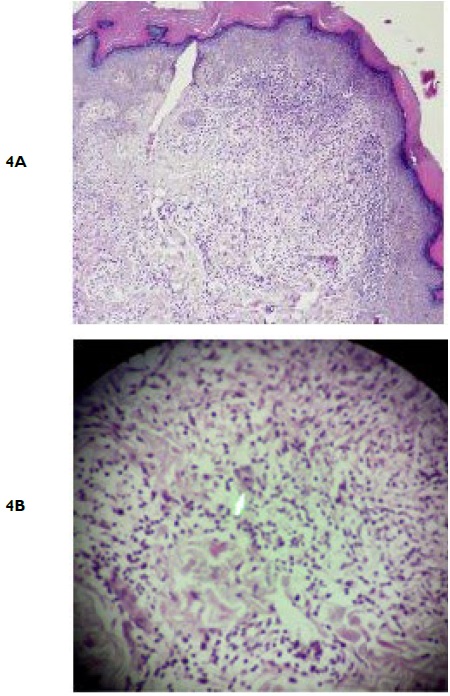
On dermoscopy, we observed shiny, round,bluish white streaks with “fern leaf ” appearance, interspersed between brownish reticular networks (Figure 3A). Areas of koebnerization appeared as shiny linear streaks mimicking “shooting stars” (Figure 3B).
Figure 3. Dermoscopy of Skin Lesion Shows Shiny, Rounded, and Bluish White “Fern Leaf ” Patterns, Interspersed between Brownish Reticular Networks
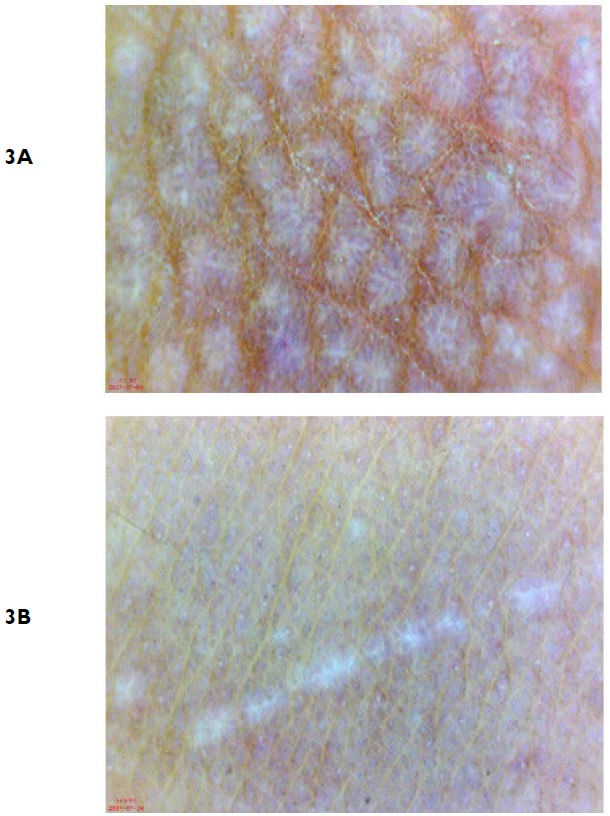
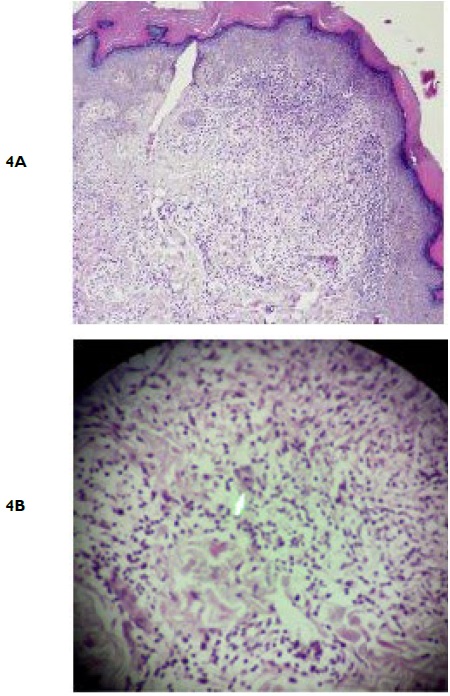
Histopathology was consistent with lichen nitidus. In epidermis, hyperkeratosis, parakeratosis and irregular acanthosis were noted. In the dermis, there was dense lymphohistiocytic infiltrate in an expanded dermal papilla with thinning of the overlying epidermis and downward extension of the rete ridges at the lateral margin of the infiltrate. Few multinucleate giant cells were seen in the infiltrate. There was no wedge-shaped hypergranulosis or basal vacuolar degeneration (Figures 4A, 4B).
Figure 4. Low Power Magnification Demonstrates Lymphohistiocytic Infiltrate in Papillary Dermis with Thinning of Overlying Epidermis, Giving a Typical “Claw Clutching A Ball” Appearance
DISCUSSION
Lichen nitidus was first described in 1907 by Pinkus.7 It occurs mostly in children and young adults, but elderly individuals can also be affected. Clinically, lichen nitidus appears as asymptomatic, discrete, 1-2 mm, flat-topped, shiny, skin colored to brown papules, on trunk, extremities and genitalia.1 Koebner’s phenomenon is frequently seen and some authors regard koebnerization as a “constitutive” feature of lichen nitidus.8 Clinical variants of lichen nitidus include confluent, vesicular, haemorrhagic, palmoplantar, follicular, perforating, linear and generalized.9
Actinic lichen nitidus (ALN) was first reported by Bedi in 1978, as “summer time actinic lichenoid eruptions (SALE)”.3 Later, cases of actinic lichen nitidus with typical histology were described.4,10 Summer time lichenoid eruptions with histologic characteristic of lichen planus (LP) have also been reported. There are interesting reports of subsequent appearance of actinic LP and lichen nitidus in the same patient. However, based on clinical and histopathological differences, ALN and actinic lichen planus (ALP) are distinct entities. Clinically, ALP appear as itchy, erythematous to violaceous annular plaques with surrounding hyperpigmentation, while ALN is asymptomatic, minute, 1-2 mm, skin colored to violaceous discrete papules appearing on sun-exposed sites.9 Histologically, LP has hyperkeratosis without parakeratosis, wedgeshaped hypergranulosis, and basal vacuolar degeneration with dense upper dermal infiltrates. Histopathology of lichen nitidus demonstrates classical granulomatous lymphohistiocytic infiltrates in the dermis, imparting a distinctive pattern of “claw clutching a ball” appearance.9,13
In our patient, typical lesions on sun exposed sites, classical morphology and koebner’s phenomenon, along with histopathological evidence favored the diagnosis of actinic lichen nitidus.
There is paucity of dermoscopic findings of lichen nitidus in literature, although dermoscopy of LP and lichenoid eruptions are abundant. In our case, we noted “fern-like”appearance of lacy whitish streaks among brownish reticular network. Qian G et al5 reported dermoscopy of cutaneous lichen nitidus showed round, elevated, shiny, and smooth appearance surrounded by radial rete ridges and reddish vascular network, while palmoplantar LN have shown pitted and punctuate hemorrhagic patterns.5,6
Interestingly, during dermoscopy of LP, Tan et al14 and Friedman et al15 observed leaf venation or “fern leaf ” pattern indermoscopy of wickham’s striae (WS).14,15 However, larger studies have not noted “fern leaf ” pattern in WS of LP.16,17 Structures resembling this pattern have been described as arboriform or starburst patterns in lichenoid eruptions.18 Hence, we conclude that “fern-leaf ”pattern may be seen in LP as well as lichen nitidus, and more importantly hints towards lichenoid eruptions in general.
Lichen nitidus may not always require treatment. Generalized and actinic variants have been treated with sun avoidance, topical and oral steroids, tacrolimus, phototherapy, acetretin, hydroxychloroquine, etc.1,2,19 Our patient showed significant improvement of lesions with hydroxychloroquine and sunscreen in 6 weeks duration.
CONCLUSION
Actinic lichen nitidus is a rare variant of LN, appearing in summer months. Dermoscopic findings of “fern-like” pattern may aid in the diagnosis of lichen nitidus or lichenoid eruptions in general. ALN responds well to short course oral hydroxychloroquine, along with photoprotection.
CONSENT INFROM STATEMENT
The authors have received written informed consent from the patient.
CONFLICT OF INTERESTS
The authors declare that there is no conflict of interests regarding the publication of this paper.