INTRODUCTION
Technology is sweeping through our society in unparalleled fashion, affecting our day-to-day life, education, social relationships, health care and business.1 In this era of patient-centered care, telepsychiatry (i.e., video or synchronous) facilitates access to care, leverages a wide range of treatments at a distance and provides quality care with outcomes as good as in-person care.2,3 It also provides versatility to health systems by enabling more patient points-of-entry, matching patient needs with provider skills and helping providers work at the top of their licenses.3 Many clinicians are still shifting from doctor-, treatment- and/or clinic-centered care, to person-centered health promotion and patient-centered care–much less adapting to new technologies (e.g., text, apps, wearable sensors, social media). Integrative use of mobile health (e.g., emergency transport linkage to the emergency department cardiologist) and in-time clinical decision support is a goal, yet not a standard practice in many institutions.
The adjustment to technology is informed by the consumer movement, traditional medical practice and the evolution of institutional approaches to incorporate it. In business, technology is a key part of the consumer decision journey, in which people consider life choices, evaluate options, make purchases, develop loyalty and advocate others do the same.4 In health care, clinicians and people make decisions based on perceived needs, resources and experiences.5 While people may conduct their life with technology in-time, health decisions are usually best weighed over time, based on patient-physician discussion and informed by data. More broadly, traditional medical practice and the evolution of science have stood the test of time, similar to the evolution of a country’s development with checks and balances (e.g., U.S. between the executive office, legislature and judiciary system). Academic health centers (AHCs) promote science and stability, but may make decisions about technology incrementally compared to private health care systems.
Globally, health care systems and governmental agencies are emphasizing quality, evidence-based care and are trying to set individual patient, aggregate and population outcomes that can be evaluated by mental health data/indicators.6 This requires services that are acceptable to patients, have metrics that can be measured and approaches that are scalable—all of which depend on technology. System management (e.g., health information systems (IS), information technology (IT), telehealth), facilities and clinics (e.g., labs, home health) and delivery structures (e.g., integrated networks) can play a key role in health care. IT falls into three general categories: clinical information systems, administrative information and clinical decision support (CDS) systems, which are supported by advances in artificial intelligence (AI) and machine learning (ML).7 Incremental often means “adding to” existing options (e.g., scheduling systems, the electronic health record (EHR), telehealth video). For example, technology is added to improve documentation of care or as part of a new clinical service, yet the practical impact on clinicians may be overlooked (e.g., time cost, burnout).8 Unintended consequences often occur in system implementation as trade-offs are made between goals and users’ work practices.9
The field of business has some similarities with health care related to implementation of technology. Both business and medicine have innovators, early adopters, early majority, late majority and laggards.10 However, large businesses and those in competitive industries have had to adopt quickly—to avoid going extinct (e.g., Nintendo).11 Indeed, progressive business practice depends on technology heavily (e.g., banking, marketing, sales). Successful businesses shifted IT from an “add-on” or appendage to a core, integrated foundation with research and development, marketing, production and financing functions—they came to a shared IT-business understanding to use IT as an organizing framework.12 Core components of this model have transformed the work of investment banking and other companies like Cirque de Soliel, L’Oreal and Nintendo.11,13,14,15
This paper is designed for leaders of health care, training/education, and other organizations as a tool to “step back” and see business enterprises and now academic health care systems are integrating IT for service delivery and workflow. It draws from a literature across psychiatry/behavioral science, technology, business and health care (i.e., clinical care, education and administration). It may help the reader learn in three ways, to: 1) understand the foundational principles and processes of business and health care in order to contextualize the role of technology; 2) apply a case example to health care of how IT was used to engage customers in banking, financing and investing (i.e., straight through processing to streamline transactions, reduce errors and manual cognitive processes); and 3) understand the challenges for Health Care systems to implement a shared IT-business-health model rather than incremental none-integrative approaches for clinical care, education and administration.
METHODS
Approach
This scoping review used a literature search of Medline, PsycNET, PsycINFO, Embase, Cochrane, SpringerLink, Scopus, ABI/Inform, Business Source Complete, and Web of Science, using subject headings and keywords along with a manual search of reference lists of articles published by November 2020. The stages in this process have been described as: 1) using a well-defined research question with purpose; 2) identifying relevant studies based on the question and purpose, employing a suitable team; 3) selecting studies based on an iterative process for searching the literature, refining the search strategy, and reviewing articles for study inclusion; 4) charting the data by having at least two reviewers extract information; 5) analyzing reporting, and considering the meaning of the findings; and 6) using preliminary findings to obtain consultation from stakeholders.16,17
The Research Question
The question that guided the review was, “What approaches are successful for health care organizations to integrate technology into clinical and administrative workflow, based on inroads from business?”
The goal was to use identify models of integrating technology into health care practices in addition to traditional clinical informatics approaches, so that clinical, technical, workflow, and administrative factors could be better planned, implemented, evaluated and improved. While clinical informatics is a rapidly expanding area may be central to this process, additional paradigms were sought to facilitate patient-centered care as defined by quality, affordable, and timely health care. For example, effectiveness and implementation science approaches assess acceptability, adoption, feasibility, cost, and sustainability.
Identifying Relevant Studies: The Search Strategy
Search terms were organized in four concept areas akin to a scoping review16 with modifications17:
- Business: adaptive, administrative, asset, break-even, brand, channel, communication, competitive, consolidate, content, corporate, costs, deliver, development, distribution, diversification, equipment, equity, expense, finance, fiscal, fixed, industry, inventory, investment, labor, leadership, liability, loss, management, margin, market(ing), opportunity, organization, outsourcing, plant, product(ion), profit, research, return, service, strategy, sunk, transaction, value.
- Service delivery: access, asynchronous, clinical, clinician, continuity, curriculum, decision, distance, documentation, education, e-mail, framework, learner, learning, measure, monitor, outcome, patient, pedagogy, remote, sensor, share, skill, social media, support, team, text, training, video, virtual, wearable.
- System change: academic, adapt, addition, adopt, alternative, analysis, approaches, assessment, benchmark, center, complementary, configure, data, design, develop, engineer, evaluation, health, implementation, improvement, installation, integration (integrity), long-term, maintain, manage, method, model, modification, operating, optimization, procedure, process, program, quality, phase, process, regulation, resolution, replacement, revision, scalable, science, short-term, simulation, standard, technique, transmission, workflow, utility.
- Technology: app, architecture, bridge, cell, computer, connection, database, development, device, digital, eConsult, e-consult, electronic, hardware, health, infrastructure, information, Internet, medical, mobile, monitoring, network, on-line, protocol, record, registry, software, store-and-forward, structure, system, web-based..
Study Selection
Articles were reviewed by title/abstract, full text review and review of references. The goal was to explore how medicine/psychiatry has integrated technology compared to business, and apply business approaches to health care and training; service delivery rather than production models of business were sought.
Articles were included if they discussed integration of technology into health care and compared literature from medicine/health, psychiatry/behavioral health, business, technology, leadership and health care administration. Articles were excluded if they were restricted to one concept area, did not have data, did not have business or scientific methodology, or if were not in English.
Charting the Data
A data-charting form was not developed and used to extract data from each study, but notes were organized consistent with a narrative review or descriptive analytical methods by each reviewer to extract contextual or process-oriented information from each study. The reviewers then compared and consolidated information regarding content. A qualitative content analysis approach would have been used if there was more content, to make sense of the wealth of extracted data. A descriptive analytical method was used to summarize the process and content information of discussions with experts, in an effort to chart and summarize complex concepts in a meaningful way.
Analysis, Reporting and Considering the Meaning of the Findings
This phase often organizes meaningful results in a table, study by study, with data outlined and consolidated by the authors and expert consensus step, but a thematic analysis was not possible.
A field study approach with unstructured interviews was used to investigate how a Company explores the use of STP. This method allows respondents to express in their own ways and pace without bias.18 To be precise, unstructured interview resembles a conversation more than an interview–thought the questions come from the interviewer–for an open-ended exploration of the issues rather than making assumptions. Sometimes independent and dependent variables already exist within the social structure of a Company under study, and inferences can then be drawn about behaviors, social attitudes, values and beliefs.19
Consultation for Expert Opinion
Expert option was solicited to review preliminary findings, and suggest additional steps to improve the review. The goal was to gain input and perspective from a diverse group of health professionals from business, medicine, behavioral health, health services and technology. Participants were also sought from clinical, administrative (e.g., chairs, deans, leaders of national organizations), health care (e.g., health system director, executive, chief of staff) and technology (e.g., artificial intelligence, developers, engineers, informatics, information systems) sectors.
RESULTS
Literature
The flow chart shows that from a total of 2,710 potential references, two authors (DH, JL) found 2,678 eligible for title and abstract review and found 327 papers eligible for full text review as directly relevant to the concept areas in combination. The authors found 58 papers directly relevant to the concepts and 11 from references searched for a total of 69.
A Historical Perspective: Similarities/Differences Between
Business and Medicine/Psychiatry, in General, and Related to Technology
A business is usually defined as any organization that provides products, services or both to individual consumers or to other organizations.20 The premise is a need for goods and services that satisfy the need, and there is an aim to make a profit and share that with stakeholders who have invested. Leaders steer the functions of businesses, which include research and development, marketing, production, accounting and financing. Businesses operate within in an overall economic system (i.e., market with supply and demand) with risk and uncertainty.
Science and medicine has changed significantly over time,20,21 with the late 19th-20th century bringing a scientific foundation and organized medicine. The focus of medicine as a business started in the 1920s, and later, health care systems, reform of training and other tenets of modern care (e.g., specialization, public health, insurance and governmental funding) appeared. The late 20th-early 21st century has seen corporatization, information revolution, globalization and the era of health care reform. Academic medicine comprises medical schools, teaching hospitals and large multispecialty physician practices and its key roles are: treating complex conditions; advancing medical discoveries for better diagnostics, preventive strategies, and treatments; educating the next generation of physicians; and providing irreplaceable community services.22 Medical research is conducted by sustainable, predictable funding growth for the National Institutes of Health. Specialized clinical care at teaching hospitals includes Medicare finances graduate medical education (GME) for direct costs for physician training and indirect medical education (IME).
The U.S. has a unique system of health care delivery, as most developed countries have national health insurance and governmental oversight.20 It is fragmented with people seeking health care through different means and a constantly changing pattern of financing, insurance, delivery and payment mechanisms with private and public components. The complexity of health care includes education/research, suppliers, insurers, providers, payers and the government. The policy cycle is complex itself, with issue, design, public support, legislative decisions and policy implementation steps. The newest movements in addition to patient-centered care are value-based care and accountable care organizations driven by the Centers for Medicare and Medicaid Service.23,24 Value-based purchasing (VBP) adjustments on reimbursement have been tied to clinical care quality (2013), patient experience (2014), safety (2015), efficiency (2016) and mortality (2017).
Technology, clinical care and competencies: There are continuum of technology-based options used by patients, families, caregivers and professionals. This continuum includes: Internet-based information; self-help/support groups; materials for patient and clinician education; social media; self- and clinician-assisted self-assessment; asynchronous text, e-mail and video options; mobile health with apps; and synchronous video (i.e., telepsychiatry) (Table 1).25,26 Technology helps users with goals, and systems may help reduce liabilities of technologies for consumers and patients by standardizing approaches. The spectrum reflects a shift to patient-centered care – and person-centered care27—empowering the whole person behind the patient.28,29 These movements put business and medicine on a common ground—helping the person/customer/patient with quality service/care. This shift parallels past trends in banking, as people have used automated teller machines (ATMs) instead of banks/tellers, though health care is more complex than that.
| Table 1. E-Behavioral Health Continuum of Interventions for Health Care |
|
Tier
|
Source |
Initiator goals/Aims |
Liabilities |
Approaches
|
| 1 |
Website information |
Health information: gain perspective, obtain standard and updated info
Refer patients for somatic symptom disorders |
Quality of information and lack of regulation; less of an issue if referred to site |
Help patients, families, caregivers and colleagues in medicine/surgery |
| 2 |
Support/chat groups |
Patient: education
Caregivers: tips and perspectives on coping |
(Peer compatibility?
Information quality |
May help with adjustment to common medical problems |
| 3 |
Social media (SM) one- or two-way |
Easy and convenient
Likely more convenient for one time use
Good option for patient and clinician prefer |
Not privacy compliant
Busy clinicians may not have time; see if “value added” |
Important to set expectations, limits and boundaries around time and content of matter |
| 4 |
Informal education for self-assessment |
Person/patient: education, tips
Caregiver: education, supports, and advice
Clinician: give assignments |
Not as good as in-person
Use a team and give good sites for quality |
Refer to sites that focus on
longitudinal skill development |
| 5 |
Resources for self-care decision-making |
Person/patient/caregiver: additional options
Clinician: skepticism unless known source; best withinelectronic health record (EHR) |
Good for options, though, what if it depends on…should do A or B? |
Information on topics
Good for team members |
| 6 |
eConsult between primary care provider (PCP) and specialist in EHR |
PCP (pediatrician, family medicine,
obstetrician): timely to visit and sent in time
Specialist: simple questions (e.g., facts, steps to do) can be answered |
May not work for difficult patient cases
These take time to clarify question and review chart |
Monitor timeliness, follow up and quality
Build into care workflow and culture of care |
| 7 |
Assisted self-care assessment and decision-making |
Person/patient/caregiver: empowering as customized and supported
Clinician: effective to distribute skills |
Without help, may make decisions lacking context?
Stay within scope of practice |
Link with social work, hotline and/or clinic, if needed |
| 8 |
Asynchronous, between-session patient-clinician contact (e.g., wearable, app text) |
Person/patient/caregiver has minor question or needs a detail→e-mail/text; tracking symptoms→app
Clinician: e-mail/text for quick, simple advice; apps good for monitoring disorder
|
Align 1-2 apps with 1-2 purposes to focus
Errors, miscommunications
Time, documentation and privacy issues |
Provide training for faculty and team
EHR integrative power
Need evidence-based app and evidence-based approach |
| 9 |
Synchronous,
telepsychiatry (TP) |
Person/patient: it really works and is much more convenient
Clinician: if patients like it, it is a good option |
It always has to be scheduled (and paid for) |
A great option; not always needed due to lesser, easier options |
| 10 |
Hybrid care: in-person and e-option; TP and e-option) |
Person/patient: connect in different ways
Clinician: ad hoc to planned |
Requires discussion, prioritization and feedback
Takes willingness to change, time and $ |
Folks will shift if healthcare financing shifts?
Paradigm shift is needed |
An e-platform may be needed for infrastructure and to efficiently and effectively stage various telecare options. Common technological approaches in medicine include: 1) EHRs, though for users, may interfere with patient engagement and menu-based user interfaces have been cumbersome and unforgiving, but are evolving into more intuitive graphical interfaces30,31; 2) dictation with voice recognition, which still has challenges of integration with legacy, billing and practice management systems—this text system could be replaced by video recordings)32; 3) e-consultation (i.e., e-consult or eConsult) to support a primary care provider (PCP) for decision-making33,34; 4) text-based, chat and social media communication, pose integration challenges and keyboard characters/ emoticons may be used differently across cultures32; and 5) mobile phones, apps and wearable sensors, which are not always evidence-based or integrated into health care systems, but could provide comprehensive self-management approaches and advanced features that leverage the broader functionalities of mobile phones (e.g., sensors, ecological momentary assessments).35,38 By obtaining patient input and preventing/troubleshooting problems, users build trust (i.e., reduce concerns of privacy).26
Many BH professions have put out best practices, guidelines, and position statements for clinicians to adjust to video and asynchronous technologies. Contributions come from: psychiatry/medicine, psychology, social work, counseling, couple/marriage/family, the American Telemedicine Association, the American Psychiatric Association and the Coalition for Technology in Behavioral Science.39 Most guidelines focused on video and sparingly mentioned e-mail, e-consultation, social media or texting,40,41,42 until competencies were published for social media,39,43 mobile health,44,45 and asynchronous care. The overarching goal of competencies is to ensure quality of care for patients, improve clinician skills and promote training.
Business versus medicine/psychiatry leadership: Continuous, committed and active leadership is crucial for strategic planning, management and implementation of change.46 Technology may mean different things to different people, professions and businesses, but it is almost always associated with innovation.47,48 A comprehensive definition of innovation relates to the impact on an organization, based on the magnitude of the advance and the dimension of novelty experienced47
- Incremental: expresses minor changes to current services/product and processes;
- Radical: not frequent in organizations, but requires a major breakthrough or discovery; and
- Transformative: an exceptional shift in processes and beliefs.
John Kotter, Professor of Leadership at Harvard Business School, has contributed two key approaches to leadership for business and health care.49 First, he proposed that leadership is a process that focuses on making organizational changes – the stimuli behind an organization’s adoption of — and adaptation to — improved processes. Management is primarily assigning and tracking tangible outcomes, however, leaders manage and managers lead to some degree. Second, he highlighted eight essential factors for transformation efforts.50 Transformation takes time, so performance improvements must be planned, actively created and achieved, and short-term wins keep participants interested and experiencing some sense of urgency.
In spite of the plethora of possibilities for improved patient care through the use of technology, human factors present the greatest impediment to the implementation of new systems. Success depends upon a blend of both technical and strong organizational skills to plan and manage these changes. Leaders need to strategically plan, understand how innovations diffuse through groups,10 assess the groups’ readiness for change,51 monitor the organizational culture, recognize/plan for resistance to change and communicate effectively. Failure of implementation is usually due to insufficient attention to how change is experienced by the people who do most of the changing.10,52
Effective change leaders:
- Embrace change when needed and take initiative;
- Develop a vision for change and communicate its urgency;
- Communicate with managers and employees, individually and through mass media, with feedback options;
- Stay actively involved; and
- Direct and review change management planning and implementation.
Several approaches, such as those of Deming and Walton53,54 and of Nadler et al,55 describe detailed tactics for working through problems and change in large organizations. Deming, in particular, stressed the importance of including staff at all organizational levels including the lowest tier front-line workers and, notably, customers in “quality circles” as he engineered numerous quality improvements at Toyota. Similarly, behavioral health care institutions need an approach for change management and a technology e-platform to plan, prioritize, and allocate resources for technology (e.g., telepsychiatric video) related to academic goals, education and community partnerships.56 This may include competencies related to patient care, education, faculty development, leadership, finance and partnerships – and it is better to take a broader e-health approach rather than focusing on one technology like telepsychiatry.26
Assessing and enhancing readiness for change: Successful change requires both individuals at all levels and their organizational policies and procedures to change or shift. Complicated processes may seem wonderful to leadership, but can be perceived as burdensome, overly complicated, ineffective, and even counterproductive by those in middle management and those providing services. Unless each level perceives the intended changes to be in their own interests, they may not prioritize or cooperate with implementation, and if objections are not adequately voiced and addressed, those affected may refuse to participate or, in subtler fashion, may engage in passive-aggressive behavior, such as delay, which sabotages the implementation plan.
Assessing how ready to change a group of individuals and organizations may be is complex. Readiness is associated with people’s perceptions of financial support, a well-defined mission, leadership structure, cohesive teamwork, the technical skills needed to adopt an innovation, and the extent to which they see their own needs for safety, security, and autonomy protected. From studies using survey instruments, focus groups, clinical interviews, site visits, and community profiles, it is key to 1) assess, 2) contextualize, and 3) enhance readiness.57 A checklist of factors may help organizations measure readiness for change and develop attitudes and beliefs that provide the context (Table 2). The personal attributes of “change agents,” are important, such as perceived credibility, trustworthiness, sincerity, and expertise. Internal change agents who are mid-range authority figures may assess readiness better than leaders at the top.
| Table 2. Essential Factors for Transformation Efforts in General and Specific to Technology for Healthcare |
| Essential Factors in General |
| 1. Establish a sense of urgency.
2. Form a powerful guiding coalition.
3. Createand communicate a vision.
4. Empower others to act on the vision.
5. Plan and create short-, mid- and long-term goals and successes.
6. Consolidate improvements and produce still more change.
7. Institutionalize new approaches. |
| Essential Factors for Healthcare and Technology |
| 8. Assess the level of innovation required: (i.e., incremental, radical, transformative).
9. Align innovation with organizational culture.
10. Link innovative service process with healthcare outcomes and/or deliverables to end-user(s) (i.e., patient, staff, clinicians; trainees, faculty; interdisciplinary teams).
11. Include clinicians and supporting agencies, patients and regulatory units.
12. Recognize and planning for resistance to change, among other things.
13. Plan an approach to contend with unexpected events.
14. Model and communicate competencies and best practices for change. |
| Problem-Solving Challenges (e.g., Resistance) |
| 15. The statusquo is threatened.
16. Immobilization (i.e., the initial shock reaction to a negatively perceived change).
17. Denial or the hope that the change project is notreal or will go away.
18. Anger or frustration often directed toward others.
19. Bargaining to minimize the impact of change.
20. Depression and other sentiments experienced when bargaining has failed (may represent the beginning of acceptance).
21. Testing, which is similar to bargaining, but more common as persons begin to accept the change and learn how to succeed under the newconditions. |
Implementing innovations often meets resistance to change. Many senior managers forget a critical principle of change management: organizations do not change; people do (Marshall, 1996).58 It is inevitable, particularly if individuals experience a loss of control. An outside organizational consultant who facilitates workers’ grief processes may help.59 Such consultants may provide a safe, non-punitive environment—a transitional space—in which employees may safely explore the implications of the imposed changes. The consultants may explore how anxieties and uncertainty, the introduction of additional complications in the form of new procedures, red tape, regulations, and other factors appear to take precedence over problem-solving, provision of services, and addressing worker concerns.
Predictors of success: leadership and management orientation: Studies have been examining relationships between the managerial-controlled critical success factors, which predict good performance across business, education and health care (largely non-profit) service sectors of the U.S. economy. In 2001, services-producing industries accounted for 81% of the nation’s employment.60 Between 1960 and 2002, employment went from: 0.6 to 2.5 million (M) in education; 0.66 to 9.3 M in business; and 1.5 to 11M in health care61 then 16.4 M in 2010.20 Market orientation (MKT), learning orientation (LRN), entrepreneurial management style (ENT) and organizational flexibility (ORG) are predictors of organizational success (Table 3).
| Table 3. U.S. Service Industry Predictors of Leadership and Organizational Success Across Business, Education and Healthcare |
| Market Orientation (MKT) |
| • Definition: A business philosophy where the focus is on identifying customer needs or wants and meeting them. The three basic tenets are customer orientation, competitive orientation, and inter-functional coordination.
• Keys: The generation of market intelligence, sharing of this knowledge throughout the firm and a marketing response mechanism are important. |
| Learning orientation (LRN) |
| • Definition: Individuals in an organization not only have the ability to do adaptive (incremental) and generative (paradigm shift) learning, but also to keep an open mind regarding different perspectives and continual learning.
• Keys: The norm becomes collaborative learning and is a market orientation is inherently a learning orientation. |
| Entrepreneurial Management Style (ENT) |
| • Definition: An organizational process that encourages and practices innovation, risk-taking, and proactive behavior toward customers, competition and opportunities.
• Keys: The process enables the firm to create value by identifying market opportunities and creating unique combinations of resources to pursue these opportunities. The firm is proactive in obtaining intelligence on customers and competitors, innovative by reconfiguring its resources to formulate a strategic response and implements the response, which usually entails some degree of risk and uncertainty. |
| Organizational Flexibility (ORG) |
| • Definition: the degree in which a business unit is adaptable in administrative relations and the authority vested in situational expertise.
• Keys: It is “organic” in terms of its attributes and structure. |
Market orientation had the highest correlation with performance in all three sectors.62 Generally, the next-highest correlations were with LRN and ENT style rather than ORG. However, in business services, ORG had a higher correlation with performance than either ENT or LRN. There were a number of managerial implications, which not surprisingly, varied by sector. Different industries and markets have different critical success factors and drivers. It is important that executives reflect on these factors, their industry and the market. Health care has done well vis-à-vis both business services and education on MKT, LRN and ENT. This probably reflects challenges faced with managed care/capitation, hyper-competition with mergers/acquisitions and discussions on who is the decision-maker (i.e., now the patient more than ever). Surviving health care organizations have been forced to become marketers and more entrepreneurial with innovation and excellent care.
An Example of Straight Through Processing: How the Banking, Financing and Investing Institutions Have Engaged Customers
Company background/history: Businesses respond to challenges of generating income, meeting consumer expectations and competing with others in a variety of ways. The Company offers life insurance products, such as term, whole, universal and variable universal life insurances, fixed and variable annuities, disability income insurance products, retirement plans and business solutions (e.g., fringe benefits and retirement plans). In addition, it also offers investments which include mutual funds, variable annuities, direct participation programs, full-service stock and bond trading products, group retirement plans, college savings plans, health savings accounts and cash management accounts. The company has strategically grown as a leader within the insurance industry for providing quality, low cost products and achieving superior financial growth. Its shares of stock are 100% owned by the Company’s Mutual Holding, Inc., whose voting members are life insurance policyholders and annuity contract owners. In 2018, it accomplished its 29th consecutive year of growth of individual life insurance sales, a record unmatched in the industry, with a 20% increase from 2015 and $XX billion (B) of assets under management.
Challenges for the company and other banking, financing and investing institutions include generating income, meeting consumer expectations and competing with others. Manual data may have some pearls, but they are hard to access quickly and require reconciliation. This delays decisions, costs time to reconcile and leads to dissatisfaction.63 In the trade life cycle — from initiation to settlement — trades by phone or via a trading desk had to be keyed into PDF trade tickets, entered into the investment accounting system in order to process the trade and security information for reporting purposes and general ledger notation. The trade is then faxed to the custodian for settlement purposes and all communication with brokers is done via phone and email. Companies had tended to leave out IT, in general, or to barely include it in order to capture parts of the data flow64,65:
Two issues have encouraged the Company to change. First, insurers — like all other businesses — have to determine how to utilize technology strategically to best manage current and new challenges related to core processes and growth of market share.66 Insurers have had more downgrades per Fitch Ratings, Standard & Poor’s and A.M. Best than other businesses, suggesting that the “back office” had to be modernized.67 Second, global financial services had skyrocketed from 13 M ($382 B) in 1980 to 221M ($11.1 trillion (T) in 2000.63 The Security and Exchange Commission (SEC) facilitated STP use for cross-border trading by setting standards T+1 (trade day + 1 day instead of T+3). This required millions of transactions — and the participants — to interface and use a system that did not crash.63,68
The company considered a solution for analysis, time/resources and planning.
Straight through processing (STP) is defined as end-to-end automation of security trading from order to settlement. Information that has been electronically entered by one party may to be transferred from another party instead of manually re-entering the same pieces of information repeatedly over the entire sequence of events (Figure 1). This reduces the time it takes to process a transaction and increases the likelihood that a contract or an agreement is settled on time and without error. This works using automatic linkages across geography with a paperless sequence of events. STP helps all parties, including asset managers, brokers, dealers, custodians, banks and other financial services players.
Figure 1. Steps of Trading Processes and Participating Parties Under the Sraight Through Processing Umbrella
| STEPS |
Securities Information Management |
Pre-trade
Preparation |
Trade
Execution |
Post-trade
Pre-settlement |
Pre-settlement |
Settlement Transaction |
Post-
settlement |
Securities
Administration |
| PARTIES |
Asset/Fund Manager
Research Institutions
Information Services Providers
Global/Local Custodians
Listed Institutions |
Asset/Fund Manager
Broker/Dealers
Market Makers |
Asset/Fund Manager
Broker/Dealers
Market Makers |
Asset/Fund Manager
Broker/Dealers
Exchanges/Markets |
Asset/Fund Manager
Broker/Dealers
Global Custodians |
Asset/Fund Manager
Broker/Dealers
Global/Local Custod-ians |
Agent and Clearing Banks
Securities Depositor-ies |
Agent and Clearing Banks
Securities Depositories
Global/Local Custodians |
| PROCESSES/ DOMAINS |
Investment Management |
|
|
|
Insurance/Asset Management |
|
|
|
Capital Market |
|
|
|
Retail and Wholesale Banking |
|
| Adapted from Idea Group, Incorporated, 2003. |
There are levels of STP: 1) intra-STP, within an organization and its branches; 2) extra-STP, between firms with direct access into other companies’ internal processes across an industry; and 3) global-STP, across worldwide or global boundaries. Challenges are/have been: 1) data capture; 2) internal workflow; 3) external workflow; 4) real time processing; 5) front, middle and back end office connectivity; 6) adoption of industry standards and protocols; 7) multilateral interfaces with third parties; 8) just-in-time enrichment; and 9) global implementation.
Field study notes: Questions asked of Company leaders and application to psychiatry/behavioral health and health care (progression from current state to IT integration).
- How would you describe the current IT/systems structure within the back office and the front office areas within your Company?
It has the functional capacity for status quo operations, but with significant opportunity for improvement. We are attempting to move away from a situation where we are playing catch-up to one more adaptable to future changes. These things take time and resources. There are an incredible number of obstacles all companies face to accomplish this. Too many of our manual and IT processes are exceptions instead of the rule. This not only creates inefficiencies, but it reduces adaptability and increases risk, especially in the areas of potential sharing of knowledge by personnel.
Application to psychiatry: mental health clinical care. In an outpatient department, there are many gaps between the back office and front office (i.e., patient side). Clinical care involves insurance (i.e., benefits), scheduling, billing, collections and communication (e.g., records to primary care) – rarely are all parties on the same page (e.g., insurer and clinic administration may only know benefits and patients and clinicians have to double check). For clinical care workflow, information systems and domains include the EHR, picture archiving and communication systems (PACS), laboratory information systems and CDS systems. Some health care systems have CDS to provide clinicians, patients and others with knowledge and person-specific information, intelligently filtered or presented at appropriate times, to enhance health and health care.7,69 Similar to STP for investments, CDS improves patient outcomes, reduces unnecessary mistakes and expenses and increases efficiency.70
- Would you say that most of your IT projects currently within the back-office and front office within the investment department are short-term (i.e., 6-months) or long-term? What has caused this?
We have been focused on shorter-term solutions more recently given the lack of appetite for longer-term projects, which tend to be on the pricier side in both terms of dollars and people. We have been trying to show a clear cost/benefit solution to the projects we are pursuing. Most critically we are getting creative with how to solve problems. For example, I might not be able to sell a project on implementing a new data warehouse. But I might be able to sell someone building the database structure for me. We attempt to budget for the actual IT, marketing/messaging and training short-term costs –if we do that well, we believe we get lower direct and indirect costs later. Then, over 1-6-months, We borrow help from existing or others’ staff to load data into the data warehouse in an automated fashion via extract, transform and load (ETL) or scheduled jobs, and I can build the reporting systems myself. These pieces make it easier to get enhanced, dedicated resources for the whole process via permanent funding.
Application to psychiatry: Mental health research and clinical care. With research there is a need to link participant expectations with procedures and completion of a study. The time, resources and infrastructure is organized with a grant, though short-term rather than long-term; some are pilots to collect data for more substantial grants for long-term projects. Clinical services and insurance are usually focused short-term (e.g., 2-4-months for therapy) or mid-term if not intensive (e.g., medication visits); few have extensive long-term insurance for clinical care. The best that can be hoped for is cost-offset, with IS and IT investments for a health care system adding to workflow, information used by multiple parties in-time across departments, and rarely, in a community.
- How are insurance companies managing the complex challenges of integrating back-office processes with front-office solutions (i.e., what is your Company’s approach)?
Companies have to create accountability for results and this means that people have to be empowered with the correct tools and resources (i.e., more than dollars and staff). The correct ethos of an organization is the biggest benefit, which for us is about customer service, accurate data, precise operations, teamwork and more transparency; we move away from silos of responsibility and disconnects between staff and customers. Business processes are becoming more complicated all the time, across multiple departments, computer software and companies. We often rely on project managers who are only concerned about their “project silo” rather than integrating multiple projects, departments, and systems together in a cohesive process (i.e., true accountability). IT additions over the years have not helped; we needed systems that enhanced data flow, integration, access and communication. Now, there are project prioritization meetings across groups (IT, marketing and production) — in-person and virtual — and we have a committed effort to break knowledge silos/barriers. Coronavirus disease 2019 (COVID-19) has boosted our virtual culture quite a bit.
Application to psychiatry: Administration: We have too few staff and many managers to keep up with university/hospital, accreditation and regular administrative tasks. We do not have time, resources and infrastructure to get organized and we have to focus on the short-term rather than the long-term — there is never enough time? Assertive health care systems forge through these challenges with incremental IT — often because “patients deserve the best.” However, expenditures are limited by budgets and systems usually do not face extinction and there are not millions or billions of dollars to make it worth their while. Some systems will invest, though, as IT can link clinical, administrative, quality improvement and external accreditation processes, making it is easier to queue participants for completing tasks, monitoring outcomes and documenting standards are met.
Summary
The company decided to prioritize the following:
- Reach higher volume activity (various instruments other than the routine fixed income and futures),
- Acquire more drill-down data and complex analytics demanded by strategic business units (SBUs),
- More quickly obtain financial information for financial control, and
- Require portfolio managers to be trained for more in-depth risk analysis and portfolio analytics.
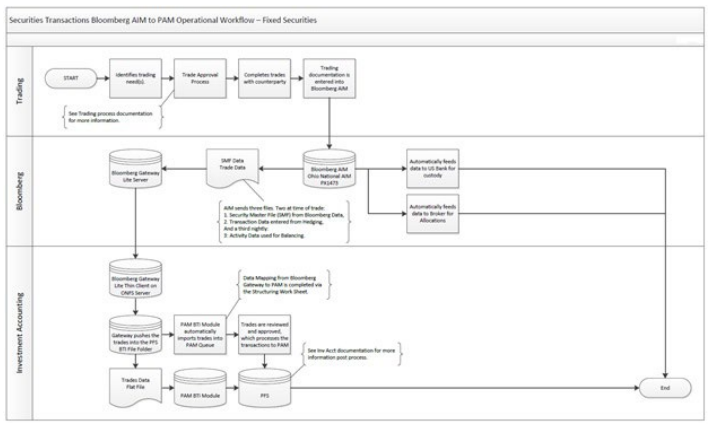
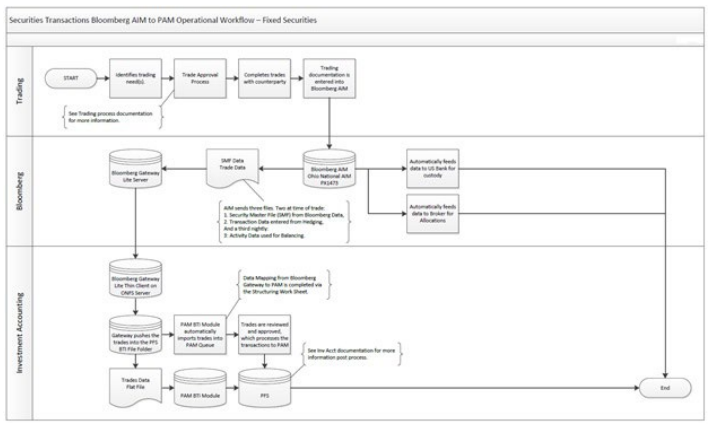
While STP initially was seen as the way to get a trade “locked in,”71 perspective shifted from settling the trade to multilateral payment and netting64 – a significant reshaping of the Company’s entire process from before and after STP (Figures 2 and 3). Overall, STP has reduced trade life time cycle — with the potential to reduce systemic and operational risk — while increasing speed and reducing cost. STP provides a competitive advantage for a company with a good business understanding-IT relationship.
Challenges and Reasons for Health Care (e.g., Medicine/
Psychiatry) to Implement a Shared IT-Business Understanding
AHCs are the standard in the health care system for tertiary and quartinery care, training/education/professional development and research. AHCs also have important partnerships with other organizations, provide jobs for the economy and serve communities in many other ways. They have survived through vigorous cost-cutting efforts, but AHCs must change dramatically to meet the changing needs of patients and society.72 First, there is the need for better balance between specialization, ambulatory/primary care and cost-effective services. Second, they face aging of the population, a dramatic rise of chronic disease, an influx of patients from different cultures, decreasing financing streams and marketplace dynamics. Third, they have to contend with technology implantation and change.
Institutional movement toward telemedicine and telepsychiatry – whose modern era probably started around 20-years-ago – has been slow with some exceptions (e.g., research, private companies, Veterans Affairs).40 Telepsychiatry video aligns with conventional care compared to other technologies used by patients, clinicians and others. Along with the EHR, it had been a specific indicator for institutional e-readiness (or not) until the COVID-19 era; the degree of telepsychiatric integration into workflow – if measured and measurable – will be an indicator of systems’ progress (or not) in the near future. AHCs have implemented EHRs, some decision support and a few other technologies (e.g., robotics, mobile health). Institutions with e-service lines (Veterans Affairs), training guidelines (e.g., Department of Defense) and technology-specific competencies (e.g., video, mobile health) indicate progress and readiness for technological integration; most IT and IS interventions are more hospital centered and in medicine (e.g., intensive care) rather than behavioral health.
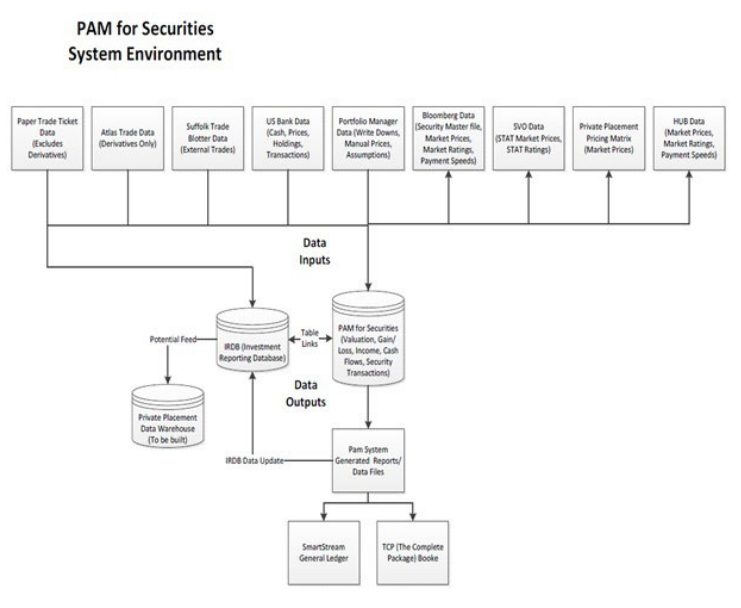
Figure 2. Processing Transactions Before STP In PAM (An Investment Accounting System) for Securities System
Environment Manual Process
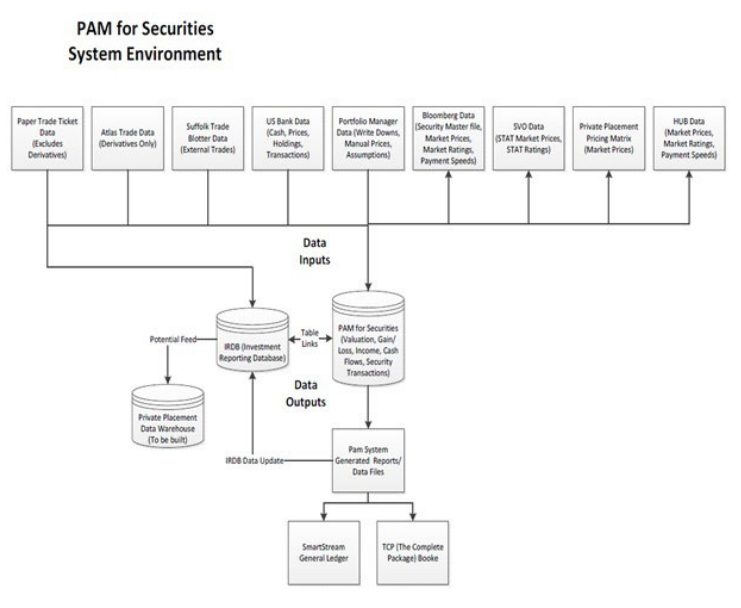
Figure 3. Processing Security Transactions after STP with Bloomberg AIM to PAM (An Investment Accounting System) Operational Workflow for Fixed Securities
The shared IT-business understanding: A Shared IT-Business Understanding is defined as shared domain knowledge and common understanding between the IT and research and development, marketing, production and financing functions.12 Specifically, a shared IT-Business Understanding is: 1) the knowledge that IT managers possess about a specific process; 2) the knowledge the line managers possess about potential opportunities to apply IT to improve the process; and 3) the common understanding between IT and line managers regarding how IT can be used to improve process performance. Problems have been associated with adding on IT for one function, short-term rather than long-term planning, manual processes and problems evaluating entire workflow systems.73,74
Empirical studies show successful implementation of IT requires integration with other core business functions and it leads to improved organizational performance.12 IT helps leaders negotiate change and position for the next growth cycle, in terms of distribution, management, scale and capital issues.75 This reflects the IT-business strategic alignment can support, organize and drive business processes. IT integration in this sense, then, is an indicator of the maturity of an organization. Investments in IT via STP have surged and the payoffs are significant – if done with a specific goal in mind and with purpose.76,78
The Ross competencies/stages: Perhaps the best step toward a shared IT-business understanding is to create a strategic IT architecture with outcomes tiered in four levels.79 In fact, the terms architecture and infrastructure are sometimes used interchangeably, with architecture seen as the plan for the next infrastructure. More often, IT architecture refers to a firm’s list of technology standards. But viewing IT architecture only as technology standards does not connect it to business requirements. An enterprise IT architecture concept, though, does place technology standards in the context of business requirements.
To develop a synergy between business strategy and IT architecture, firms must develop organizational competencies in IT architecture.79 An IT architecture competency is the ability of a firm to create a mutually reinforcing pattern of evolving, tightly aligned business strategy and IT capabilities. The logical sequence for developing an enterprise IT architecture is based on defining: 1) the firm’s strategic objectives; 2) key IT capabilities for enabling those objectives; and 3) the policies and technical choices for developing the IT capabilities. This specifically includes a company’s need (e.g., doing a needs assessment) and assessing how IT is used (i.e., levels extend from silo to standardized to rationalized data to modular architecture)79 (Table 4). Steps include defining a set of critical IT capabilities with lasting value, tradeoffs due to policies and technical choices and incremental progress.
| Table 4. ROSS’ Four Informational Technology (IT) Architectural Stages: Qualities and PROS/CONS for Businesses and Applied to Academic Health Centers |
|
Architect-Ure Stage
|
Definition/Example |
Assumptions |
PROS |
CONS
|
| Application Silo |
Individual applications rather than for the entireenterprise
High technology companies
Individual clinician |
Best available technology
Single geography
Needs-based
Technology-based change
management |
Facilitates innovation
Well-received by most
Predictable system benefits and outcomes measurable
Data: centered in the application |
Difficulty linking new applications to related systems
Applications become a burden
Expensive to maintain |
| Standardized Technology |
Enterprise-wide and provides
efficiencies through
standardization and, usually centralized
UPS
Clinic system approach |
Technology standards to limit technology choice and reduce the number of platforms
Solutions-based
Standardization and exception management |
Good for local knowledge and worker support
Better IT maintainability,
reliability and security
Data: create warehouses to share
Cost savings |
Data still in individual applications; silos
Manager resistance to standards
Figure out exceptions
Long-term planning key |
| Rationalized Data |
Enterprise-wide IT architecture expands to include standardization of data andprocesses
Air Products, Nestle USA, Delta Airlines
Healthcare system |
Data management and infrastructure; core wiring
Performance- and integration-basedmanagement |
Stabilizes the firm’s core
activities and increases
predictability ofoutcomes
Data integrity
Process standardization
Stability
Business not IT owns data |
Difficulty deciding “core” processes (excluding others)
Change harder and incremental (to reach)
Implementation risk: accountability, discipline |
| Modular |
Enterprise-wide standards with looselycoupledapplications
andtechnologyforlocaldifferences
Citibank Asia Pacific
AHC with departments or special programs |
Enables strategic agility through customized or reusable modules
Extend the core processes but allow for differences |
Business units select
customer-oriented processes from a menu
Greater discretion
Efficiency (e.g., quickly
implements core products in new countries) |
Ongoing dialog between
management and IT executives: clarify required/selective and one/more processes for choice |
In the case example, the Company realized that they needed to look more closely at developing a shared IT-business understanding, and that specifically, that they were missing the opportunity to capture more/better data and moving too slowly through manual processes. They also realized that this type of IT intervention was not just a “good idea” or innovation, but that they may be falling behind competitors – at a competitive disadvantage.
Will AHCs, health care systems adopt a shared IT-business understanding model?
Key steps suggested for institutions to integrate video apply to other technologies: 1) assess readiness; 2) create/hardwire the culture; 3) write policies and procedures; 4) establish the curriculum and competencies; 5) train learners and faculty; and 6) evaluate/manage change.56 Institutional level competencies – aside from technology competencies for clinicians – involve steps for video and asynchronous competencies organized into focus areas: Patient-Centered Care; Evaluation and Outcomes; Roles/Needs of Participants (e.g., Trainees, Faculty, Teams, Professions); Teams, Professions and Systems Within Institutions; and the Academic Health Center Institutional Structure, Process and Administration (Table 5).
| Table 5. Competencies for Institutions/Academic Health Centers for Synchronous and Asynchronous Telehealth |
| Competency Focus |
General Technology Approach |
Shift to Include Synchronous Care |
Shift to Include Asynchronous Care
|
| Patient-centered Care |
Offer multiple points-of-entry
Employ interprofessional teams and care
coordination
Data warehouse, analysis and health information exchange
Screen for technology use |
Educate on in-person and synchronous similarities
Use as one of many care models/treatment options
Use templates and adjust policies and procedures |
Offer selected options (e.g., apps, sensors/
wearables)
Design clinical technology workflows
Import social science, health behavior and business ideas |
| Evaluation and
Outcomes |
Assess readiness for change
Link behavior to outcomes for a patient or program
Use evidence-based measures
Use accreditation principles: Goal, Measure, Benchmark, Target and Data |
Build video scheduled and on demand options
Use disease state measures and adapt, if applicable, aligned with in-person
accreditation
Use 360 evaluation |
Organize care on a technology platform (e.g., EHR, pre- and post loads)
Use technology-specific measures, evidence-based if available
Use 360 evaluation |
| Trainee/Student Needs/Roles |
Patient- and learner-centered outcomes
Prepare as Resource Manager
Clarify personal versus professional technology use
Use technology as a lifelong learner/teacher |
Integrate skill development, care, teaching, supervision
Monitor well-being and professionalism
Adjust curricula (e.g., part-time rotations, supervision)
Employ quality measures |
Use quantitative and qualitative approaches
Use observation, video and simulation
Role model healthy behaviors
Capitalize on personal expertise to spur others’ use |
| Faculty Clinical,
Teaching and
Leadership Roles |
Emphasize communication, well-being and professionalism
Emphasize resource manager technology
leadership role
Use social science, health service and business constructs to shift attitudes |
Monitor technology impact on care,
well-being/fatigue
Integrate part-time use for care, with teaching by champions
Define success based on teams, systems and populations |
Use sustainable, longitudinal approaches
Remember that “less is more” and evidence base is key
Use technology for portfolio, curricula,
dissemination, networking and other purposes |
| Teams, Professions and Systems Within Institutions |
Assess structure/function of social groups that govern behavior of a community
Use faculty development with teams, projects and professions to build skills and shift culture |
Foster alignment across systems
Organize goals and outcomes for success based on teams, systems and professions
Employ team-based care and virtual teams |
Align shared outcomes
Patient/clinician outcomes
Learner/teacher
Clinic/system
Institution/community
Use stepped care and interprofessional principles |
| AHC Organizational Structure, Process and Finance |
Evaluate/manage governance structure and change
Weigh human resources,
Technology and cost issues
Market technology delivery of care competitively
Build AHC-community partnerships to share resources and integrate care
Align clinical, educational and research missions and values Integrate (not add or append) information technology into organizational structure |
Use faculty development projects for
existing/new leaders, as a gateway to
others (e.g., mobile health)
Measure technology in performance
evaluations and provide feedback
Add research and funding infrastructure for pilot and full-scale projects, to impact health service delivery and training programs |
Assess context, pace, scope and drive of/for change
Monitor private, federal, state and other sectors for best practices, partner agencies and grant funding
Strive for incremental, sustainable solutions
Use/adapt others’ evidence-based system
approaches
Develop strategies for promoting adoption/
optimization of clinical information systems |
There are usually competing priorities in companies akin to AHCs’ clinical care, education, research and other missions. In addition, AHCs contend with policy, accreditation, reimbursement and other administrative tasks. Regulatory standards often determine how quickly policy decisions are reached and consequently result in huge differences in current state of the technology development and adoption around the globe. The significant disadvantage that an AHC or a department has, is that its existence does not depend on a shared IT-business understanding unless an AHC’s does, since millions or billions of dollars are not immediately at stake to remain viable. Traditional AHCs are not competitive with clinical models of other more modern health care systems (e.g., Kaiser, Veterans Affairs), so new AHC models by the Mayo and Cleveland Clinics are moving forward.
If an AHC decides to transform its strategic planning with technology, then institutional competencies would include a better e-platform for integrated clinical and administrative workflow, as well as a vision for short- and long-term planning. A change management plan with process management26 could help to plan, prioritize and allocate resources. Buy-in across all levels is essential,50,51 as stakeholders have to believe that technology significantly contributes to improving the mission. Then, training, supervision and evaluation is needed for managing, adjusting competencies/skills and quality/performance improvement. The deployment, innovation and integration – not the cost or elegance – enables companies to standardize and reduce costs and risks. eHealth integration and interoperability solutions use an enterprise architecture.80 When implementation climate is strong, consistency of technology use is high. However, quality of technology use was high only when implementation climate was strong and values compatibility is high.81
DISCUSSION
Technology is rapidly shifting what we do and how we do it in day-to-day life, education, social relationships, health care and business. Our view of technology, like our view of medicine, will change over time based on social, political and scientific roots. Much of this is evident in the evolution of telephone, the stethoscope and now telehealth and telepsychiatry; human factors have always played a role.82 Similarly, how medicine has been conceptualized has changed over many eras from descriptions a social science, a germ theory of disease, and a battleground to a management enterprise, as well as a way to meet rights/needs (i.e., the social justice model) and an evidence-based practice (i.e., public or population health).83 Business may serve as a role model for medicine/psychiatry to use technology to streamline health care across individual, community and societal domains. Models like the Learning-Adapting-Leveling (LAL) shoot for translation of technology from market to implementation into health care systems moving towards personalized health care.84
Technology via mobile health could reshape health care service delivery if is integrated into services, used wisely and limitations are addressed.85 A review of cognition and mobile health has raised concerns about attention, memory, and delay of gratification – and undercut colloquial assumptions that we can cognitively multi-task.86,87 Current research on mobile health does not often employ true experimental methods with random assignment, longitudinal evaluation, momentary in-time integration of data, diverse populations and objective measures.86,88 A further shift is research and evaluation based on effectiveness, implementation science and models of assessment of technology.89,90,91,92 User-friendly approaches and frameworks for evaluating multi-stakeholder perspectives predict success (e.g., co-construction between designers and users).93,94 One example would be applying the Effective Technology Use Model to implementation of e-consult management software.95 Another option is to upgrade the Integrated Technology Implementation Model (TIM) for integrating technology into health care practice by adding a conceptual guide for nursing leadership, vendors, and engineers based on focus group methodology (i.e., Integrated TIM (ITIM)).96
A shift in research paradigms is also suggested at a system level.97 The Technology Acceptance Model (TAM) and Unified Theory of Acceptance and Use of Technology (UTAUT) have been used widely in studies of health information technology implementation. TAM is determined by attitude toward using the technology, which in turn is determined by two perceptions of usefulness and ease of use. Various external factors affect both perceptions. UTAUT’s four constructs that affect usage intention are performance expectancy, effort expectancy, social influence and facilitating conditions. Age, gender, experience, and voluntariness of use mediate the impact of these expectancies on intention98 and poor perceptions about the technology’s usefulness and lack of trust employers’ use of tracking data were associated with weaker intentions.99 In addition, these tend to focus on individual adopters’ beliefs, perceptions and intention rather than tackling complexity with a broad enough perspective for all levels of an institution – or preferably across populations.
Multi-dimensional approaches can better capture the complexity of issues surrounding implementation and use of HIT. Models for good governance of health care technology management in the public sector globally, based on evidence-informed policy development and implementation are also suggested.100 Furthermore, health technology reassessment is suggested via structured, evidence-based assessment of the clinical, social, ethical and economic effects to inform optimal use and quality of technology in comparison with its alternatives by health care providers, managers and policy-makers.101 Suggested phases are: 1) selection (identification and prioritization), 2) decision (evidence synthesis, policy development); and 3) policy implementation, evaluation. Some countries have an advantage in establishing consortia to create an alliance of universities, university hospitals, research institutions and IT companies, which establish Data Integration Centers (DICs) at each partner hospital and to implement use cases which demonstrate the usefulness of the approach.102
AHC and psychiatric leaders have slowly explored/added telepsychiatric services – but few have an approach to technology, in general, due to competing clinical, educational and research demands. On one hand, radical and/or transformative change is not easy for AHCs, but on the other hand, incremental approaches are resulting in health care and psychiatry/behavioral health being passed by other components of our culture. The model of a shared IT-business-medicine103 or IT-business-health understanding104 – as part of strategic planning – could improve performance via efficiency, quality of data/information processing/integration and managerial teamwork. For it to work, though, clinicians, managers and administrators need to shift their philosophy—from seeing what happens—to proactively designing the services in advance to achieve outcomes. Needs and impact assessment for participants across all levels of the organization, continuous quality/performance and short- and long-term planning are required. For example, it is important to assess attitudes and behavior of health care workers before, during, and after implementation of real-time location system technology.99
There are limitations to this work and many future directions are suggested. The first limitation is that this is not a formal systematic review, as this explored the literature to find key concepts, which will serve as the foundation for more specific future research. Second, other models of assessing, implementing and integrating technology exist. The shared IT-business understanding, though, is conceptually simple. If it is coupled with institutional competencies for technology and an architectural process with competency stages, institutions may self-assess and explore the next step. Third, STP is only one of many potential examples of system integration, but it is representative of business culture. Fourth, a more formal process of expert consensus could be helpful for this type of review. Finally, more research is needed on the assessment of companies’ models, objectives, methods and outcomes. The pilot application of this model and similar frameworks to medicine/psychiatry would also be helpful. Within such research, quantitative and qualitative methods would be imperative. Effectiveness rather than efficacy evaluation would also be suggested.
CONCLUSION
The field of business has some similarities with health care related to implementation of technology. Continuous, committed and active leadership is crucial for strategic planning, management and implementation of change. Leadership skill and orientation toward market, learning, entrepreneurial management style (ENT) and organizational flexibility are predictors of organizational success When IT is integrated into health care service delivery workflow rather than appended, it facilitates the translation of strategic planning into organizational change. Successful implementation requires a needs and impact assessment for patients, staff, clinicians and leaders across all levels of the organization. Incremental and strategically innovative approaches need to be evaluated and quality improved. Benefits to the mission, limited disruptions of core operational workflow and reasonable costs reduce the likelihood of failure.
ETHICAL CONSIDERATIONS
IRB approval was not necessary due to this being a review of
literature.
FUNDING SOURCES
No funding sources were required for this literature review.
ACKNOWLEDGEMENTS
VA Northern California Health care System.University of Cincinnati Lindner College of Business. University of California, Davis School of Medicine and Department of Psychiatry & Behavioral Sciences.
DISCLOSURE
On behalf of all authors, the corresponding author states that there are no financial or personal conflicts of interest. The authors participate in national organizations, but do not have leadership positions, nor would that participation impact competencies, as far as can be ascertained. The authors alone are responsible for the content and writing of the paper.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest