INTRODUCTION
A hematoma known as spontaneous retroperitoneal haemorrhage (SRH) is unrelated to invasive procedures, surgery, trauma, or abdominal aortic aneurysm.1 It is a rare complication in people receiving hemodialysis, anticoagulant medications, or who have bleeding disorders. It is one of the most serious and potentially fatal side effects of anticoagulant medication.2 It has been calculated that the risk of bleeding with unfractionated heparin therapy is two to five times higher than that with Warfarin.3
CASE REPORT
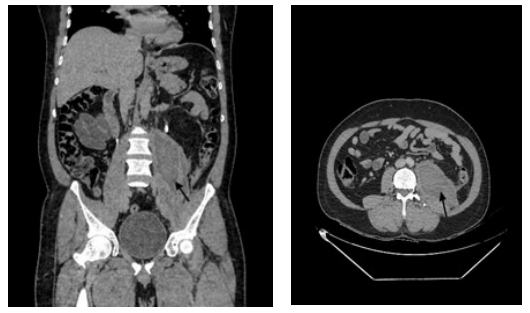
A 57-year-old-man arrived at the emergency room (ER) complaining of a fever, dark-colored faeces, generalized tiredness, and profuse sweating for the prior three-days. The patient previously complained of a stomachache on the left side that would get worse while leaning over or coughing and go away with rest. There was no other notable history. He was currently taking oral anticoagulants in addition to having previously undergone surgery to replace his mitral valve. The patient has no history of recent trauma. international normalizedratio (INR) 2.01 was the most recent value, which was within advised range. Both the heart rate and blood pressure remained stable at 108 beats per minute and 130/90 mm Hg, respectively. When examined clinically, the patient displayed pallor. A systemic examination identified discomfort in the left lumbar and hypochondrium areas. A click was heard in the mitral region during a cardiovascular (CVS) check. Other systemic analyses were not really noteworthy. Routine tests and an abdominal ultrasonography (USG) indicated anaemia and a mildly dilated small bowel loop measuring 7.3 cm. A significant heterodyne retroperitoneal lesion with surrounding fat stranding and fluid was visible on the abdomen on computed tomography (CT) Figure 1.
Figure 1. Contrast-enhanced CT showing Hematoma Involving the Left Iliopsoas Compartment with
Surrounding Fat Stranding and Free Fluid in Posterior Pararenal Space
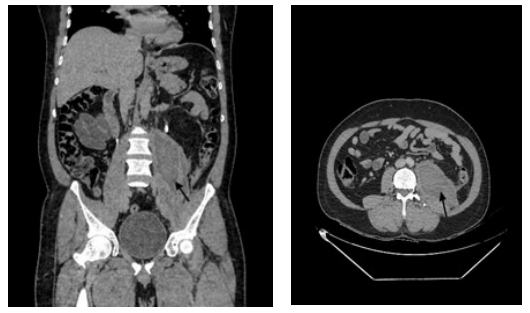
On the left psoas muscle, further CT contrast revealed a positive haematocrit sign. Hetero-dense lesion with fluid tracking along the left lateral conal fascia and left paracolic gutter, measuring 6.8×7×18.4 cm. Pigtail catheterization was used to manage the patient, and new frozen plasma and a blood transfusion were administered. Repeat CTs were performed on successive days, and they showed a shrinking hematoma. The patient was discharged because his symptoms had improved. Despite its ambiguous presentation, it is essential to get a diagnosis right away in order to reverse the anticoagulation and stop future bleeding.
DISCUSSION
According to reports, between 0.6 to 6.6% of patients receiving therapeutic anticoagulation develop retroperitoneal hematomas. 4,5,6 Heparin with low molecular weight, unfractionated heparin, and warfarin have all been linked. For heart issues or venous thromboembolism (including deep vein thrombosis and pulmonary embolism), the majority of patients receive anticoagulant treatment (prosthetic valves and atrial fibrillation (AF). Anticoagulant-taking individuals are at risk for substantial bleeding if they have anaemia, severe renal disease, are under 75-years-old, have experienced previous bleeding, or have high blood pressure. Patients with endstage renal disease (ESRD) are more likely to experience hemorrhagic consequences,7 mostly because of platelet dysfunction, anaemia, and low levels of vitamin K. Patients using warfarin have a higher risk of major bleeding if their INR is below 3, especially the elderly.8 A multispecialty approach is necessary to manage warfarin-related bleeding because it depends on a number of factors, including the patient’s hemodynamic instability, the significance of the bleeding, the supratherapeutic INR value, and the potential for a thrombotic event after reversing anticoagulation. Patients report experiencing hip or lower abdomen pain that radiates to their groin or anterior thigh compartment. Bleeding into the psoas muscle causes spasticity and hip flexion, and as it worsens, bruising on the side or thigh may appear. Reduced quadriceps strength, lack of knee jerk, and paraesthesia in the region of cutaneous supply are all effects of femoral nerve compression. The preferred investigation is a CT scan,9 but ultrasonography is a quicker diagnostic technique. Delay in diagnosis may be fatal since major haemorrhage may follow. A localised ureteric blockage from the hematoma may result in acute renal failure or femoral nerve compression.10 Other than stopping anticoagulants and giving vitamin K to individuals with life-threatening bleeding, quick reversal medications such prothrombin complex concentrates (PCCs) or fresh frozen plasma (FFP) should be given.11
CONCLUSION
Patients who appear with abdominal pain, hypotension, and low haemoglobin levels while on anticoagulant therapy should be evaluated for spontaneous retroperitoneal haemorrhage as a differential diagnosis. Despite the hazy appearance, early diagnosis is essential for the right course of action and to stop the condition from getting worse. Anticoagulant-induced bleeding should only be managed carefully.
CONSENT
The authors certify that appropriate patient consent was obtained.
CONFLICT OF INTEREST
No potential conflict of interest related to this article was reported.