Cervical spine synovial cysts are rare.1 Because they can be asymptomatic, the exact incidence is unknown. For example, they have been shown to become symptomatic with neurologic deficit only after an acute flexion-extension injury.2A retrospective report of patients at the Mayo clinic from 1984-1997 included nine with synovial cysts at C7-T1.3 A recent study of seventeen cases of cervical synovial cysts at Johns Hopkins from 1991-2013 included ten cysts at C7-T1.4 A meta-analysis published in conjuction with that report accounted for 23 additional cysts at C7-T1 for a total of thirty-three cases.
As in the lumbar spine, synovial cysts are associated with spinal segments that have increased mobility3 and there has been documented evidence of related instability within the cervical spine as well, anywhere from the atlantoaxial junction4 to C7/T1.5 Generally accepted treatment for symptomatic synovial cysts is a posterior approach with laminectomy, hemilaminectomy, laminotomy, or foraminotomy, as the case requires to access and resect the cyst. In the case of symptomatic cysts without indication of instability, the debate is whether a fusion is required to prevent subsequent instability and symptomatology.
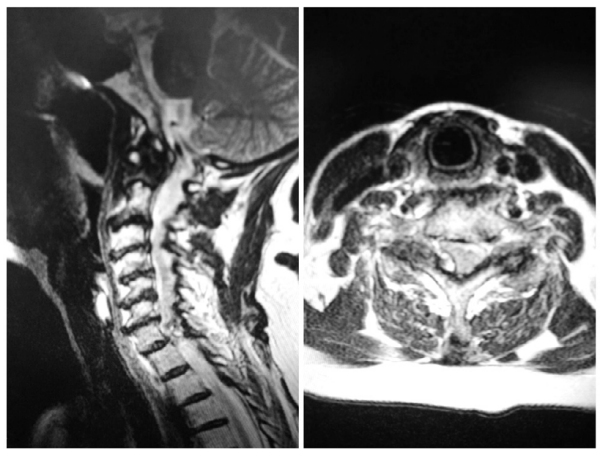
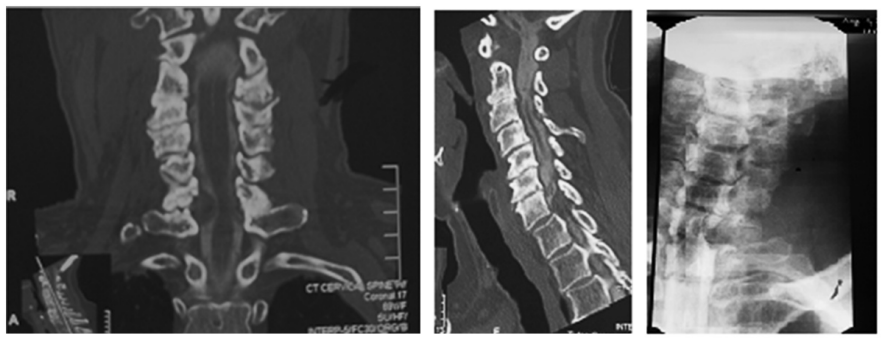
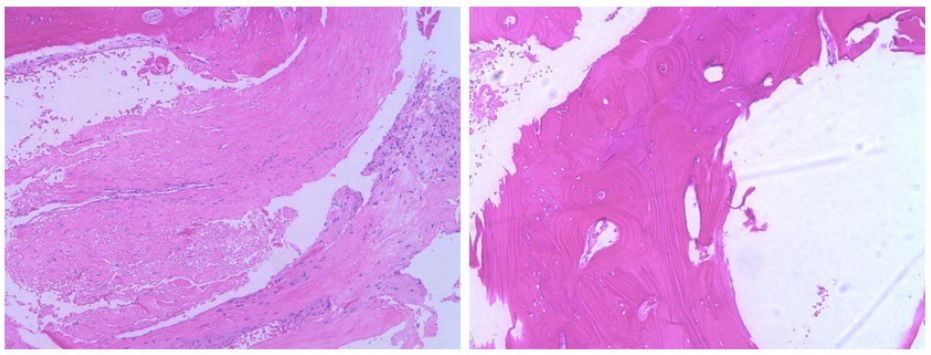
The authors think this is a unique case because in the literature this patient unlike other reported cases had diffuse cervical pathology on MRI (Figure 1) and the final diagnosis required confirmation with Myelo/CT (Figure 2) and EMG in the face of diffuse degenerative cervical disc and spondylolisthesis. In fact, the exam and EMG were instrumental in establishing the diagnosis of a C8 radiculopathy and allowed the authors to perform a more minimally invasive approach, restricted to C7-T1. In addition, this paper has pathologic confirmation of a synovial cyst as the diagnosis (Figure 3).
Figure 1: Sagittal and axial T2 MRI.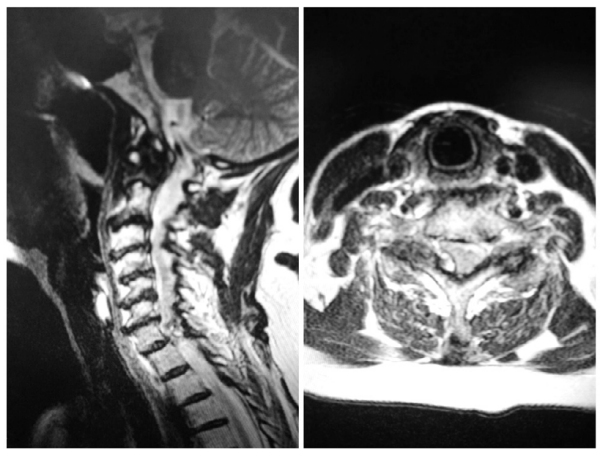
Figure 2: Myelogram and post-myelogram CT
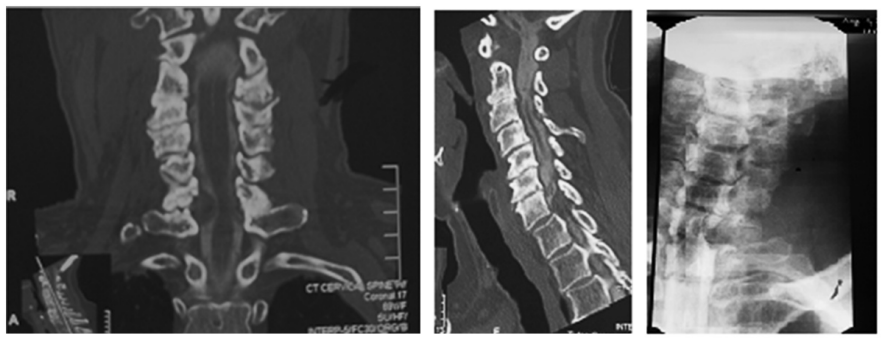
Figure 3: Pathology confirmed the diagnosis of synovial cyst.
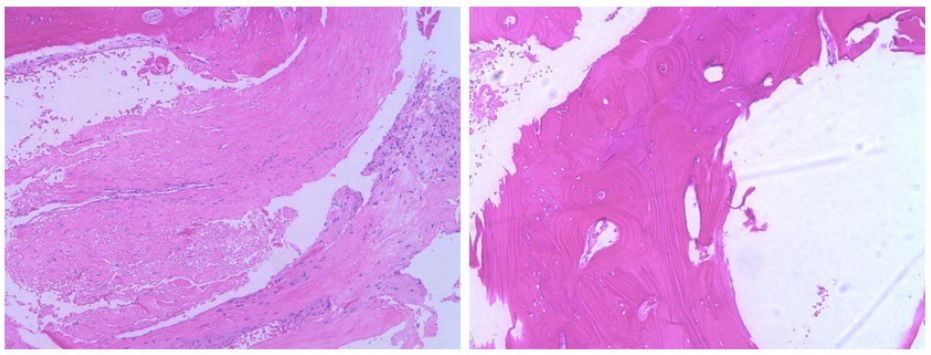
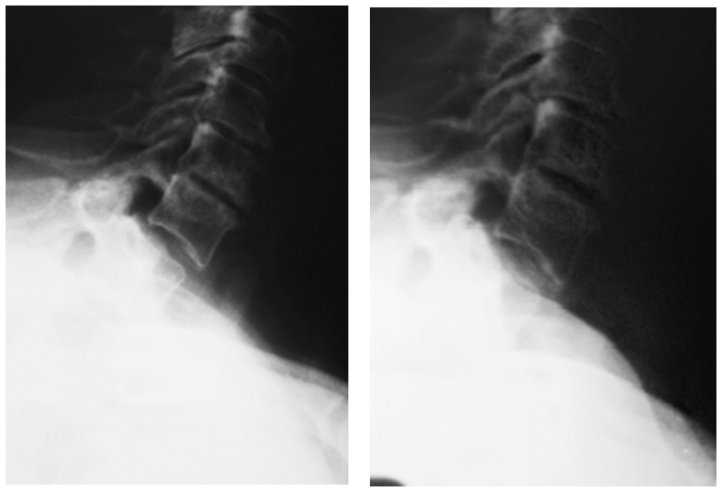
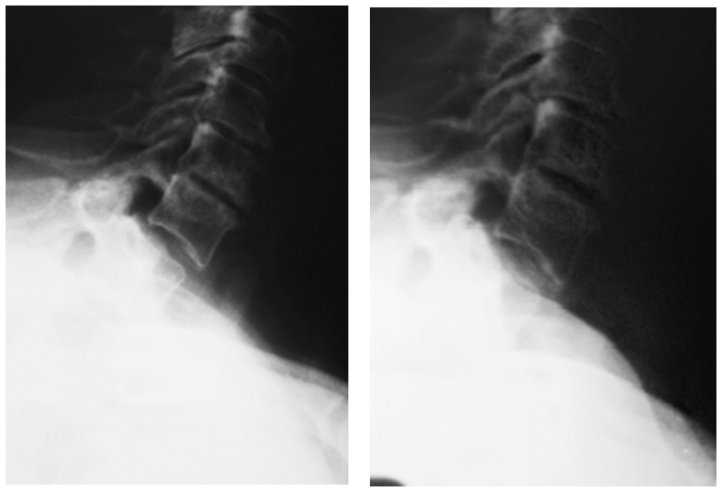
Figure 4: No evidence of instability on post-operative flexion/extension x-rays.
A 69-year-old woman presented with complaints of neck pain with bilateral radiation of pain and numbness to her shoulders, arms and hands; the pain was worse on the right. She also was having frequent headaches and stabbing pain, especially in her left occipital region. She complained of poor balance and frequent falls. The patient had undergone treatment by a chiropractor as well as cervical epidural steroid injections without much relief.
Physical exam showed decreased grip strength on the right. The left-handed patient gripped with 60 foot pounds on the left and 30 foot pounds on the right. She had a positive Hoffman on the left and an ataxic gait, but no pathologic reflexes or clonus.
MRI showed multiple levels of degenerative changes with some amount of collapsed disc throughout her cervical spine. She also had very small subluxations at C2/3 and C3/4. There was some element of spondylosis and facet hypertrophy at multiple levels, with mild foraminal stenosis and C4/5, C5/6, and C6/7. EMG of the right upper extremity showed a C8 radic ulopathy and no significant carpal tunnel syndrome. Myelogram CT scan was most remarkable for right C7-T1 neural impingement and cord deviation caused by an epidural mass, thought most likely to be a synovial cyst or atypical far-right lateral herniated disc. Other degenerative changes consistent with the MRI were noted, but the right-sided mass at C7/T1 was consistent with her C8 radiculopathy found on EMG.
The patient was treated with a right C7 laminotomy, T1 hemilaminectomy, and C7/T1 foraminotomy with resection of a synovial cyst. The facet was somewhat disrupted and the thecal sac was displaced from right to left. Pathology report measured the cyst at 2.0×1.8×0.3 cm. Postoperatively she was neurologically intact and by post-op day 1 she had improvement in her subjective right hand numbness.
By her final post-op visit at 5 months, after several months of physical therapy, she had no arm/hand numbness, equal and full upper extremity strength, increased range of motion in her neck, and mild upper neck pain which was dramatically better than prior to surgery.
This case report also demonstrates that when appropriate pre-op testing is done to assess stability, such as the flexion extension myelogram done here, that a C7-T1 synovial cyst can be approached safely and effectively by a unilateral posterior decompression and synovial cyst resection. Care should be taken to partially preserve the facet joint.
Synovial cysts are generally considered degenerative, but likely can have other causes such as trauma.6 They are not symptomatic unless they cause neural impingement, and can become symptomatic with structural changes in the spine.2 Cysts are the result of increased mobility but can contribute to joint disruption and pain.
A recent meta-analysis and case report indicated that patients treated with decompression and subaxial synovial cyst resection without fusion improved post-operative Nurick scores greater than patients who were also treated with fusion. For both groups the recurrence rate at time of report was 0%. However, the authors point out that a longer follow-up time could reveal other group difference with regard to recurrence and symptomatology.4 The literature is divided on whether a fusion is required after cyst resection with removal of all or a portion of a cervical lamina, particularly at C7/T1. It has been argued that because of the flexibility differences between the cervical and thoracic spine, that decompression at C7/T1 should include a fusion due to increased concern of instability.7 In the current case, the patient, a 69-year-old woman with multiple levels of cervical spine degenerative chances, present with both neck pain and radiculopathy. She had resolution of neurologic symptoms and nearcomplete resolution of neck pain after localized surgical resection without fusion, indicating that she had not become unstable at 5 months post-op (Figure 4).
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONSENT
Consent is not required for article publication, this article is a case report and not a study.