INTRODUCTION
During early embryonic development, the allantois forms as a vestigial membrane which originates from the cloaca and passes into the connecting yolk sac stalk. Between the 5th and 7th week gestation, the lower part of the allantois forms the bladder, and the intra-abdominal portion of the allantois evolves into the urachus which drains into the bladder.1 From the 32nd week gestation, descent of the bladder towards the pelvis stretches the urachus, causing its lumen to obliterate and transform into the median umbilical ligament. If this obliterative process is incomplete, this can lead to a persistently patent urachal remnant.2 This occurs in approximately 32% of the adult population and is most commonly located within the bladder dome, and may extend to the umbilicus.3 A patent urachus consists of an outer muscular layer and a lumen which is usually lined by urothelium with occasional foci of glandular metaplasia.4The exact course of a patent urachal remnant remains unknown; however, its persistence has shown to rarely undergo malignant transformation, accounting for 0.07-0.34% of all bladder carcinomas.5
Neoplasms of the urachus are predominantly glandular, and most are high grade invasive adenocarcinomas, representing 20-39% of bladder adenocarcinomas.6,7 In addition, there is a small subgroup of urachal glandular tumours that are cystic and have a striking resemblance to mucinous epithelial tumours of the ovary.8 Whilst these mucinous cystic tumours of the urachus have only been studied in case reports and small case series, its classification has been proposed by Amin et al and later modified in the WHO 2016 Classification of Tumours of the Urinary System and Male Genital Organs.8,9
In this report, we describe a rare case of a urachal mucinous cystic tumour of low malignant potential (MCTLMP) in a 59-year-old male, and aim to facilitate future interpretation and management of these tumours.
CASE REPORT
Patient and Diagnosis
A 59-year-old male presented to the Urology outpatients department in 2016 with mucinuria accompanied with persistent urinary frequency, urgency and cystitis. The patient was previously treated in the community with antibiotics for a presumed urinary tract infection and prostatitis, but no improvement was observed. Urine cultures and urethral swabs were negative for infection. The patient had a past surgical history of laparoscopic appendectomy for a histologically confirmed appendicitis in 2007.
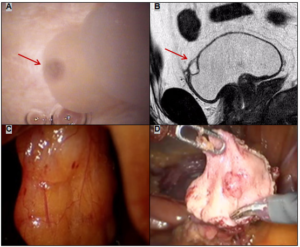
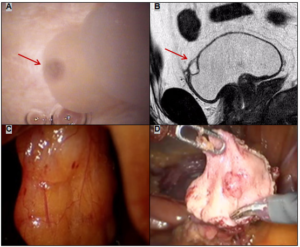
A flexible cystoscopy was performed and detected a discharging sinus at the dome of the bladder (Figure 1A). An ensuing magnetic resonance imaging (MRI) scan demonstrated a 17×15×9 mm thick walled septated cystic collection closely related to the anterio-superior bladder wall (Figure 1B), and a provisional diagnosis of a cystic urachal remnant was made.
Figure 1. Discharging Sinus at Dome of Bladder seen at Flexible Cystoscopy. B) MRI Image Demonstrating the Cystic and Septated Urachal Remnant. C) Intraoperative View of Urachal Remnant. D) Excision of the Urachal Remnant
Surgery and Follow-up
The patient underwent a partial cystectomy using a robotically assisted laparoscopic technique. A standard 4-port robotic approach was used, starting with dissection of the urachus from the umbilicus attachments and mobilising the remnant up to the dome of the bladder. A partial cystectomy was performed, excising a cuff of bladder around the urachal opening and cyst (Figure 1C and 1D). There was no evidence of pseudomyxoma peritoneii (PMP). At six months post-surgical follow up, the patient showed no clinical evidence of disease recurrence.
Pathology
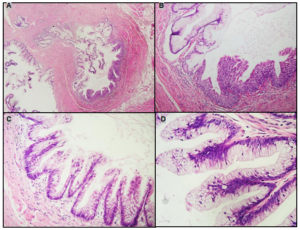
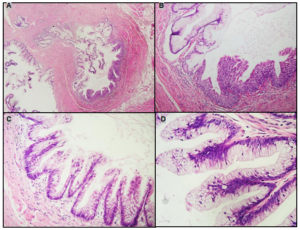
Grossly, the specimen showed no evidence of mucin extravasation. On dissection, a multiloculated mucin-filled cystic lesion was identified within the bladder wall, measuring 12 mm in size. The cyst showed no evidence of a solid component. Histologically, the cyst was predominantly lined by mucinous columnar epithelium and focally by transitional epithelium (Figure 2A and 2B). Areas of intestinal metaplasia were also noted (Figure 2C). The mucinous epithelium showed focal stratification and was thrown into papillary folds and tufts. Cytologically, the epithelial cells exhibited mild cytological atypia characterised by nuclear enlargement, hyperchromasia and pleomorphism (Figure 2D). Very occasional mitotic figures were identified. There was no evidence of intraepithelial carcinoma or stromal invasion. The overall constellation of features was in keeping with a urachal MCTLMP. The surgical resection margin was free of tumour.
Figure 2. Photomicrographs of the Urachal MCTLMP. (A) The Cystic Tumour was Lined by Mucinous Columnar Epithelium. (B) Abrupt Change into Transitional Epithelium was Noted. (C) Occasional Foci of Intestinal Metaplasia was Present. (D) Areas of Epithelial Tufting with Mild Cytological Atypia was also Identified
DISCUSSION
Urachal remnants are increasingly being discovered as an incidental finding with the use of cross sectional imaging. In particular, MRI is considered to be a highly specific and sensitive image modality for detection.10 Whilst they are often identified and managed in childhood, they can also present in adults. Many urachal remnants undergo spontaneous resolution, however, they are surgically resected in adults to avoid the potential risk of neoplastic transformation following chronic exposure to urinary stasis, inflammation and infection.11
Glandular tumours of the urachus can be classified into benign tumours, non-cystic adenocarcinoma and mucinous cystic tumours.3 The latter group has shown to exhibit morphological and immunohistochemical appearances very similar to mucinous tumours of the ovary. Based on this, Amin et al have classified mucinous cystic tumours of the urachus into the following categories: mucinous cystadenoma (no dysplasia), MCTLMP (mild to moderate cytological atypia with some mild architectural complexity), MCTLMP with intraepithelial carcinoma (focal severe cytological atypia with mitotic activity) and invasive mucinous cystadenocarcinoma (either minimal or frank invasion).8Subsequently, the WHO 2016 classification developed a revised categorisation of glandular neoplasms of the urachus, Table 1. The WHO 2016 also outlines criteria for the diagnosis of a urachal adenocarcinoma which was previously defined by Gopalan et al, Table 2.
| Table 1. WHO 2016 Classification of Glandular Neoplasms of the Urachus9 |
| Adenomas |
| Villous Adenoma |
| Mucinous cystadenoma ~ Cystic lesion lined by a single layer of mucinous columnar cells with no dysplasia. |
| Adenocarcinoma |
| Non-cystic Adenocarcinoma |
| Enteric (intestinal) adenocarcinoma ~ Tumour morphologically resembles colorectal adenocarcinoma |
| Mucinous colloid adenocarcinoma ~ Tumour contains cells with intracellular mucin alongside extracellular mucin pools. |
| Signet ring adenocarcinoma ~ Mucin filled tumour cells with potential to infiltrative in a diffuse manner. |
| Adenocarcinoma, NOS |
| Mixed Adenocarcinoma |
| Cystic Adenocarcinoma |
| Mucinous cystic tumours of low malignant potential (MCTLMP) ~ Epithelial cytological atypia range from low grade to intraepithelial carcinoma. |
| Mucinous cystadenocarcinoma ~ Tumour is either microinvasive (<2 mm invasion constituting <5% of the tumour) or frankly invasive. |
| Table 2. WHO 2016 Criteria for Urachal Adenocarcinoma9 |
| 1. Location of the tumour in the bladder dome and/or anterior wall. |
| 2. Epicenter of carcinoma in the bladder wall |
| 3. Absence of widespread cystitis cystica and/or cystitis glandularis beyond the dome or anterior wall. |
| 4. Absence of a known primary elsewhere. |
Urachal MCTLMP have had very limited review due to their rare incidence. 27 other cases have been reported in the English-language literature to date, in the form of case reports and a case series from 2012 to 2016.8,10,12,13,14,15 Overall, urachal MCTLMP have been reported in adults aged from to 26 to 80 years, with exception of only one case reported in a 15-year-old female.12 So far, they have been found to occur predominantly in female patients (60%). In 64% of cases, patients reported symptoms including the presence of an abdominal/pelvic mass (6 cases), abdominal pain (5 cases), mucinuria (3 cases), haematuria (2 cases) and umbilical discharge (1 case). The presence of umbilical discharge and mucinuria, in particular, are distinctive features of a persistent connection of the urachal remnant with the umbilicus and urinary bladder, respectively.10 In the remainder of cases, the tumour was detected incidentally via imaging. When the site of the tumour was recorded, they were mainly identified within the dome of the bladder, in keeping with the most common location for urachal remnants. In the majority of cases, the lesion was surgically removed via partial cystectomy with or without an umbilectomy and urachectomy. Macroscopically, the size of the tumour varied amongst reports, with a range of 8 mm to 80 mm and a median dimension of 45 mm.
In this case report, there was only mild epithelial dysplasia, and in a diagnosis of MCTLMP a range of epithelial abnormalities can be present from low grade atypia to intraepithelial carcinoma. The overall histological features documented amongst the MCTLMP case reports/series were extremely similar, with all cystic urachal lesions lined by mucinous columnar epithelium, with one case showing intestinal metaplasia.14In mostly all cases, the lining epithelium showed mild to moderate cytological atypia, demonstrated by slightly enlarged and hyperchromatic nuclei with pseudostratification by no more than three cell layers. Areas of epithelial proliferation were documented with a range of pseudopapillary, villous and tubulo-villous architectures.8 In addition, two cases demonstrated features of intraepithelial carcinoma.8 Stromal invasion was not present in any case, as this feature is incompatible with a diagnosis of MCTLMP and falls within the category of invasive mucinous cystadenocarcinoma.
The precise biological potential of urachal MCTLMP’s is not yet fully understood. It has been hypothesised that as in ovarian and appendiceal borderline tumours, MCTLMP may represent a precursor for mucinous cystadenocarcinoma.13 In addition, all mucinous tumours should be suspected of having an aggressive behaviour with development of PMP. Whilst there have been no reports of PMP in any case, mucin extravasation into the cyst wall was present in three cases of MCTLMP.10,13,15 We also note two reported cases of PMP arising from non-invasive urachal mucinous cystic tumours.16,17 Therefore, complete surgical excision and follow up with surveillance in all cases is advised. To date, all cases of MCTLMP have demonstrated a favourable prognosis, with no reports of recurrence, PMP or metastases during an intermediate follow-up period of 1 to 69 months.8
CONCLUSION
The categorisation of urachal glandular tumours first proposed by Amin et al, and modified by the WHO 2016 Classification offers a clear nomenclature of mucinous cystic tumours of the urachus. By utilising these schemes, we have described a rare case of a urachal MCTLMP, which is the first case to be reported in the United Kingdom, to our knowledge. Our evaluation of all reported cases of MCTLMP to date will hopefully aid future interpretation of these tumours.
ACKNOWLEDGEMENTS
Professor Clare Verrill’s and Dr Lisa Browning’s research time is part funded by the Oxford NIHR Biomedical Research Centre (Molecular Diagnostics Theme/Multimodal Pathology Subtheme).
CONFLICTS OF INTEREST
No potential conflicts of interest relevant to this article were reported.
CONSENT
The authors have received written informed consent from the patient.